Therapeutic Class Overview Opioids, Short Acting
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
These Highlights Do Not Include All the Information Needed to Use BENZHYDROCODONE and ACETAMINOPHEN TABLETS Safely and Effectively
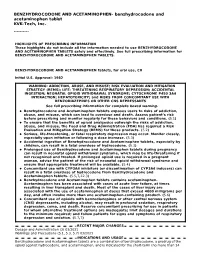
BENZHYDROCODONE AND ACETAMINOPHEN- benzhydrocodone and acetaminophen tablet KVK-Tech, Inc. ---------- HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information needed to use BENZHYDROCODONE AND ACETAMINOPHEN TABLETS safely and effectively. See full prescribing information for BENZHYDROCODONE AND ACETAMINOPHEN TABLETS. BENZHYDROCODONE AND ACETAMINOPHEN tablets, for oral use, CII Initial U.S. Approval: 1982 WARNING: ADDICTION, ABUSE, AND MISUSE; RISK EVALUATION AND MITIGATION STRATEGY (REMS); LIFE- THREATENING RESPIRATORY DEPRESSION; ACCIDENTAL INGESTION; NEONATAL OPIOID WITHDRAWAL SYNDROME; CYTOCHROME P450 3A4 INTERACTION; HEPATOTOXICITY; and RISKS FROM CONCOMITANT USE WITH BENZODIAZEPINES OR OTHER CNS DEPRESSANTS See full prescribing information for complete boxed warning. Benzhydrocodone and Acetaminophen tablets exposes users to risks of addiction, abuse, and misuse, which can lead to overdose and death. Assess patient’s risk before prescribing and monitor regularly for these behaviors and conditions. (5.1) To ensure that the benefits of opioid analgesics outweigh the risks of addiction, abuse, and misuse, the Food and Drug Administration (FDA) has required a Risk Evaluation and Mitigation Strategy (REMS) for these products. (5.2) Serious, life-threatening, or fatal respiratory depression may occur. Monitor closely, especially upon initiation or following a dose increase. (5.3) Accidental ingestion of Benzhydrocodone and Acetaminophen tablets, especially by children, can result in a fatal overdose of hydrocodone. (5.3) Prolonged use of Benzhydrocodone and Acetaminophen tablets during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated. If prolonged opioid use is required in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available. -

Analgesia After Cesarean Section in Preeclampsia Parturients Receiving Magnesium Sulfate: a Retrospective Comparison with Non-Preeclampsia Parturients
Anesth Pain Med 2012; 7: 136~141 ■Clinical Research■ Analgesia after Cesarean section in preeclampsia parturients receiving magnesium sulfate: a retrospective comparison with non-preeclampsia parturients † Department of Anesthesiology and Pain Medicine, *Seoul National University Bundang Hospital, Seongnam, Seoul National University ‡ Hospital, Boramae Medical Center, Seoul, Korea Hyo-Seok Na*, Hyun-Bin Kim†, Chong-Soo Kim‡, and Sang-Hwan Do* Background: Magnesium sulfate (MgSO4) is the first-line therapy Key Words: Cesarean section, Magnesium sulfate, Postoperative for managing preeclampsia in obstetrics. Its perioperative adminis- pain, Preeclampsia. tration has been proved to be an effective analgesic adjuvant, which we investigated in parturients undergoing Cesarean section (C-sec). Methods: A retrospective chart review examined 504 parturients INTRODUCTION who underwent C-secs between June 2006 and August 2010, including normal parturients (group N, n = 401) and those diagnosed In parturients with preeclampsia, magnesium sulfate (MgSO4) with preeclampsia (group P, n = 103). A postoperative numeric is the first choice drug for the prevention of eclamptic rating scale (NRS) was used to assess pain, and the number of seizures. It is administered routinely via a loading dose and rescue analgesic administrations and frequency of transfusions were investigated. Perioperative magnesium concentrations were recor- continuous infusion with a target serum concentration of 2− ded for patients in group P. 3.5 mmol/L during the antepartum period and is continued Results: Patients in group P had longer operation and anesthesia until at least 24 h postpartum [1]. times, and more postoperative admission days than those in group Magnesium acts as an N-methyl-D-aspartate (NMDA) recep- N. -

Summary Analgesics Dec2019
Status as of December 31, 2019 UPDATE STATUS: N = New, A = Advanced, C = Changed, S = Same (No Change), D = Discontinued Update Emerging treatments for acute and chronic pain Development Status, Route, Contact information Status Agent Description / Mechanism of Opioid Function / Target Indication / Other Comments Sponsor / Originator Status Route URL Action (Y/No) 2019 UPDATES / CONTINUING PRODUCTS FROM 2018 Small molecule, inhibition of 1% diacerein TWi Biotechnology / caspase-1, block activation of 1 (AC-203 / caspase-1 inhibitor Inherited Epidermolysis Bullosa Castle Creek Phase 2 No Topical www.twibiotech.com NLRP3 inflamasomes; reduced CCP-020) Pharmaceuticals IL-1beta and IL-18 Small molecule; topical NSAID Frontier 2 AB001 NSAID formulation (nondisclosed active Chronic low back pain Phase 2 No Topical www.frontierbiotech.com/en/products/1.html Biotechnologies ingredient) Small molecule; oral uricosuric / anti-inflammatory agent + febuxostat (xanthine oxidase Gout in patients taking urate- Uricosuric + 3 AC-201 CR inhibitor); inhibition of NLRP3 lowering therapy; Gout; TWi Biotechnology Phase 2 No Oral www.twibiotech.com/rAndD_11 xanthine oxidase inflammasome assembly, reduced Epidermolysis Bullosa Simplex (EBS) production of caspase-1 and cytokine IL-1Beta www.arraybiopharma.com/our-science/our-pipeline AK-1830 Small molecule; tropomyosin Array BioPharma / 4 TrkA Pain, inflammation Phase 1 No Oral www.asahi- A (ARRY-954) receptor kinase A (TrkA) inhibitor Asahi Kasei Pharma kasei.co.jp/asahi/en/news/2016/e160401_2.html www.neurosmedical.com/clinical-research; -

Efficacy of Opioids and Non-Opioid Analgesics in the Treatment of Post Procedure Pain of Burned Patients: a Narrative Review
Journal Pre-proof Efficacy of opioids and non-opioid analgesics in the treatment of post procedure pain of burned patients: a narrative review Paola Andrea Chinchilla Hermida, Jairo Ricardo Moyano Acevedo PII: S0104-0014(21)00303-1 DOI: https://doi.org/10.1016/j.bjane.2021.07.022 Reference: BJANE 744243 To appear in: Brazilian Journal of Anesthesiology (English edition) Received Date: 1 October 2020 Accepted Date: 20 July 2021 Please cite this article as: Hermida PAC, Acevedo JRM, Efficacy of opioids and non-opioid analgesics in the treatment of post procedure pain of burned patients: a narrative review, Brazilian Journal of Anesthesiology (English edition) (2021), doi: https://doi.org/10.1016/j.bjane.2021.07.022 This is a PDF file of an article that has undergone enhancements after acceptance, such as the addition of a cover page and metadata, and formatting for readability, but it is not yet the definitive version of record. This version will undergo additional copyediting, typesetting and review before it is published in its final form, but we are providing this version to give early visibility of the article. Please note that, during the production process, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain. © 2020 Published by Elsevier. BJAN-D-20-00269 - Narrative Review Efficacy of opioids and non-opioid analgesics in the treatment of post procedure pain of burned patients: a narrative review Paola Andrea Chinchilla Hermidaa,*, Jairo Ricardo Moyano Acevedob a Universidad El Bosque, Medicina Del Dolor y Cuidados Paliativos, Bogota, Colombia b Fundación Santafé Bogotá, Anesthesia Department, Pain Service, Bogota, Colombia * Corresponding author. -

Enhancement of Antinociception but Not Constipation by Combinations
Archives of Medical Research 44 (2013) 495e503 ORIGINAL ARTICLE Enhancement of Antinociception but not Constipation by Combinations Containing Tramadol and Metamizole in Arthritic Rats Francisco Javier Lopez-Mu noz,~ a Luis Alfonso Moreno-Rocha,a Guadalupe Bravo,a Uriah Guevara-Lopez, b Adriana Miriam Domınguez-Ramırez,c and Myrna Deciga-Camposd aDepartamento de Farmacobiologıa, Centro de Investigacion y Estudios Avanzados, Sede Sur, Mexico, D.F., Mexico bDireccion de Educacion e Investigacion en Salud, Unidad Medica de Alta Especialidad Dr. Victorio de la Fuente Narvaez, Instituto Mexicano del Seguro Social, Mexico, D.F., Mexico cDepartamento Sistemas Biologicos, Universidad Autonoma Metropolitana, Unidad Xochimilco, Mexico, D.F., Mexico dSeccion de Posgrado e Investigacion de la Escuela Superior de Medicina del Instituto Politecnico Nacional, Mexico, D.F., Mexico Received for publication February 1, 2013; accepted August 26, 2013 (ARCMED-D-13-00072). Background and Aims. The use of a combination of analgesics could provide an optimal pain treatment with minimal side effects. Combinations of tramadol and some nonste- roidal anti-inflammatory drugs have demonstrated synergistic antinociceptive effects as well as a significantly reduced occurrence of adverse effects. The purpose of this study was to investigate the antinociceptive and constipation effects of tramadol and metami- zole alone or in combination in rats and to discern among the types of drug interactions that exist using dose-response curves and an isobolographic analysis. Methods. The antinociceptive effects of tramadol and metamizole, alone or in various combination ratios, were quantitatively evaluated using the ‘‘pain-induced functional impairment model in the rat.’’ Additionally, the constipation effect was evaluated using the charcoal meal test. -

Short-Acting Opioid Analgesics
Short-acting Opioid Analgesics Goals: Restrict use of short-acting opioid analgesics for acute conditions funded by the OHP. Promote use of preferred short-acting opioid analgesics. Length of Authorization: Initial: 7 to 30 days (except 12 months for end-of-life, sickle cell disease, severe burn injury, or cancer-related pain) Renewal: Up to 6 months Covered Alternatives: Current PMPDP preferred drug list per OAR 410-121-0030 at www.orpdl.org Searchable site for Oregon FFS Drug Class listed at www.orpdl.org/drugs/ Requires a PA: Non-preferred short-acting opioids and opioid combination products. All short-acting products prescribed for more than 14 days. Each prescription is limited to 7 days in treatment-naïve patients. Patients may fill up to 2 prescriptions every 90 days without prior authorization. All codeine and tramadol products for patients under 19 years of age Note: Patients on palliative care with a terminal diagnosis or with cancer-related pain or with pain associated with sickle cell disease or severe burn injury are exempt from this PA. Table 1. Daily Dose Threshold (90 morphine milligram equivalents per day (MME/day) of Oral Opioid Products. Opioid 90 MME/day Dose Notes Benzhydrocodone 73.5 mg Codeine 600 mg Codeine is not recommended for pediatric use; codeine is a prodrug of morphine and is subject to different rates of metabolism, placing certain populations at risk for overdose. Dihydrocodeine 360 mg Hydrocodone bitartrate 90 mg Hydromorphone 22.5 mg Levorphanol tartrate 8 mg Meperidine 900 mg Meperidine is not recommended for management of chronic pain due to potential accumulation of toxic metabolites. -

Acetaminophen, Caffeine and Dihydrocodeine Bitartrate* Tablets CIII 712.8 Mg/60 Mg/32 Mg Rx Only Code 790Z00 Rev
ACETAMINOPHEN, CAFFEINE AND DIHYDROCODEINE BITARTRATE- acetaminophen, caffeine and dihydrocodeine bitartrate tablet MIKART, INC. ---------- Acetaminophen, Caffeine and Dihydrocodeine Bitartrate* Tablets CIII 712.8 mg/60 mg/32 mg Rx only Code 790Z00 Rev. 02/99 DESCRIPTION Acetaminophen, Caffeine and Dihydrocodeine Bitartrate Tablets are supplied in tablet form for oral administration. Each tablet contains: Acetaminophen..........................................................712.8 mg Caffeine.....................................................................60 mg Dihydrocodeine Bitartrate*..........................................32 mg (*Warning: May be habit forming) Acetaminophen (4'-hydroxyacetanilide), a slightly bitter, white, odorless, crystalline powder, is a non- opiate, non-salicylate analgesic and antipyretic. It has the following structural formula: C8H9NO2 M.W. = 151.17 Caffeine (1,3,7-trimethylxanthine), a bitter, white powder or white-glistening needles, is a central nervous system stimulant. It has the following structural formula: C8H10N4O2 (anhydrous) M.W. = 194.19 Dihydrocodeine bitartrate (4,5α-Epoxy-3-methoxy-17-methylmorphinan-6α-ol (+)-tartrate), an odorless, fine white powder is an opioid analgesic. It has the following structural formula: C18H23NO3•C4H6O6 M.W. = 451.48 In addition, each tablet contains the following inactive ingredients: colloidal silicon dioxide, crospovidone, magnesium stearate, microcrystalline cellulose, povidone, pregelatinized starch, stearic acid, D&C Red #27 Aluminum Lake, D&C Red #30 -
Abuse-Deterrent Formulation (ADF) Opioid Medications
Abuse-Deterrent Formulation (ADF) Opioid Medications Mark Garofoli, PharmD, MBA, BCGP, CPE Director, Experiential Learning Program WVU School of Pharmacy Clinical Pain Management Pharmacist, WVU Medicine Center for Integrative Pain Management Opioid Risk Screenings Opioid Naïve Opioid Experienced Self Reported Self Reported • Drug Abuse Screening Test (DAST) • Current Opioid Misuse Measure (COMM) • Screener & Opioid Assessment for Patients with Pain (SOAPP) • Pain Medication Questionnaire (PMQ) • Prescription Drug Use Questionnaire, Patient (PDUQp) Provider Reported • Opioid Risk Tool (ORT) Provider Reported • Diagnosis, Intractability, Risk, & Efficacy Score (DIRE) • Prescription Drug Use Questionnaire (PDUQ) www.opioidrisk.com Opioid Risk Tool (ORT) Opioid Risk Tool (ORT) Female Male Family History of SUD Alcohol 1 3 Illegal Drugs 2 3 Prescription Drugs 4 4 Personal History of SUD Alcohol 3 3 Illegal Drugs 4 4 Low Risk 0 - 3 Prescriptions Drugs 5 5 Moderate Risk 4 - 7 Age 16-45 1 1 High Risk >/= 8 History of Preadolescence Yes 3 0 Sexual Abuse Psychological Disease ADHD, OCD, Bipolar, Schizophrenia 2 2 Depression 1 1 Total Score Where are these opioids coming from… Friend/Relative (Theft) Drug Dealer Rx from >1 MD Clinician/Office (Theft) Friend/Relative Rx from 1 MD (Buy) Friend/Relative (Free) 2017 DEA National Drug Threat Assessment. https://www.dea.gov/docs/DIR-040-17_2017-NDTA.pdf Opioid Abuse Transition Hydrocodone Oxycodone Oxycodone Combo Combo IR Sole ER/IR Heroin Tablets Products Products ($10/Bag) $5-10/Tab $10-15/Tab $1.50/mg Shah A, et al. Characteristics of Initial Prescription Episodes and Likelihood of Long-Term Opioid Use – United States, 2006-2015. -

208653Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 208653Orig1s000 CLINICAL REVIEW(S) As noted by the biopharmaceutics reviewer, the in vitro dissolution method for the drug product “was derived directly from the USP monograph for Hydrocodone Bitartrate and Acetaminophen Tablets. The dissolution method of KP201 had been determined in buffers with different pH conditions. This method also showed that the dissolving conditions of acetaminophen matched those in the USP monograph. Therefore, the proposed dissolution method as Apparatus II (paddle), 0.1N HCl, 900 mL, 50 rpm, is acceptable for the drug product.” The in vitro dissolution method was adequately validated, and the mean and individual dissolution data were acceptable for the drug product. The CMC microbiology review found the drug product to be a low microbial risk solid oral tablet, (b) (4) and found the Applicant’s request for waiver of microbial limit testing (MLT) specifications for drug product release and stability specifications acceptable. The Applicant has committed to MLT and (b) (4) tests on these stability batches annually and to report additional stability data from these studies in post-approval Annual Reports to the NDA. The tablets are stored in HDPE bottles (b) (4) The facilities, the site responsible for drug product manufacture, packaging and labeling, and release and stability testing, is (b) (4) As noted in the CMC review (b) (4) : (b) (4) The response to the information request was adequate and the reviewer concluded that “based on the acceptable inspectional history of this facility, their experience with these unit operations, and the adequate IR responses received, (b) (4) is acceptable for NDA 208653.” Sufficient data were provided to support the quality and safety of the manufacture and release of the drug substance and drug product. -

FDA Briefing Document Joint Meeting of Anesthetic and Analgesic Drug
FDA Briefing Document Joint Meeting of Anesthetic and Analgesic Drug Products Advisory Committee and Drug Safety and Risk Management Advisory Committee May 5, 2016 1 of 158 DISCLAIMER STATEMENT The attached package contains background information prepared by the Food and Drug Administration (FDA) for the panel members of the advisory committee. The FDA background package often contains assessments and/or conclusions and recommendations written by individual FDA reviewers. Such conclusions and recommendations do not necessarily represent the final position of the individual reviewers, nor do they necessarily represent the final position of the Review Division or Office. We have brought results of studies evaluating the abuse of KP201 (benzhydrocodone/acetaminophen) tablets to this Advisory Committee in order to gain the Committee’s insights and opinions, and the background package may not include all issues relevant to the final regulatory recommendation and instead is intended to focus on issues identified by the Agency for discussion by the advisory committee. The FDA will not issue a final determination on the issues at hand until input from the advisory committee process has been considered and all reviews have been finalized. The final determination may be affected by issues not discussed at the advisory committee meeting. 2 of 158 FOOD AND DRUG ADMINISTRATION Center for Drug Evaluation and Research Joint Meeting of the Anesthetic and Life Support Drugs Advisory Committee and Drug Safety & Risk Management Advisory Committee May 5, 2016 Table of Contents- Open Session Background Materials Page 1. Division of Anesthesia, Analgesia, and Addiction Products (DAAAP) 4 Director Memorandum (Dr. Hertz) 2. Regulatory History of Abuse-Deterrent Opioids 7 3. -

Why Ketamine? Presentation
WhyWhy Ketamine?Ketamine? JenniferJennifer Davis,Davis, M.D.M.D. HospiceHospice andand PalliativePalliative CareCare CenterCenter MayMay 13,13, 20112011 ObjectivesObjectives BeBe familiarfamiliar withwith thethe pharmacology,pharmacology, dosing,dosing, andand administrationadministration ofof KetamineKetamine UnderstandUnderstand thethe indications,indications, contraindications,contraindications, benefits,benefits, andand sideside effectseffects ofof KetamineKetamine KnowKnow thethe variousvarious usesuses ofof KetamineKetamine andand itsits abuseabuse potentialpotential HistoryHistory DevelopedDeveloped inin earlyearly 1960s1960s andand FDAFDA approvedapproved inin 19701970 FirstFirst usedused inin soldierssoldiers inin VietnamVietnam WarWar forfor warfarewarfare surgicalsurgical proceduresprocedures ClassifiedClassified asas scheduleschedule IIIIII drugdrug AugustAugust 19991999 OutlawedOutlawed inin UnitedUnited KingdomKingdom JanuaryJanuary 20062006 HistoryHistory AccordingAccording toto DEA,DEA, 80%80% seizedseized isis fromfrom MexicoMexico MostMost commonlycommonly usedused inin clubsclubs atat ravesraves 20022002 statistic,statistic, almostalmost 3%3% ofof 1212th gradegrade studentsstudents admittedadmitted toto usingusing ketamineketamine inin thethe lastlast yearyear Rave?Rave? HistoryHistory TheThe ScientistScientist byby JohnJohn LillyLilly JourneysJourneys intointo thethe BrightBright WorldWorld byby MarciaMarcia MooreMoore andand HowardHoward AlltounianAlltounian TheThe EssentialEssential PsychedelicPsychedelic -

Evaluation of Potential Drug Interaction of Analgesic in Cancer
Original Article 1 Pharmaceutical Sciences and Research (PSR), 7(1), 2020, 1 - 8 Evaluation of Potential Drug Interaction of Analgesic in Cancer Patient Receiving Palliative Care in Dharmais Cancer Hospital Eme Stepani Sitepu*, Atika Wahyu Puspitasari, Nuriza Ulul Azmi, Lila Nilam Sari Faculty of Pharmacy, Universitas Indonesia, Depok, Indonesia ABSTRACT Analgesics are mostly used in cancer patients receiving palliative care to improve the quality of life of patients. Besides analgesics, cancer patients receiving palliative care were also given other drugs in combination to overcome other symptoms of cancer, and this combination could potentially cause drug interactions. This study was aimed to analyze the potential of drug interactions with analgesics in cancer patients. The study design was cross-sectional with a retrospective method and descriptive ARTICLE HISTORY study. The sample of this study was cancer palliative care patient’s prescription at Dharmais Cancer Received: August 2019 Hospital in the period of January – December 2017. The sample analyzed in this study consisted of 273 Revised: February 2020 prescriptions. This study found that there were 191 prescriptions (69.9%) of analgesics which potential- Accepted : April 2020 ly interacted with 316 interaction cases. Fentanyl and morphine with 61 cases (19.3%), morphine and gabapentin with 60 cases (18.9%) and morphine and amitriptyline with 33 cases (10.4%) were observed as the three most analgesics-other drugs interaction. Based on severity levels, there were 73.5% of major interaction, 26.3% of moderate interaction, and 0.2% of minor interaction. This study concluded that high occurrence of drug interactions was observed in analgesic drugs, therefore close monitoring is needed in cancer patient receiving palliative care.