Female Reproductive System Pathology Female Reproductive System Structure [Fig
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Reference Sheet 1
MALE SEXUAL SYSTEM 8 7 8 OJ 7 .£l"00\.....• ;:; ::>0\~ <Il '"~IQ)I"->. ~cru::>s ~ 6 5 bladder penis prostate gland 4 scrotum seminal vesicle testicle urethra vas deferens FEMALE SEXUAL SYSTEM 2 1 8 " \ 5 ... - ... j 4 labia \ ""\ bladderFallopian"k. "'"f"";".'''¥'&.tube\'WIT / I cervixt r r' \ \ clitorisurethrauterus 7 \ ~~ ;~f4f~ ~:iJ 3 ovaryvagina / ~ 2 / \ \\"- 9 6 adapted from F.L.A.S.H. Reproductive System Reference Sheet 3: GLOSSARY Anus – The opening in the buttocks from which bowel movements come when a person goes to the bathroom. It is part of the digestive system; it gets rid of body wastes. Buttocks – The medical word for a person’s “bottom” or “rear end.” Cervix – The opening of the uterus into the vagina. Circumcision – An operation to remove the foreskin from the penis. Cowper’s Glands – Glands on either side of the urethra that make a discharge which lines the urethra when a man gets an erection, making it less acid-like to protect the sperm. Clitoris – The part of the female genitals that’s full of nerves and becomes erect. It has a glans and a shaft like the penis, but only its glans is on the out side of the body, and it’s much smaller. Discharge – Liquid. Urine and semen are kinds of discharge, but the word is usually used to describe either the normal wetness of the vagina or the abnormal wetness that may come from an infection in the penis or vagina. Duct – Tube, the fallopian tubes may be called oviducts, because they are the path for an ovum. -

Ovarian Cancer and Cervical Cancer
What Every Woman Should Know About Gynecologic Cancer R. Kevin Reynolds, MD The George W. Morley Professor & Chief, Division of Gyn Oncology University of Michigan Ann Arbor, MI What is gynecologic cancer? Cancer is a disease where cells grow and spread without control. Gynecologic cancers begin in the female reproductive organs. The most common gynecologic cancers are endometrial cancer, ovarian cancer and cervical cancer. Less common gynecologic cancers involve vulva, Fallopian tube, uterine wall (sarcoma), vagina, and placenta (pregnancy tissue: molar pregnancy). Ovary Uterus Endometrium Cervix Vagina Vulva What causes endometrial cancer? Endometrial cancer is the most common gynecologic cancer: one out of every 40 women will develop endometrial cancer. It is caused by too much estrogen, a hormone normally present in women. The most common cause of the excess estrogen is being overweight: fat cells actually produce estrogen. Another cause of excess estrogen is medication such as tamoxifen (often prescribed for breast cancer treatment) or some forms of prescribed estrogen hormone therapy (unopposed estrogen). How is endometrial cancer detected? Almost all endometrial cancer is detected when a woman notices vaginal bleeding after her menopause or irregular bleeding before her menopause. If bleeding occurs, a woman should contact her doctor so that appropriate testing can be performed. This usually includes an endometrial biopsy, a brief, slightly crampy test, performed in the office. Fortunately, most endometrial cancers are detected before spread to other parts of the body occurs Is endometrial cancer treatable? Yes! Most women with endometrial cancer will undergo surgery including hysterectomy (removal of the uterus) in addition to removal of ovaries and lymph nodes. -

Differential Studies of Ovarian Endometriosis Cells from Endometrium Or Oviduct
European Review for Medical and Pharmacological Sciences 2016; 20: 2769-2772 Differential studies of ovarian endometriosis cells from endometrium or oviduct W. LIU1,2, H.-Y. WANG3 1Reproductive Center, the First Affiliated Hospital of Anhui Medical University, Hefei, Anhui, China 2Department of Obstetrics and Gynecology, the Second Affiliated Hospital of Medical University of Anhui, Hefei, Anhui, China 3Department of Gynecologic Oncology, Anhui Provincial Cancer Hospital, the West Branch of Anhui Provincial Hospital, Hefei, Anhui, China Abstract. – OBJECTIVE: To study the promi- In most cases, EMT affects ovary and peritone- nent differences between endometriosis (EMT) um, and as a result a plump shape cyst forms in cells derived from ovary, oviduct and endometri- the ovary. The cyst is called ovarian endometrio- um, and to provided new ideas about the patho- sis cyst (aka ovarian chocolate cyst) which usually genesis of endometriosis. PATIENTS AND METHODS: contains old blood and is covered by endometrioid From June 2010 1 to June 2015, 210 patients diagnosed with en- epithelium. In 1860, Karl von Rokitansky studied dometriosis were enrolled in our study. Patients the disease and observed retrograde menstruation were treated by laparoscopy or conventional in nearly 90% of child-bearing women, and later surgeries in our hospital. Ovarian chocolate proposed “retrograde menstruation implantation cyst and paired normal ovarian tissues, fimbri- theory”. However, this theory explained endo- ated extremity of fallopian and uterine cavity en- metriosis in the abdominopelvic cavity does not domembrane tissues were collected, prepared 2 and observed by microscope. PCR was used for explain endometriosis outside of enterocelia . Lat- 3 4 amplification of target genes (FMO3 and HOXA9) er on, Iwanoff and Meyer proposed “coelomic and Western blot was used to evaluate FMO3 metaplasia theory” which stipulated that endome- and HOXA9 expression levels. -
Echography of the Cervix and Uterus During the Proliferative and Secretory Phases of the Menstrual Cycle in Bonnet Monkeys (Macaca Radiata)
Journal of the American Association for Laboratory Animal Science Vol 53, No 1 Copyright 2014 January 2014 by the American Association for Laboratory Animal Science Pages 18–23 Echography of the Cervix and Uterus during the Proliferative and Secretory Phases of the Menstrual Cycle in Bonnet Monkeys (Macaca radiata) Uddhav K Chaudhari,1,* Siddnath M Metkari,2 Dhyananjay D Manjaramkar,2 Geetanjali Sachdeva,1 Rajendra Katkam,1 Atmaram H Bandivdekar,3 Abhishek Mahajan,4 Meenakshi H Thakur,4 and Sanjiv D Kholkute1 We undertook the present study to investigate the echographic characteristics of the uterus and cervix of female bonnet monkeys (Macaca radiata) during the proliferative and secretory phases of the menstrual cycle. The cervix was tortuous in shape and measured 2.74 ± 0.30 cm (mean ± SD) in width by 3.10 ± 0.32 cm in length. The cervical lumen contained 2 or 3 col- liculi, which projected from the cervical canal. The echogenicity of cervix varied during proliferative and secretory phases. The uterus was pyriform in shape (2.46 ± 0.28 cm × 1.45 ± 0.19 cm) and consisted of serosa, myometrium, and endometrium. The endometrium generated a triple-line pattern; the outer and central lines were hyperechogenic, whereas the inner line was hypoechogenic. The endometrium was significantly thicker during the secretory phase (0.69 ± 0.12 cm) than during the proliferative phase (0.43 ± 0.15 cm). Knowledge of the echogenic changes in the female reproductive organs of bonnet monkeys during a regular menstrual cycle may facilitate understanding of other physiologic and pathophysiologic changes. Ultrasound imaging is a noninvasive, atraumatic, and simple Materials and Methods method to assess various organs in humans and nonhuman pri- Animals and husbandry practices. -

The Cyclist's Vulva
The Cyclist’s Vulva Dr. Chimsom T. Oleka, MD FACOG Board Certified OBGYN Fellowship Trained Pediatric and Adolescent Gynecologist National Medical Network –USOPC Houston, TX DEPARTMENT NAME DISCLOSURES None [email protected] DEPARTMENT NAME PRONOUNS The use of “female” and “woman” in this talk, as well as in the highlighted studies refer to cis gender females with vulvas DEPARTMENT NAME GOALS To highlight an issue To discuss why this issue matters To inspire future research and exploration To normalize the conversation DEPARTMENT NAME The consensus is that when you first start cycling on your good‐as‐new, unbruised foof, it is going to hurt. After a “breaking‐in” period, the pain‐to‐numbness ratio becomes favourable. As long as you protect against infection, wear padded shorts with a generous layer of chamois cream, no underwear and make regular offerings to the ingrown hair goddess, things are manageable. This is wrong. Hannah Dines British T2 trike rider who competed at the 2016 Summer Paralympics DEPARTMENT NAME MY INTRODUCTION TO CYCLING Childhood Adolescence Adult Life DEPARTMENT NAME THE CYCLIST’S VULVA The Issue Vulva Anatomy Vulva Trauma Prevention DEPARTMENT NAME CYCLING HAS POSITIVE BENEFITS Popular Means of Exercise Has gained popularity among Ideal nonimpact women in the past aerobic exercise decade Increases Lowers all cause cardiorespiratory mortality risks fitness DEPARTMENT NAME Hermans TJN, Wijn RPWF, Winkens B, et al. Urogenital and Sexual complaints in female club cyclists‐a cross‐sectional study. J Sex Med 2016 CYCLING ALSO PREDISPOSES TO VULVAR TRAUMA • Significant decreases in pudendal nerve sensory function in women cyclists • Similar to men, women cyclists suffer from compression injuries that compromise normal function of the main neurovascular bundle of the vulva • Buller et al. -

Pregnancy and Cesarean Delivery After Multimodal Therapy for Vulvar Carcinoma: a Case Report
MOLECULAR AND CLINICAL ONCOLOGY 5: 583-586, 2016 Pregnancy and cesarean delivery after multimodal therapy for vulvar carcinoma: A case report KUNIAKI TORIYABE1,2, HARUKI TANIGUCHI2, TOKIHIRO SENDA2,3, MASAKO NAKANO2, YOSHINARI KOBAYASHI2, MIHO IZAWA2, HIROHIKO TANAKA2, TETSUO ASAKURA2, TSUTOMU TABATA1 and TOMOAKI IKEDA1 1Department of Obstetrics and Gynecology, Mie University Graduate School of Medicine, Tsu, Mie 514-8507; 2Department of Obstetrics and Gynecology, Mie Prefectural General Medical Center, Yokkaichi, Mie 510-8561; 3Department of Obstetrics and Gynecology, Kinan Hospital, Mihama, Mie 519-5293, Japan Received November 4, 2015; Accepted September 12, 2016 DOI: 10.3892/mco.2016.1021 Abstract. Reports of pregnancy following treatment for vulvectomy, may have an increased incidence of caesarean vulvar carcinoma are extremely uncommon, as the main delivery (2). In the literature, vulvar scarring following radical problem of subsequent pregnancy is vulvar scarring following vulvectomy was the major reason for pregnant women under- radical surgery. We herein report the case of a patient who was going caesarean section (2-7). To date, no cases of pregnancy diagnosed with stage I squamous cell carcinoma of the vulva following vulvar carcinoma have been reported in patients at the age of 17 years and was treated with multimodal therapy, who had undergone surgery and radiotherapy. including neoadjuvant chemotherapy, wide local excision with We herein describe a case in which caesarean section was bilateral inguinal lymph node dissection and adjuvant radio- performed due to the presence of extensive vulvar scarring therapy. The patient became pregnant spontaneously 9 years following multimodal therapy for vulvar carcinoma, including after her initial diagnosis and the antenatal course was good, chemotherapy, surgery and radiotherapy. -
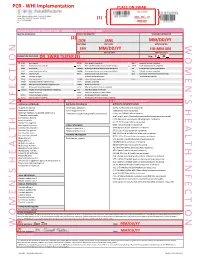
Womens Health Requisition Forms
PCR - WHI Implementation PLACE ON SWAB 10854 Midwest Industrial Blvd. St. Louis, MO 63132 MM DD YY Phone: (314) 200-3040 | Fax (314) 200-3042 (1) CLIA ID #26D0953866 JANE DOE v3 PCR MOLECULAR REQUISITION - WOMEN'S HEALTH INFECTION PRACTICE INFORMATION PATIENT INFORMATION *SPECIMEN INFORMATION (2) DOE JANE MM/DD/YY LAST NAME FIRST NAME DATE COLLECTED W O M E ' N S H E A L T H I F N E C T I O N SSN MM/DD/YY HH:MM AM SSN DATE OF BIRTH TIME COLLECTED REQUESTING PHYSICIAN: DR. SWAB TESTER (3) Sex: F X M (4) Diagnosis Codes X N76.0 Acute vaginitis B37.49 Other urogenital candidiasis A54.9 Gonococcal infection, unspecified N76.1 Subacute and chronic vaginitis N89.8 Other specified noninflammatory disorders of vagina A59.00 Urogenital trichomoniasis, unspecified N76.2 Acute vulvitis O99.820 Streptococcus B carrier state complicating pregnancy A64 Unspecified sexually transmitted disease N76.3 Subacute and chronic vulvitis O99.824 Streptococcus B carrier state complicating childbirth A74.9 Chlamydial infection, unspecified N76.4 Abscess of vulva B95.1 Streptococcus, group B, as the cause Z11.3 Screening for infections with a predmoninantly N76.5 Ulceration of vagina of diseases classified elsewhere sexual mode of trasmission N76.6 Ulceration of vulva Z22.330 Carrier of group B streptococcus Other: N76.81 Mucositis(ulcerative) of vagina and vulva N70.91 Salpingitis, unspecified N76.89 Other specified inflammation of vagina and vulva N70.92 Oophoritis, unspecified N95.2 Post menopausal atrophic vaginitis N71.9 Inflammatory disease of uterus, unspecified -

Female Perineum Doctors Notes Notes/Extra Explanation Please View Our Editing File Before Studying This Lecture to Check for Any Changes
Color Code Important Female Perineum Doctors Notes Notes/Extra explanation Please view our Editing File before studying this lecture to check for any changes. Objectives At the end of the lecture, the student should be able to describe the: ✓ Boundaries of the perineum. ✓ Division of perineum into two triangles. ✓ Boundaries & Contents of anal & urogenital triangles. ✓ Lower part of Anal canal. ✓ Boundaries & contents of Ischiorectal fossa. ✓ Innervation, Blood supply and lymphatic drainage of perineum. Lecture Outline ‰ Introduction: • The trunk is divided into 4 main cavities: thoracic, abdominal, pelvic, and perineal. (see image 1) • The pelvis has an inlet and an outlet. (see image 2) The lowest part of the pelvic outlet is the perineum. • The perineum is separated from the pelvic cavity superiorly by the pelvic floor. • The pelvic floor or pelvic diaphragm is composed of muscle fibers of the levator ani, the coccygeus muscle, and associated connective tissue. (see image 3) We will talk about them more in the next lecture. Image (1) Image (2) Image (3) Note: this image is seen from ABOVE Perineum (In this lecture the boundaries and relations are important) o Perineum is the region of the body below the pelvic diaphragm (The outlet of the pelvis) o It is a diamond shaped area between the thighs. Boundaries: (these are the external or surface boundaries) Anteriorly Laterally Posteriorly Medial surfaces of Intergluteal folds Mons pubis the thighs or cleft Contents: 1. Lower ends of urethra, vagina & anal canal 2. External genitalia 3. Perineal body & Anococcygeal body Extra (we will now talk about these in the next slides) Perineum Extra explanation: The perineal body is an irregular Perineal body fibromuscular mass. -

Polycystic Ovary Syndrome.Pdf
Female reproductive system diseases Polycystic ovary syndrome Introduction: Polycystic ovary syndrome is one of the most common hormonal disorders among women. The name of this condition comes from the cysts that develop when ovulation vesicles get trapped under the surface of the ovaries preventing them from releasing the eggs. Cause: Normally, the pituitary gland in the brain secretes hormones (FSH) and (LH), that are responsible for controlling ovulation, while the ovary secretes estrogen and progesterone hormones, which prepare the uterus for the egg. The ovary also secretes the male hormone (androgen). However, in the case of polycystic ovary syndrome, the pituitary gland secretes excess amounts of (LH) and the ovary secretes excess amounts of the male hormone (androgen), resulting in irregular menstrual cycles and difficulties conceiving, as well as an increase facial hair and acne. There are many factors that may play a role in causing polycystic ovary syndrome: • Increased resistance to insulin (high blood glucose levels). • Heredity Symptoms: • Menstrual cycle abnormalities: The duration of the menstrual cycle may be prolonged to 35 days, or it could become less frequent occurring less than 8 times a year or it could be completely absent. • Increased body and facial hair • Acne • Obesity • Difficulty conceiving Diagnosis: • Medical history: Absence of the menstrual cycle - increased facial and body hair - acne - excess weight. • Ultrasound examination: of the uterus and ovaries • Blood test: To measure hormone levels, especially androgens and (LH). Treatment: Treatment depends on the symptoms regardless of whether the woman wants to conceive or not: • Lifestyle changes: This includes following a low-carb diet that is rich in grains, vegetables, fruits and small amounts of meat. -

The Discovery of Different Types of Cervical Mucus and the Billings Ovulation Method
The Discovery of Different Types of Cervical Mucus and the Billings Ovulation Method Erik Odeblad Emeritus Professor, Dept. of Medical Biophysics, University of Umeå, Sweden Published with permission from the Bulletin of the Ovulation Method Research and Reference Centre of Australia, 27 Alexandra Parade, North Fitzroy, Victoria 3068, Australia, Volume 21, Number 3, pages 3-35, September 1994. Copyright © Ovulation Method Research and Reference Centre of Australia 1. Abstract 2. Introduction 3. Anatomy and Physiology 4. What is Mucus? 5. The Commencement of my Research 6. The Existence of Different Types of Crypts and of Mucus 7. Identification and Description of G, L, and S Mucus 8. G- and G+ Mucus 9. Age, Pregnancy, the Pill and Microsurgery 10. P Mucus 11. F Mucus 12. The Role of the Vagina 13. The Different Types of Secretions and the Billings Ovulation Method 14. Early Infertile Days 15. The Days of Possible Fertility 16. Late Infertile Days 17. Anovulatory Cycles 18. Lactation 19. Diseases and the Billings Ovulation Method 20. The Future 21. Acknowledgements 22. Author's Note 23. References 24. Appendix Abstract An introduction to and some new anatomical and physiological aspects of the cervix and vagina are presented and also an explanation of the biosynthesis and molecular structure of mucus. The history of my discoveries of the different types of cervical mucus is given. In considering my microbiological investigations I suspected the existence of different types of crypts and cervical mucus and in 1959 1 proved the existence of these different types. The method of examining viscosity by nuclear magnetic resonance was applied to microsamples of mucus extracted 1 outside of several crypts. -

Women's Menstrual Cycles
1 Women’s Menstrual Cycles About once each month during her reproductive years, a woman has a few days when a bloody fluid leaves her womb and passes through her vagina and out of her body. This normal monthly bleeding is called menstruation, or a menstrual period. Because the same pattern happens each month, it is called the menstrual cycle. Most women bleed every 28 days. But some bleed as often as every 20 days or as seldom as every 45 days. Uterus (womb) A woman’s ovaries release an egg once a month. If it is Ovary fertilized she may become pregnant. If not, her monthly bleeding will happen. Vagina Menstruation is a normal part of women’s lives. Knowing how the menstrual cycle affects the body and the ways menstruation changes over a woman’s lifetime can let you know when you are pregnant, and help you detect and prevent health problems. Also, many family planning methods work best when women and men know more about the menstrual cycle (see Family Planning). 17 December 2015 NEW WHERE THERE IS NO DOCTOR: ADVANCE CHAPTERS 2 CHAPTER 24: WOMEN’S MENSTRUAL CYCLES Hormones and the menstrual cycle In women, the hormones estrogen and progesterone are produced mostly in the ovaries, and the amount of each one changes throughout the monthly cycle. During the first half of the cycle, the ovaries make mostly estrogen, which causes the lining of the womb to thicken with blood and tissue. The body makes the lining so a baby would have a soft nest to grow in if the woman became pregnant that month. -

Luteal Phase Deficiency: What We Now Know
■ OBGMANAGEMENT BY LAWRENCE ENGMAN, MD, and ANTHONY A. LUCIANO, MD Luteal phase deficiency: What we now know Disagreement about the cause, true incidence, and diagnostic criteria of this condition makes evaluation and management difficult. Here, 2 physicians dissect the data and offer an algorithm of assessment and treatment. espite scanty and controversial sup- difficult to definitively diagnose the deficien- porting evidence, evaluation of cy or determine its incidence. Further, while Dpatients with infertility or recurrent reasonable consensus exists that endometrial pregnancy loss for possible luteal phase defi- biopsy is the most reliable diagnostic tool, ciency (LPD) is firmly established in clinical concerns remain about its timing, repetition, practice. In this article, we examine the data and interpretation. and offer our perspective on the role of LPD in assessing and managing couples with A defect of corpus luteum reproductive disorders (FIGURE 1). progesterone output? PD is defined as endometrial histology Many areas of controversy Linconsistent with the chronological date of lthough observational and retrospective the menstrual cycle, based on the woman’s Astudies have reported a higher incidence of LPD in women with infertility and recurrent KEY POINTS 1-4 pregnancy losses than in fertile controls, no ■ Luteal phase deficiency (LPD), defined as prospective study has confirmed these find- endometrial histology inconsistent with the ings. Furthermore, studies have failed to con- chronological date of the menstrual cycle, may be firm the superiority of any particular therapy. caused by deficient progesterone secretion from the corpus luteum or failure of the endometrium Once considered an important cause of to respond appropriately to ovarian steroids.