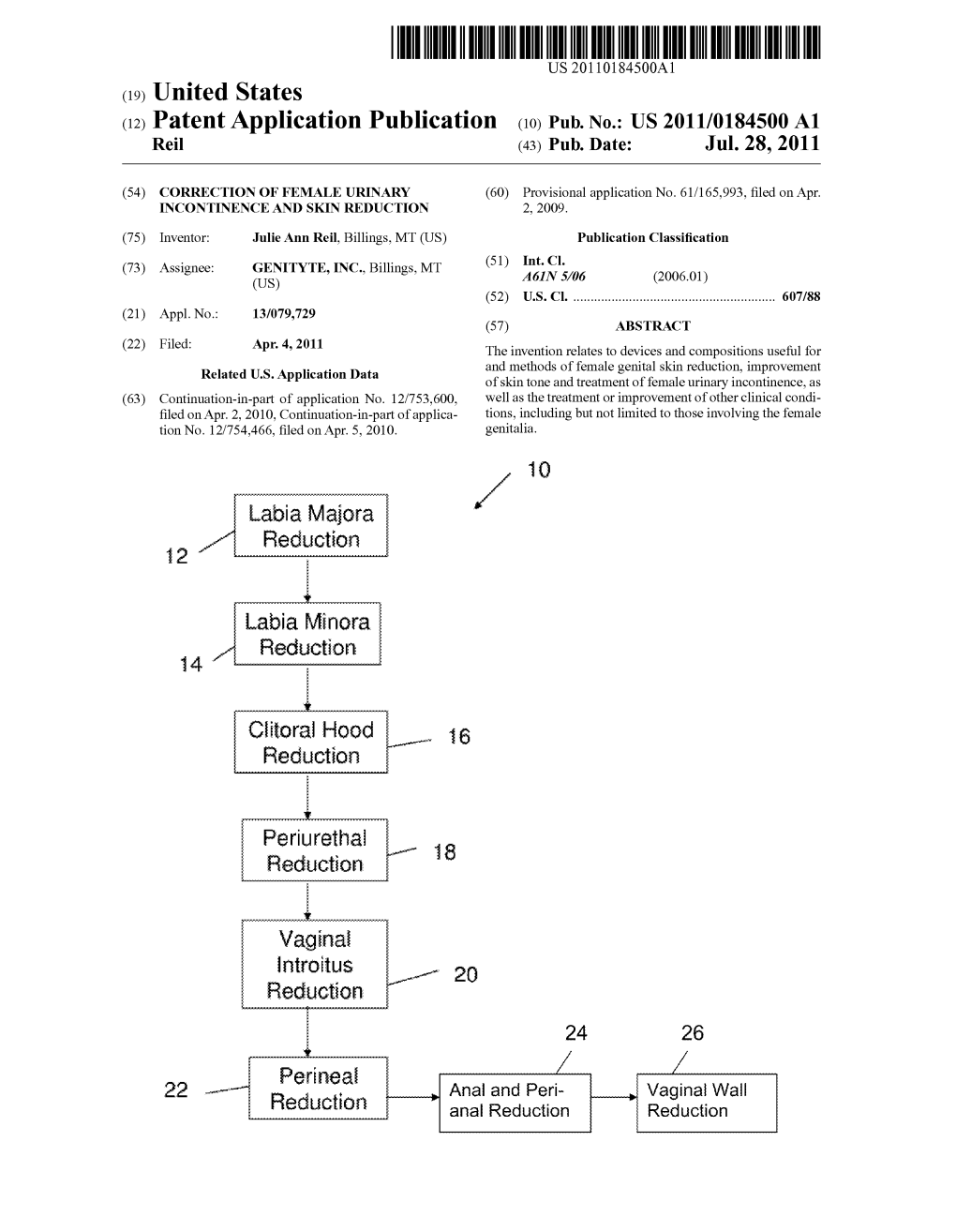
Reduction 2, 2009
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Aesthetic Surgery of the Female Genitalia
Aesthetic Surgery of the Female Genitalia Julie M.L.C.L. Dobbeleir, M.D.,1 Koenraad Van Landuyt, M.D., Ph.D.,2 and Stan J. Monstrey, M.D., Ph.D.2 ABSTRACT Aesthetic genital surgery seems to have become a fashionable issue nowadays. Many procedures and techniques have been described these last years, but very few long- term results or follow up studies are available. The novelty of this aspect of plastic surgery and the lack of evidence-based interventions, have led to a comparison with female genital mutilation. In this article, the authors provide an overview of the possible surgical procedures as well as the general principles of aesthetic surgery of the female genitalia. KEYWORDS:Genital surgery, genital cutting, labioplasty, vaginal tightening Aesthetic surgery of the female genitalia is a rium, many questions have been raised, regarding tech- much discussed topic in the popular press as well as the nical issues, indications, and—not in the least–ethics, scientific journals. It seems to be fashionable for men but few scientific answers are available. and women of today’s world to have their genitals As for every new specialty, guidelines need to be altered. set up and long-term studies are a necessity. Complicat- Although it might strike as a new trend quickly ing the issue even more is the fact that genital beauty is arising in all layers of society, it has been around for ages. very culturally defined. The same template and indica- The genital ideal may differ historically and cross- tions cannot be used cross-culturally. -

FGM – Female Genital Mutilation Kvinnlig Könsstympning
Trollhättan, 17+18/11 2016 Senior FGM – Female Genital Mutilation Kvinnlig Könsstympning Dr. med. Johannes Leidinger, MD., MPH. Senior Consultant in Gynaecology and Obstetrics Överläkare på Kvinnokliniken Södersjukhuset Stockholm & Mälarsjukhuset Eskilstuna Lehrbeauftragter/Dozent der Ludwig-Maximilians-Universität München 16 days of activism 2016 From 25 November, the International Day for the Elimination of Violence against Women, to 10 December, Human Rights Day, the 16 Days of Activism against Gender-Based Violence Campaign is a time to galvanize action to end violence against women and girls around the world. http://www.unwomen.org/en/what-we-do/ending-violence-against-women/ take-action/16-days-of-activism#sthash.zXvSzU8E.dpuf Sexual Violence: ¨ Rape ¨ Indecent Assault ¨ Forced Marriage ¨ Sexual Slavery http://www.eldis.org ¨ FGM (Female Genital Mutilation) ¨ Forced Pregnancy ¨ Forced Abortion ¨ Sexual Harassment WHO: FGM ¨ „FGM comprises all procedures that involve altering or injuring the female genitalia for non medical reasons - , and is recognized internationally as a violation of the human rights of girls and women. It reflects deep-rooted inequality between the sexes, and constitutes an extreme form of discrimination against women and girls.“ Program 18 Nov 2016, 9-12 am ¨ Nomenklatur ¨ Klassifikation ¨ Global Prevalens ¨ Förklaringsmodeller ¨ Medicinska komplikationer ¨ Nationell & internationell Lagstiftning ¨ Vård i Sverige – AMEL-mottagning – Operativa rekonstruktioner – Desert Flower Scandinavia ¨ Global perspektiv – Internationella strategier (WHO och NGOs) – Medicalization of FGM Terminology ¨ The expression ”Female Genital Mutilation" gained growing support from the late 1970s. The word ”mutilation” establishes a clear linguistic distinction from male circumcision, and emphasizes the gravity and harm of the act. ¨ In 1990, this term was adopted at the ”3rd Conference of the Inter-African Committee on Traditional Practices Affecting the Health of Women and Children”, in Addis Ababa, Ethiopia. -

Labiaplasty Brochure
· LABIAPLASTY· · TESTIMONIAL · · OTHER TREATMENTS THAT FURTHER REJUVENATE THE LABIA AND VAGINA · "I have been contemplating labiaplasty for some time now. I only have one child and my issues with my labia were not due to childbirth. Obviously, this · PRP INJECTION THERAPY- Your own growth particular subject matter could even make the most self-assured a bit factors provide for the most healthy tissue uncomfortable. Yet, there was never a moment that I felt judged in any way by growth and best healing. Dr. Bloy or anyone in his oce. Everyone ...across the board... was supportive · JULIET FEMININE LASER- Laser treatment for and reassuring. The procedure was done under local anesthesia which made the choice easier for me. I did not even require medication to calm me down or the labia (outside) or vagina (inside) tightens, sedate me, so I was able to drive myself to and from the appointment. The restores function and increases collagen. procedure was pain-free. I was in and out in under two hours with my brand · LABIAL PUFFING- Dermal fillers are used to new and pretty vagina! I cannot begin to say enough times how highly I plump the tissue creating more youthful labia. recommend Dr. Bloy and his oce in Ft. Myers, Florida. They did everything but · LASER HAIR REMOVAL- Permanent hair jump through hoops for me to make the experience streamlined and eortless. reduction delivers smooth, soft skin free of Dr. Bloy's years of experience and caring heart will put you at ease every step of the way." razor bumps, irritation, and without time - Actual 48-Year-Old CHC Patient consuming waxing or shaving. -

Female Genital Cosmetic Surgery: a Review of Techniques and Outcomes
Int Urogynecol J (2013) 24:1997–2009 DOI 10.1007/s00192-013-2117-8 REVIEW ARTICLE Female genital cosmetic surgery: a review of techniques and outcomes Cheryl B. Iglesia & Ladin Yurteri-Kaplan & Red Alinsod Received: 15 April 2013 /Accepted: 18 April 2013 /Published online: 22 May 2013 # The International Urogynecological Association 2013 Abstract The aesthetic and functional procedures that com- Keyword Female genital cosmetic surgery . Cosmetic prise female genital cosmetic surgery (FGCS) include tradi- gynecology . Vaginal rejuvenation . Labiaplasty . tional vaginal prolapse procedures as well as cosmetic Vaginoplasty vulvar and labial procedures. The line between cosmetic and medically indicated surgical procedures is blurred, and today many operations are performed for both purposes. The Introduction contributions of gynecologists and reconstructive pelvic surgeons are crucial in this debate. Aesthetic vaginal sur- Consumer marketing and media hype have spawned the con- geons may unintentionally blur legitimate female pelvic siderable controversy over female genital cosmetic surgery floor disorders with other aesthetic conditions. In the ab- (FGCS). FGCS articles first appeared in North American sence of quality outcome data, the value of FGCS in im- journals in 1978, and the first technical article appeared in proving sexual function remains uncertain. Women seeking 1984 [1, 2]. This review describes the techniques and outcome FGCS need to be educated about the range and variation of data of labiaplasty, vaginoplasty, and other cosmetic gyneco- labia widths and genital appearance, and should be evaluat- logical procedures. ed for true pelvic support disorders such as pelvic organ prolapse and stress urinary incontinence. Women seeking FGCS should also be screened for psychological conditions Female genital perceptions and should act autonomously without coercion from part- ners or surgeons with proprietary conflicts of interest. -
LABIAPLASTY: Labia Minora Reduction LABIA MAJORA
10/27/2016 Aesthetic Surgery of Female Genitalia: A Plastic Surgery Perspective Maura Reinblatt, MD, FACS Assistant Professor of Surgery Division Plastic & Reconstructive Surgery Icahn School of Medicine at Mount Sinai DISCLOSURES No relevant financial relationships with a commercial interest 1 10/27/2016 WHO AM I? . Board Certified by American Board of Surgery . Board Certified by American Board of Plastic Surgery . Member of ASPS . Member ASAPS . Former faculty at Johns Hopkins School of Medicine . Practicing 9 years SPECIALTIES WORKING TOGETHER What we do What we do NOT do 2 10/27/2016 WHY? . Styles & fashion . Popularity of waxing & hairless trend . Primarily cosmetic in nature “meat curtains” . Complaints of rubbing with cycling & running . Complaints of feeling “bulky” in yoga clothes . How a woman perceives her genitals may have a positive effect on sexual function . Possible insurance with preapproval CPT 56620 . Congenital, puberty, pregnancy, age Hamori CA. Postoperative clitoral hood deformity after labiaplasty. Aesthet Surg J. 2013 Sep 1;33(7):1030-6. “Vaginas Under Attack”? . Cosmopolitan Magazine Cover July 2010 . Vaginas Under Attack: Don’t Let a Greedy Gyno Talk You into This Horrible Mistake . Perception doctors are encouraging patients . Women are actively seeking this procedure . Ethics of safety & marketing of cosmetic vaginal surgery has been raised . Reports of cosmetic procedures on external genitals in both plastics & gynecology date to 70’s-80’s -Hamori CA. Aesthet Surg J. 2013 Sep 1;33(7):1030-6. -Hardwick-Smith S. Examining the controversy in aesthetic vaginal surgery. Am J Cosmet Surg. 2011;28:106–113. 3 10/27/2016 PLASTICS LEADERS & MENTORS Dr. -

Clitoral Reconstructive Surgery After Female Genital Cutting
FEATURE Clitoral reconstructive surgery after female genital cutting BY AMR SEIFELDIN emale genital mutilation / cutting (FGM/C), aka female circumcision, is defined by the World Health FOrganization (WHO) as “All procedures that involve partial or total removal of the external female genitalia for non-medical reasons” [1]. Practised in Africa and other parts of the world, the WHO recently estimated that over 250 million females have been circumcised so far, and an additional three million are at risk of circumcision each year, nearly 8000 cases a day [2]. First recorded in Egypt in the 5th Century BC, and noted on a papyrus from Memphis in 2nd Century BC, its historic background goes back more than 3000 years. Some ancient Egyptian mummies were found to World Health Organization Classification of Female Genital Mutilation have been circumcised. Type I: Partial or total removal of Type Ia: Removal of the clitoral hood or prepuce FGM/C awareness has increased globally the clitoris and / or the prepuce only in the past 20 years, due to an increased (clitoridectomy) influx of African immigrants and refugees, Type Ib: Removal of the clitoris with the prepuce with 680,000 cases in Europe and 513,000 Type II: Partial or total removal of the Type IIa: Removal of the labia minora only in the United States, putting a heavy burden clitoris and the labia minora, with or Type IIb: Partial or total removal of the clitoris and on the healthcare systems of the host without excision of the labia majora (excision) the labia minora countries. It is a destructive procedure, Type IIc: Partial or total removal of the clitoris, the criminalised by law in most countries, and labia minora and the labia majora considered a crime against humanity [3]. -

Labiaplasty Brochure
· LABIAPLASTY· · TESTIMONIAL · · OTHER TREATMENTS THAT REJUVENATE THE "I have been contemplating labiaplasty for some time now. I only have one child and my issues with LABIA AND VAGINA · my labia were not due to childbirth. Obviously, this particular subject matter could even make the most self-assured a bit uncomfortable. Yet, there was never a moment that I felt judged in any way · PRP INJECTION THERAPY- Your own growth factors by Dr. Bloy or anyone in his office. Everyone ...across the board... was supportive and reassuring. provide for the most healthy tissue growth and best The procedure was done under local anesthesia which made the choice easier for me. I did not even healing. require medication to calm me down or sedate me, so I was able to drive myself to and from the appointment. The procedure was pain-free. I was in and out in under two hours with my brand new · JULIET FEMININE LASER- Laser treatment for the labia and pretty vagina! I cannot begin to say enough times how highly I recommend Dr. Bloy and his (outside) or vagina (inside) tightens, restores function, stops office in Ft. Myers, Florida. They did everything but jump through hoops for me to make the stress urinary incontinence and increases collagen. experience streamlined and effortless. Dr. Bloy's years of experience and caring heart will put you at · LABIAL PUFFING- Dermal fillers are used to immediately ease every step of the way." plump the outer labia creating more youthful appearance. - Actual 48-Year-Old CHC Patient · VAMPIRE WINGLIFT - Natural, patented PRP treatment rejuvenates labia using your own growth factors. -

Clitoral Hood Reduction Surgery to Decrease the Size of the Clitoral
Clitoral Hood Reduction Surgery to decrease the size of the clitoral hood to improve the genital appearance and increase sensation What is Clitoral Hood Reduction? Clitoral Hood Reduction is surgery to remove excess skin from the hood of the clitoris, reducing its size and increasing clitoral sensation. The experienced surgeons at Bella Vou provide bespoke Intimate Rejuvenation. Clitoral Hood Reduction can be a stand-alone procedure or combined with a Labia Minor Reduction to remove excess folds of skin, rejuvenate the vulva, and create a neat and balanced genital appearance. Why have Clitoral Hood Reduction? Natural anatomy and the effects of ageing can make the skin over the clitoris appear bulgy or prominent. The clitoral hood may protrude, catching on clothing or causing discomfort during sex. It can also make the area stick out so that it resembles a small penis. Furthermore, for some women, the excess skin over the clitoris reduces sensation and subdues sexual pleasure. If you are unhappy with the appearance of your vulva, if excess skin covering your clitoris is reducing your confidence and affecting your sex life, then Clitoral Hood Reduction surgery can help. The specialist aesthetic surgeons can remove excess skin to improve the appearance of the genital area and restore your body confidence. What happens in Clitoral Hood Reduction? At Bella Vou, Clitoral Hood Reduction is performed under local anaesthetic as a day case procedure, so you won’t need to stay in the clinic overnight. The surgeon carefully cuts away the extra tissue to make the hood shorter, neater, and less prominent. -

Patient Brochure 2018
Patient Information Booklet AESTHETIC VULVOVAGINAL SURGERY AT SOUTH COAST UROGYNECOLOGY 2018 v Red M. Alinsod, M.D., FACOG, FACS, ACGE 949-499-5311 • [email protected] www.urogyn.org Pacific Coast Highway, Laguna Beach, California Red M. Alinsod, M.D., FACOG, FACS, ACGE 2 Contents Introduction to The Alinsod Institute for Aesthetic Vaginal Surgery 3 Vaginoplasty (vaginal rejuvenation) 39 About Dr. Red Alinsod 4 Description of Surgical Procedures - Perineoplasty 40 Introduction to South Coast Urogynecology 5 Description of Surgical Procedures - Labia Minora Plasty 41 Office Photos 6 Description of Surgical Procedures - Labia Majora Plasty Cont. 42 Meet Our Staff 7 Description of Surgical Procedures - Clitoral Hood Reduction 43 Meet Our Staff 8 Description of Surgical Procedures - Hymenoplasty 44 The Process: What happens when you finally decide to have surgery 45 Medical Treatments 9 The Process cont. 46 Procedure Details for Labiaplasty in the Office 47 Speciality Descriptions for SCU 10 Procedure Details for Labiaplasty in the Office cont. 48 High Frequency (No Scalpel) Surgery vs. Laser Surgery 11 Labiaplasty and Vaginoplasty Recovery Ellman Surgitron versus Lasers: Which is Best? 12 Essential Pre-Op Instructions 49 Ellman/Laser Lab: Seeing is believing 13 Post-Operative Care Instructions 50 What is Vaginal Rejuvenation? 14 What is Vaginal Rejuvenation? (cont.) 15 Before and After Photos 51-52 Frequently Asked Questions about Vaginal Surgery 16-21 Case Studies of Dr. Alinsod’s Vaginal Surgeries 53 ThermiVa: Non-Surgical Vaginal Tightening -

The Extended Clitoral-U Suspension and Unhooding
Case Report Clinics in Surgery Published: 16 Feb, 2018 The Extended Clitoral-U Suspension and Unhooding Steven P Davison*, Kylie D Hayes and Gabrielle LaBove Department of Plastic Surgery, Georgetown University Hospital, USA Abstract Labiaplasty with clitoral unhooding is becoming a more common procedure. The authors discuss the extended clitoral-U suspension, and unhooding technique to address both the labia minora excess and clitoral hooding of the patient. Introduction As labiaplasty has become more main stream the labia minora reduction procedure has changed from discussing the amputation technique versus the wedge technique to a more tailored approach to each patient. One of the a la carte additions to labia minora reduction has been the clitoral hood reduction. This has been particularly successful as it addresses the visible tissue show of the clitoral prepuce in the anterior labial commissure, a major concern for the patient [1]. Patients with significant clitoral hooding often present with frustration with the forward standing view presentation of their labia and clitoral hood in which three arches and two folds appear (Figure 1). Case Presentation Current techniques Two main surgical techniques have addressed the clitoral unhooding. The first described by Gary Alter removes a horizontal central cleft of tissue midshaft on the clitoral hood [2]. The next technique, most effectively communicated by Hamori, reduces the overhang just dorsal to the clitoral hood [3]. Neither of the techniques observes the time-aged plastic surgery trick of hiding incisions at subunit transitions. Technical Detail We suggest that placing the suture line at the vaginal cleft rim and resecting the proximal one- third to one-half of the hood has considerable advantages. -

Gynecology & Gynecologic Oncology
Rafal Kuzlik, Gynecol Obstet 2018, Volume 8 conferenceseries.com DOI: 10.4172/2161-0932-C2-027 6th International Congress on Gynecology & Gynecologic Oncology July 23-24, 2018 | Rome, Italy Radiofrequency - New solution for treatment of vaginal laxity, urinary incontinence and sexual disorders Rafal Kuzlik SaskaMed Clinic, Poland Introduction: Vaginal laxity, urinary incontinence and sexual disfunction, They are very serious problems of many women. All over the world there are many devices to treat patients with these disorders. Objectives: To prove, that radiofrequency is a safe procedure with fast results. Materials and methods: 24 patients took part in the study, aged between 30 and 70 y.o. with vaginal laxity and urinary incontinence. Excluding criteria: vagina’s width over 3 fingers, level of SUI over second degree, vaginal bleeding, unproper PAP smear or other pathologies of the vagina and uterus, Besides vaginal and urinary problems, sexual satisfaction was taken under consideration. In the study ThermiVa was used as radiofrequency device. 3 examinations were made: before, after first and second procedure. All procedures were performed with temperature 45-47 º C. Results: Over 30% of improvement was observed. Conclusions: Radiofrequency procedures using ThermiVa are safe and effective, without any side effects. Biography Rafal Kuzlik MD, PhD, specialist in obstetrics and gynecology. Plastic and reconstrative gynecologist with over twenty years of professional experience. He is endoscopist and oncological surgeon. Specialist in ultrasound imaging. Doctor Rafal Kuzlik received a lot of certificates confirming participation in numerous courses and trainings. He published many scientific papers. Co-author of two books (in Polish): „Plastic Gynecology” and „Physiotherapy after plastic surgical procedures”. -

An Analysis of the Content and Clinical Implications of Online Advertisements for Female Genital Cosmetic Surgery
BMJ Open: first published as 10.1136/bmjopen-2012-001908 on 21 November 2012. Downloaded from Open Access Research An analysis of the content and clinical implications of online advertisements for female genital cosmetic surgery Lih-Mei Liao, Neda Taghinejadi, Sarah M Creighton To cite: Liao L-M, ABSTRACT ARTICLE SUMMARY Taghinejadi N, Creighton SM. Objectives: Women who are contemplating any form An analysis of the content of female genital cosmetic surgery (FGCS) are likely to and clinical implications of Article focus seek information from provider websites. The aim of online advertisements for ▪ A content analysis of the clinical information in female genital cosmetic this study is to examine the breadth, depth and quality web-based advertisements for female genital surgery. BMJ Open 2012;2: of clinical information communicated to women on 10 cosmetic surgery (FGCS), focusing on 10 easily e001908. doi:10.1136/ popular sites and to discuss the implications of the accessed provider websites. bmjopen-2012-001908 results. Methods: The content of online advertisement from Key messages ▪ No lower age limit is stated for any of the elective ▸ Prepublication history for 10 private providers that offer FGCS procedures was this paper are available examined according to 16 information categories procedures. ▪ online. To view these files relating to indications for surgery, types of procedure, Information pertaining to the unknowns and to please visit the journal online risks and benefits. the anecdotal nature of clinical claims is (http://dx.doi.org/10.1136/ Results: FGCS procedures were presented on all of missing. ▪ bmjopen-2012-001908). the provider websites as an effective treatment for Numerous labels pertaining perhaps to similar genital appearance concerns.