Making Abortions Safe: a Matter of Good Public Health Policy and Practice M
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Snapshot of the Status of Women in Brazil 2019
A SNAPSHOT OF THE STATUS OF WOMEN IN BRAZIL 2019 A Snapshot of the Status of Women in Brazil: 2019 Edited by Anna Prusa and Lara Picanço Brazil Institute | Wilson Center Washington, DC © Woodrow Wilson Interantional Center for Scholars 2019 TABLE OF CONTENTS 3 Letter from the Editors Anna Prusa and Lara Picanço 6 Stuck in the Middle: Gender Violence Alison Brysk 8 Maternal Health: Persistent Challenges Continue to Endanger Women’s Lives Sarah B. Barnes 12 Women in Politics Malu A. C. Gatto 16 A View from the Private Sector: Closing Our Gender Gap at Azul Carolyn Trabuco 18 Women in Science: Still Invisible? Fernanda De Negri 20 Women in the Fight Against Corruption Tiffany D. Barnes 24 Gender Equity on the Bench and Before the Law Tainá Machado de Almeida Castro 28 Contemporary Racism, Sexism, and Slave Labor Mércia Consolação Silva 32 Women in Combat: The Long Path Toward Integration in the Armed Forces Lívia Peres Milani 34 On the Margins: Black Women, Public Policies, and Black Feminism Claudielle Pavão da Silva Letter from the Editors Anna Prusa & Lara Picanço The status of women in Brazil is emblematic of the country’s internal tensions. Brazil is a country where a woman can become president; yet it also has one of the highest rates of femicide—the killing of women due to their gender—in the world.1 The 2018 elections underscored the growing polarization of this issue in Brazil. Even as a record number of women ran for office and won seats at all levels of government, the election also ushered in a far more conservative administration that has sought to reinforce traditional gender roles. -

Forced Abortion in China PRI Staff / November 1, 2001
UNFPA Whitewash: Forced Abortion in China PRI Staff / November 1, 2001 Population Research Institute (PRI) has obtained a copy of a letter sent from the Executive Director of the United Nations Population Fund (UNFPA), Thoraya Ahmed Obaid, to the US Secretary of State, Colin L. Powell. The letter, dated 19 November 2001, falsely claims that information presented by PRI to members of the US Congress regarding UNFPA-supported abuses in China is untrue.1 Visit to China PRI investigators this September visited a county in Southern China where UNFPA claims coercion does not exist. In Sihui county, Guangdong province, they obtained testimony from victims of a UNFPA-funded family planning program who had suffered forced abortion, forced sterilization and destruction of homes and property at the hands of local officials. They presented this evidence at an October 17 hearing of the House International Relations Committee, along with further evidence linking these abuses to the UNFPA. In their opinion, based on interviews with two dozen women, coercion in Sihui county is as bad today as it ever has been. The UNFPA sought to counter PRI’s on-the-ground investigation of UNFPA-funded family planning programs by carrying out its own in-house review. A delegation of UNFPA employees and associates was hastily organized and sent to China in October. The seven- and-a-half page “mission report” produced by that delegation describes visits with Chinese officials in Beijing, Guangzhou, Sihui county, and Hubei Province, all of whom — not surprisingly — denied -

Brazilian Supreme Court Decides Cases En Banc Or by One of Its Two Panels Or Chambers
[. Below is the chamber’s 3 x 2 majority opinion, authored by its president, Justice Barroso.] WRIT OF HABEAS CORPUS 124.306 RIO DE JANEIRO STATE1 ORIGINAL RAPPORTEUR: JUSTICE MARCO AURÉLIO RAPPORTEUR FOR THE MAJORITY OPINION: JUSTICE LUÍS ROBERTO BARROSO DEFENDANT(S): EDILSON DOS SANTOS DEFENDANT(S): ROSEMERE APARECIDA FERREIRA PETITIONER(S): JAIR LEITE PEREIRA RESPONDENT(S) AUTHORITY(IES): SUPERIOR COURT OF JUSTICE MAJORITY OPINION2 JUSTICE LUÍS ROBERTO BARROSO: Syllabus: CRIMINAL PROCEDURE. WRIT OF HABEAS CORPUS. PRETRIAL DETENTION. ABSENCE OF LEGAL REQUIREMENTS FOR ITS DECREE. UNCONSTITUTIONALITY OF THE INCIDENCE OF THE PENAL OFFENCE OF ABORTION IN CASE OF VOLUNTARY TERMINATION OF PREGNANCY DURING THE FIRST TRIMESTER. RELEASE FROM CUSTODY. ORDER GRANTED “EX OFFICIO”. 1. The writ of habeas corpus is not applicable to the case at bar. However, the situation demands that the order be granted “ex officio” on two grounds, for the purpose of releasing the defendants from pretrial detention. 2. First, the original pretrial detention does not meet the legal requirements for the measure, namely: risks to public order, economic order, the criminal investigation or the enforcement of criminal law (article 312 of the Criminal Procedure Code). The 1 The English version of this opinion was edited by Sara Huddleston and revised by Professor Paulo Barrozo, Associate Professor at Boston College Law School. 2 The Brazilian Supreme Court decides cases en banc or by one of its two panels or chambers. Five justices compose each chamber. Although Justice Luís Roberto Barroso was not the original justice-rapporteur in this case, his opinion was joined by the majority of the First Chamber. -

The Epidemiology of Abortion and Its Prevention in Chile, 79(5) Rev
Gene Gene Start Gene End Motif Start Motif End Motif Strand Exon Start Exon End HS Start HS End Distance NLGN4X 5808082 6146706 5821352 5821364 gtggccacggcgg ‑ 5821117 5821907 5811910 5813910 7442 AFF2 147582138 148082193 148048477 148048489 ccaccatcacctc + 148048319 148048609 148036319 148040319 8158 NLGN3 70364680 70391051 70386983 70386995 gtggatatggtgg + 70386860 70387650 70371089 70377089 9894 MECP2 153287263 153363188 153296166 153296178 gtggtgatggtgg ‑ 153295685 153296901 153306976 153308976 10798 FRMPD4 12156584 12742642 12739916 12739928 ccaccatggccgc + 12738647 12742642 12721454 12727454 12462 PHF8 53963112 54071569 54012352 54012364 ccaccatgtcctc ‑ 54012339 54012382 54025089 54033089 12725 RAB39B 154487525 154493852 154493567 154493579 cctccatggccgc ‑ 154493358 154493852 154478566 154480566 13001 FRMPD4 12156584 12742642 12736309 12736321 ggggcaagggagg + 12735619 12736909 12721454 12727454 14867 GRPR 16141423 16171641 16170710 16170722 cctccgtggccac + 16170378 16171641 16208454 16211454 37732 AFF2 147582138 148082193 148079262 148079274 cccccgtcaccac + 148072740 148082193 148036319 148040319 38943 SH3KBP1 19552082 19905744 19564111 19564123 cctccttatcctc ‑ 19564039 19564168 19610454 19614454 46331 PDZD4 153067622 153096003 153070331 153070343 cccccttctcctc ‑ 153067622 153070355 153013976 153018976 51355 SLC6A8 152953751 152962048 152960611 152960623 ccaccctgacccc + 152960528 152962048 153013976 153018976 53353 FMR1 146993468 147032647 147026533 147026545 gaggacaaggagg + 147026463 147026571 147083193 147085193 56648 HNRNPH2 -
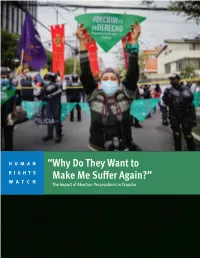
“Why Do They Want to Make Me Suffer Again?” the Impact of Abortion Prosecutions in Ecuador
HUMAN “Why Do They Want to RIGHTS WATCH Make Me Suffer Again?” The Impact of Abortion Prosecutions in Ecuador “Why Do They Want to Make Me Suffer Again?” The Impact of Abortion Prosecutions in Ecuador Copyright © 2021 Human Rights Watch All rights reserved. Printed in the United States of America ISBN: 978-1-62313-919-3 Cover design by Rafael Jimenez Human Rights Watch defends the rights of people worldwide. We scrupulously investigate abuses, expose the facts widely, and pressure those with power to respect rights and secure justice. Human Rights Watch is an independent, international organization that works as part of a vibrant movement to uphold human dignity and advance the cause of human rights for all. Human Rights Watch is an international organization with staff in more than 40 countries, and offices in Amsterdam, Beirut, Berlin, Brussels, Chicago, Geneva, Goma, Johannesburg, London, Los Angeles, Moscow, Nairobi, New York, Paris, San Francisco, Sydney, Tokyo, Toronto, Tunis, Washington DC, and Zurich. For more information, please visit our website: http://www.hrw.org JULY 2021 ISBN: 978-1-62313-919-3 “Why Do They Want to Make Me Suffer Again?” The Impact of Abortion Prosecutions in Ecuador Summary ........................................................................................................................... 1 Key Recommendations ....................................................................................................... 8 To the Presidency ................................................................................................................... -

Abortion Rates
MEASURE DHS assists countries worldwide in the collection and use of data to monitor and evaluate population, health, and nutrition programs. Funded by the U.S. Agency for International Development (USAID), MEASURE DHS is implemented by ORC Macro in Calverton, Maryland. The main objectives of the MEASURE DHS project are: 1) to provide decisionmakers in survey countries with information useful for informed policy choices, 2) to expand the international population and health database, 3) to advance survey methodology, and 4) to develop in participating countries the skills and resources necessary to conduct high-quality demographic and health surveys. Information about the MEASURE DHS project or the status of MEASURE DHS surveys is available on the Internet at http://www.measuredhs.com or by contacting: ORC Macro 11785 Beltsville Drive, Suite 300 Calverton, MD 20705 USA Telephone: 301-572-0200 Fax: 301-572-0999 E-mail: [email protected] DHS Analytical Studies No. 8 Recent Trends in Abortion and Contraception in 12 Countries Charles F. Westoff Office of Population Research Princeton University ORC Macro Calverton, Maryland, USA February 2005 This publication was made possible through support provided by the U.S. Agency for Interna- tional Development under the terms of Contract No. HRN-C-00-97-00019-00. The opinions expressed herein are those of the authors and do not necessarily reflect the views of the U.S. Agency for International Development Suggested citation: Westoff, Charles F. 2005. Recent Trends in Abortion and Contraception -

Induced Abortion in Chile
In Brief Induced Abortion in Chile Chile is one of a small handful of countries worldwide that Abortion-related deaths and injuries appear to have declined dramatically prohibit induced abortion under any circumstance, including In the 1960s, many Chilean women if a woman’s life is at risk. The longstanding ban, which undergoing unsafe abortions died as a result, or suffered serious short- or long- runs counter to Chile’s stated commitment to international term health complications for which they women’s rights treaties, faces a robust challenge in the did not receive the medical treatment they needed.9 In 1960, there were 294 form of a recent bill proposed by the government of maternal deaths per 100,000 live births,10 and one-third of these deaths were at- President Bachelet that would allow the procedure under tributable to unsafe abortion.11 One in limited circumstances. Yet informed debate on the topic is five hospital beds in obstetric depart- ments were occupied by women receiving hindered by the lack of data on the incidence and context of postabortion treatment. clandestine induced abortion. Chile’s maternal mortality ratio fell to 55 deaths per 100,000 live births by In every country, regardless of the legal No data exist on the characteristics of 1990, and to 22 by 2013.12 The precise status of induced abortion, some women women obtaining abortions in Chile, nor contribution of unsafe induced abortion experiencing an unintended pregnancy on their reasons for doing so. As one to overall maternal mortality is unclear, turn to abortion to end it.1 Chile is no researcher points out, “we do not know… but experts agree that far fewer deaths exception to this worldwide pattern. -

Medical Abortion Reference Guide INDUCED ABORTION and POSTABORTION CARE at OR AFTER 13 WEEKS GESTATION (‘SECOND TRIMESTER’) © 2017, 2018 Ipas
Medical Abortion Reference Guide INDUCED ABORTION AND POSTABORTION CARE AT OR AFTER 13 WEEKS GESTATION (‘SECOND TRIMESTER’) © 2017, 2018 Ipas ISBN: 1-933095-97-0 Citation: Edelman, A. & Mark, A. (2018). Medical Abortion Reference Guide: Induced abortion and postabortion care at or after 13 weeks gestation (‘second trimester’). Chapel Hill, NC: Ipas. Ipas works globally so that women and girls have improved sexual and reproductive health and rights through enhanced access to and use of safe abortion and contraceptive care. We believe in a world where every woman and girl has the right and ability to determine her own sexuality and reproductive health. Ipas is a registered 501(c)(3) nonprofit organization. All contributions to Ipas are tax deductible to the full extent allowed by law. For more information or to donate to Ipas: Ipas P.O. Box 9990 Chapel Hill, NC 27515 USA 1-919-967-7052 [email protected] www.ipas.org Cover photo: © Ipas The photographs used in this publication are for illustrative purposes only; they do not imply any particular attitudes, behaviors, or actions on the part of any person who appears in the photographs. Printed on recycled paper. Medical Abortion Reference Guide INDUCED ABORTION AND POSTABORTION CARE AT OR AFTER 13 WEEKS GESTATION (‘SECOND TRIMESTER’) Alison Edelman Senior Clinical Consultant, Ipas Professor, OB/GYN Oregon Health & Science University Alice Mark Associate Medical Director National Abortion Federation About Ipas Ipas works globally so that women and girls have improved sexual and reproductive health and rights through enhanced access to and use of safe abortion and contraceptive care. -

A Qualitative Examination of Women's Abortion Experiences
University of New Hampshire University of New Hampshire Scholars' Repository Master's Theses and Capstones Student Scholarship Fall 2006 Talking about abortion: A qualitative examination of women's abortion experiences Diana L. Dumais University of New Hampshire, Durham Follow this and additional works at: https://scholars.unh.edu/thesis Recommended Citation Dumais, Diana L., "Talking about abortion: A qualitative examination of women's abortion experiences" (2006). Master's Theses and Capstones. 27. https://scholars.unh.edu/thesis/27 This Thesis is brought to you for free and open access by the Student Scholarship at University of New Hampshire Scholars' Repository. It has been accepted for inclusion in Master's Theses and Capstones by an authorized administrator of University of New Hampshire Scholars' Repository. For more information, please contact [email protected]. TALKING ABOUT ABORTION: A QUALITATIVE EXAMINATION OF WOMEN’S ABORTION EXPERIENCES BY Diana L. Dumais B.A. Psychology, Keene State College, 2000 THESIS Submitted to the University of New Hampshire In Partial Fulfillment of The Requirements for the Degree of Master of Arts In Sociology September 2006 Reproduced with permission of the copyright owner. Further reproduction prohibited without permission. UMI Number: 1437627 INFORMATION TO USERS The quality of this reproduction is dependent upon the quality of the copy submitted. Broken or indistinct print, colored or poor quality illustrations and photographs, print bleed-through, substandard margins, and improper alignment can adversely affect reproduction. In the unlikely event that the author did not send a complete manuscript and there are missing pages, these will be noted. Also, if unauthorized copyright material had to be removed, a note will indicate the deletion. -

Unsafe Abortion in Brazil: a Systematic Review of the Scientific Production, 2008-2018 Aborto Inseguro No Brasil
REVISÃO REVIEW Aborto inseguro no Brasil: revisão sistemática da produção científica, 2008-2018 Unsafe abortion in Brazil: a systematic review of the scientific production, 2008-2018 Aborto inseguro en Brasil: revisión sistemática de la producción científica, 2008-2018 Rosa Maria Soares Madeira Domingues 1 Sandra Costa Fonseca 2 Maria do Carmo Leal 3 Estela M. L. Aquino 4 Greice M. S. Menezes 4 doi: 10.1590/0102-311X00190418 Resumo Correspondência R. M. S. M. Domingues Instituto Nacional de Infectologia Evandro Chagas, Fundação O objetivo deste estudo é atualizar o conhecimento sobre o aborto inseguro Oswaldo Cruz. no país. Foi realizada uma revisão sistemática com busca e seleção de estudos Av. Brasil 4365, Rio de Janeiro, RJ 21040-360, Brasil. via MEDLINE e LILACS, sem restrição de idiomas, no período 2008 a 2018, [email protected] com avaliação da qualidade dos artigos por meio dos instrumentos elaborados 1 pelo Instituto Joanna Briggs. Foram avaliados 50 artigos. A prevalência de Instituto Nacional de Infectologia Evandro Chagas, Fundação Oswaldo Cruz, Rio de Janeiro, Brasil. aborto induzido no Brasil foi estimada por método direto em 15% no ano de 2 Instituto de Saúde Coletiva, Universidade Federal Fluminense, 2010 e 13% no ano de 2016. Prevalências mais elevadas foram observadas Rio de Janeiro, Brasil. em populações socialmente mais vulneráveis. A razão de aborto induzido por 3 Escola Nacional de Saúde Pública Sergio Arouca, Fundação 1.000 mulheres em idade fértil reduziu no período 1995-2013, sendo de 16 por Oswaldo Cruz, Rio de Janeiro, Brasil. 4 Instituto de Saúde Coletiva, Universidade Federal da Bahia, 1.000 em 2013. -

Abortion by Rape Victim: a Dilemma in the Drat of Penal Code and Indonesian Health Law
Journal of Law and Legal Reform JOURNAL (2020 OF), 1 (LAW4), pp. & 631 LEGAL-640. REFORM VOLUME 1(4) 2020 631 DOI: https://doi.org/10.15294/jllr.v1i4.39659 ISSN (Print) 2715-0941, ISSN (Online) 2715-0968 RESEARCH ARTICLE ABORTION BY RAPE VICTIM: A DILEMMA IN THE DRAT OF PENAL CODE AND INDONESIAN HEALTH LAW Fikri Ariyad1, Ali Masyhar2 1 LBH Rumah Pejuang Keadilan Kota Semarang, Indonesia 2 Faculty of Law, Universitas Negeri Semarang, Indonesia [email protected] CITED AS Ariyad, F., & Masyhar, A. (2020). Abortion by Rape Victim: A Dilemma in the Drat of Penal Code and Indonesian Health Law. Journal of Law and Legal Reform, 1(4), 631-640. https://doi.org/10.15294/jllr.v1i4.39659 ABSTRACT In this present time, the debate about abortion in Indonesia is increasingly crowded. Abortion is also carried out by women - victims of rape to reduce the burden they suffered. The regulation on abortion in Indonesia has been regulated in the statutory regulations, namely the Criminal Code, especially in Article 346, Article 347, Article 348, and Article 349. In the RKUHP (Draft of Criminal Code), abortion regulation is regulated in two chapters namely, Chapter XIV Article 501 and Chapter XIX Articles 589, 590, 591, 592. In addition, the government has also issued several regulations governing abortion such as Government Regulation No. 61 of 2014 concerning Reproductive Health and also Law No. 36 of 2009 concerning health. However, the various regulations that exist between the Criminal Code, RKUHP, PP and the Act actually contradict to each other. There is no synchronization between the regulations regarding abortion by women rape victims. -

The Regulatory Model of Abortion in China Through a Feminist Lens* 1 Weiwei Cao Hunan University, China
The Regulatory Model of Abortion in China through a Feminist Lens* 1 Weiwei Cao Hunan University, China Abstract A medical, surgical termination of pregnancy is the only means of avoiding an unplanned and unwanted birth when contraception fails. Access to safe and afford- able abortion is therefore essential to satisfy women’s rights to health and the exercise of control over life choices. Restrictive law is usually considered as the main cause of abortions performed in illegal and unhygienic clinics, which could be health- or life-threatening. Thus, many feminists argue that women’s reproductive health and rights would be promoted by establishing a less restrictive regulatory model of abortion. By examining the Chinese abortion law, this paper aims to analyze whether it is liberal and if so, how it satisfies women’s rights to health and re- productive self-determination. While the law looks unrestrictive, in reality it fails to serve this purpose and instead facilitates the state’s manipulation of female fertility. Since the regulation of abortion in China is significantly determined by the state’s policy-making in relation to population, an in-depth analysis of the connection be- tween regulation and policy is given to indicate how the state imposes the burden of achieving its population goals on women. In addition, to further scrutinize how women’s rights to health and reproductive decision-making are violated by the im- plementation of abortion law in practice, this paper offers a discussion on the Chinese-style practice of family planning. Finally, feasible proposals are made for reformulating the Chinese regulatory model, so it can protect women’s health and reproductive rights from the state’s coercive involvement and can promote women’s access to adequate medical and state support.