(DMXB-A) in a Third Trimester Chronic Ethanol Exposure Model in Rats
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
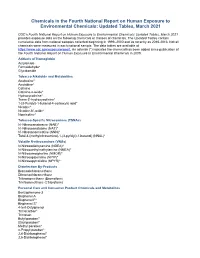
Chemicals in the Fourth Report and Updated Tables Pdf Icon[PDF
Chemicals in the Fourth National Report on Human Exposure to Environmental Chemicals: Updated Tables, March 2021 CDC’s Fourth National Report on Human Exposure to Environmental Chemicals: Updated Tables, March 2021 provides exposure data on the following chemicals or classes of chemicals. The Updated Tables contain cumulative data from national samples collected beginning in 1999–2000 and as recently as 2015-2016. Not all chemicals were measured in each national sample. The data tables are available at https://www.cdc.gov/exposurereport. An asterisk (*) indicates the chemical has been added since publication of the Fourth National Report on Human Exposure to Environmental Chemicals in 2009. Adducts of Hemoglobin Acrylamide Formaldehyde* Glycidamide Tobacco Alkaloids and Metabolites Anabasine* Anatabine* Cotinine Cotinine-n-oxide* Hydroxycotinine* Trans-3’-hydroxycotinine* 1-(3-Pyridyl)-1-butanol-4-carboxylic acid* Nicotine* Nicotine-N’-oxide* Nornicotine* Tobacco-Specific Nitrosamines (TSNAs) N’-Nitrosoanabasine (NAB)* N’-Nitrosoanatabine (NAT)* N’-Nitrosonornicotine (NNN)* Total 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol) (NNAL)* Volatile N-nitrosamines (VNAs) N-Nitrosodiethylamine (NDEA)* N-Nitrosoethylmethylamine (NMEA)* N-Nitrosomorpholine (NMOR)* N-Nitrosopiperidine (NPIP)* N-Nitrosopyrrolidine (NPYR)* Disinfection By-Products Bromodichloromethane Dibromochloromethane Tribromomethane (Bromoform) Trichloromethane (Chloroform) Personal Care and Consumer Product Chemicals and Metabolites Benzophenone-3 Bisphenol A Bisphenol F* Bisphenol -

Molecular Mechanisms Associated with Nicotine Pharmacology and Dependence
Molecular Mechanisms Associated with Nicotine Pharmacology and Dependence Christie D. Fowler, Jill R. Turner, and M. Imad Damaj Contents 1 Introduction 2 Basic Neurocircuitry of Nicotine Addiction 3 Role of Nicotinic Receptors in Nicotine Dependence and Brain Function 4 Modulatory Factors That Influence nAChR Expression and Signaling 5 Genomics and Genetics of Nicotine Dependence 5.1 Overview 5.2 Human and Animal Genetic Studies 5.3 Transcriptionally Adaptive Changes 6 Other Constituents in Nicotine and Tobacco Products Mediating Dependence 7 Therapeutic Approaches for Tobacco and Nicotine Dependence 7.1 Nicotine Replacement Therapies 7.2 Varenicline and Bupropion 7.3 Novel Approaches 8 Conclusion References Abstract Tobacco dependence is a leading cause of preventable disease and death world- wide. Nicotine, the main psychoactive component in tobacco cigarettes, has also C. D. Fowler Department of Neurobiology and Behavior, University of California Irvine, Irvine, CA, USA J. R. Turner Department of Pharmaceutical Sciences, College of Pharmacy, University of Kentucky, Lexington, KY, USA M. Imad Damaj (*) Department of Pharmacology and Toxicology, Virginia Commonwealth University, Richmond, VA, USA Translational Research Initiative for Pain and Neuropathy at VCU, Richmond, VA, USA e-mail: [email protected] # Springer Nature Switzerland AG 2019 Handbook of Experimental Pharmacology, https://doi.org/10.1007/164_2019_252 C. D. Fowler et al. been garnering increased popularity in its vaporized form, as derived from e-cigarette devices. Thus, an understanding of the molecular mechanisms under- lying nicotine pharmacology and dependence is required to ascertain novel approaches to treat drug dependence. In this chapter, we review the field’s current understanding of nicotine’s actions in the brain, the neurocircuitry underlying drug dependence, factors that modulate the function of nicotinic acetylcholine receptors, and the role of specific genes in mitigating the vulnerability to develop nicotine dependence. -

(19) United States (12) Patent Application Publication (10) Pub
US 20130289061A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2013/0289061 A1 Bhide et al. (43) Pub. Date: Oct. 31, 2013 (54) METHODS AND COMPOSITIONS TO Publication Classi?cation PREVENT ADDICTION (51) Int. Cl. (71) Applicant: The General Hospital Corporation, A61K 31/485 (2006-01) Boston’ MA (Us) A61K 31/4458 (2006.01) (52) U.S. Cl. (72) Inventors: Pradeep G. Bhide; Peabody, MA (US); CPC """"" " A61K31/485 (201301); ‘4161223011? Jmm‘“ Zhu’ Ansm’ MA. (Us); USPC ......... .. 514/282; 514/317; 514/654; 514/618; Thomas J. Spencer; Carhsle; MA (US); 514/279 Joseph Biederman; Brookline; MA (Us) (57) ABSTRACT Disclosed herein is a method of reducing or preventing the development of aversion to a CNS stimulant in a subject (21) App1_ NO_; 13/924,815 comprising; administering a therapeutic amount of the neu rological stimulant and administering an antagonist of the kappa opioid receptor; to thereby reduce or prevent the devel - . opment of aversion to the CNS stimulant in the subject. Also (22) Flled' Jun‘ 24’ 2013 disclosed is a method of reducing or preventing the develop ment of addiction to a CNS stimulant in a subj ect; comprising; _ _ administering the CNS stimulant and administering a mu Related U‘s‘ Apphcatlon Data opioid receptor antagonist to thereby reduce or prevent the (63) Continuation of application NO 13/389,959, ?led on development of addiction to the CNS stimulant in the subject. Apt 27’ 2012’ ?led as application NO_ PCT/US2010/ Also disclosed are pharmaceutical compositions comprising 045486 on Aug' 13 2010' a central nervous system stimulant and an opioid receptor ’ antagonist. -

NINDS Custom Collection II
ACACETIN ACEBUTOLOL HYDROCHLORIDE ACECLIDINE HYDROCHLORIDE ACEMETACIN ACETAMINOPHEN ACETAMINOSALOL ACETANILIDE ACETARSOL ACETAZOLAMIDE ACETOHYDROXAMIC ACID ACETRIAZOIC ACID ACETYL TYROSINE ETHYL ESTER ACETYLCARNITINE ACETYLCHOLINE ACETYLCYSTEINE ACETYLGLUCOSAMINE ACETYLGLUTAMIC ACID ACETYL-L-LEUCINE ACETYLPHENYLALANINE ACETYLSEROTONIN ACETYLTRYPTOPHAN ACEXAMIC ACID ACIVICIN ACLACINOMYCIN A1 ACONITINE ACRIFLAVINIUM HYDROCHLORIDE ACRISORCIN ACTINONIN ACYCLOVIR ADENOSINE PHOSPHATE ADENOSINE ADRENALINE BITARTRATE AESCULIN AJMALINE AKLAVINE HYDROCHLORIDE ALANYL-dl-LEUCINE ALANYL-dl-PHENYLALANINE ALAPROCLATE ALBENDAZOLE ALBUTEROL ALEXIDINE HYDROCHLORIDE ALLANTOIN ALLOPURINOL ALMOTRIPTAN ALOIN ALPRENOLOL ALTRETAMINE ALVERINE CITRATE AMANTADINE HYDROCHLORIDE AMBROXOL HYDROCHLORIDE AMCINONIDE AMIKACIN SULFATE AMILORIDE HYDROCHLORIDE 3-AMINOBENZAMIDE gamma-AMINOBUTYRIC ACID AMINOCAPROIC ACID N- (2-AMINOETHYL)-4-CHLOROBENZAMIDE (RO-16-6491) AMINOGLUTETHIMIDE AMINOHIPPURIC ACID AMINOHYDROXYBUTYRIC ACID AMINOLEVULINIC ACID HYDROCHLORIDE AMINOPHENAZONE 3-AMINOPROPANESULPHONIC ACID AMINOPYRIDINE 9-AMINO-1,2,3,4-TETRAHYDROACRIDINE HYDROCHLORIDE AMINOTHIAZOLE AMIODARONE HYDROCHLORIDE AMIPRILOSE AMITRIPTYLINE HYDROCHLORIDE AMLODIPINE BESYLATE AMODIAQUINE DIHYDROCHLORIDE AMOXEPINE AMOXICILLIN AMPICILLIN SODIUM AMPROLIUM AMRINONE AMYGDALIN ANABASAMINE HYDROCHLORIDE ANABASINE HYDROCHLORIDE ANCITABINE HYDROCHLORIDE ANDROSTERONE SODIUM SULFATE ANIRACETAM ANISINDIONE ANISODAMINE ANISOMYCIN ANTAZOLINE PHOSPHATE ANTHRALIN ANTIMYCIN A (A1 shown) ANTIPYRINE APHYLLIC -

Biomarkers of Exposure Among Adult Smokeless Tobacco Users in the Population Assessment of Tobacco and Health Study (Wave 1, 2013-14)
Author Manuscript Published OnlineFirst on January 27, 2020; DOI: 10.1158/1055-9965.EPI-19-0766 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Biomarkers of Exposure among Adult Smokeless Tobacco Users in the Population Assessment of Tobacco and Health Study (Wave 1, 2013-14) Running Title: Biomarkers of Exposure in PATH Study Smokeless Tobacco Users Yu-Ching Cheng1, Carolyn M. Reyes-Guzman1,2, Carol H. Christensen1, Brian L. Rostron1, Kathryn C. Edwards3, Lanqing Wang4, Jun Feng4, Jeffery M. Jarrett4, Cynthia D. Ward 4, Baoyun Xia4, Heather L. Kimmel5, Kevin Conway5, Carmine Leggett1, Kristie Taylor3, Charlie Lawrence3, Ray Niaura6, Mark J. Travers7, Andrew Hyland7, Stephen S. Hecht8, Dorothy K. Hatsukami8, Maciej L. Goniewicz7, Nicolette Borek1, Benjamin C. Blount4, Dana M. van Bemmel1 1Center for Tobacco Products, Food and Drug Administration, MD, USA, 2National Cancer Institute, National Institutes of Health, MD, USA, 3Westat, MD, USA, 4US Centers for Disease Control and Prevention, USA, 5National Institute on Drug Abuse, National Institutes of Health, MD, USA, 6New York University College of Global Public Health, NY, USA, 7Roswell Park Cancer Institute, NY, USA, 8University of Minnesota, Masonic Cancer Center, USA. Key Words: biomarkers of exposure, smokeless tobacco Corresponding author: Yu-Ching Cheng, PhD 11785 Beltsville Drive, RM 8321 Beltsville, MD 20705 [email protected] 240-402-5957 1 Downloaded from cebp.aacrjournals.org on October 1, 2021. © 2020 American Association for Cancer Research. Author Manuscript Published OnlineFirst on January 27, 2020; DOI: 10.1158/1055-9965.EPI-19-0766 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. -

7 Nicotinic Receptor Agonists
CORE Metadata, citation and similar papers at core.ac.uk Provided by PubMed Central The Open Medicinal Chemistry Journal, 2010, 4, 37-56 37 Open Access 7 Nicotinic Receptor Agonists: Potential Therapeutic Drugs for Treatment of Cognitive Impairments in Schizophrenia and Alzheimer’s Disease Jun Toyohara, and Kenji Hashimoto* Division of Clinical Neuroscience, Chiba University Center for Forensic Mental Health, Chiba, Japan Abstract: Accumulating evidence suggests that 7 nicotinic receptors (7 nAChRs), a subtype of nAChRs, play a role in the pathophysiology of neuropsychiatric diseases, including schizophrenia and Alzheimer’s disease (AD). A number of psychopharmacological and genetic studies shown that 7 nAChRs play an important role in the deficits of P50 auditory evoked potential in patients with schizophrenia, and that 7 nAChR agonists would be potential therapeutic drugs for cognitive impairments associated with P50 deficits in schizophrenia. Furthermore, some studies have demonstrated that 7 nAChRs might play a key role in the amyloid- (A)-mediated pathology of AD, and that 7 nAChR agonists would be potential therapeutic drugs for A deposition in the brains of patients with AD. Interestingly, the altered expression of 7 nAChRs in the postmortem brain tissues from patients with schizophrenia and AD has been reported. Based on all these findings, selective 7 nAChR agonists can be considered potential therapeutic drugs for cognitive impairments in both schizophrenia and AD. In this article, we review the recent research into the role of 7 nAChRs in the pathophysiology of these diseases and into the potential use of novel 7 nAChR agonists as therapeutic drugs. Keywords: 7 Nicotinic receptors, Cognition, Schizophrenia, Alzheimer’s disease. -
Nicotinic Acetylcholine Receptor Signaling in Neuroprotection
Akinori Akaike · Shun Shimohama Yoshimi Misu Editors Nicotinic Acetylcholine Receptor Signaling in Neuroprotection Nicotinic Acetylcholine Receptor Signaling in Neuroprotection Akinori Akaike • Shun Shimohama Yoshimi Misu Editors Nicotinic Acetylcholine Receptor Signaling in Neuroprotection Editors Akinori Akaike Shun Shimohama Department of Pharmacology, Graduate Department of Neurology, School of School of Pharmaceutical Sciences Medicine Kyoto University Sapporo Medical University Kyoto, Japan Sapporo, Hokkaido, Japan Wakayama Medical University Wakayama, Japan Yoshimi Misu Graduate School of Medicine Yokohama City University Yokohama, Kanagawa, Japan ISBN 978-981-10-8487-4 ISBN 978-981-10-8488-1 (eBook) https://doi.org/10.1007/978-981-10-8488-1 Library of Congress Control Number: 2018936753 © The Editor(s) (if applicable) and The Author(s) 2018. This book is an open access publication. Open Access This book is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made. The images or other third party material in this book are included in the book’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the book’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. The use of general descriptive names, registered names, trademarks, service marks, etc. -

With Amantadine
CHARACTERIZATION OF RENAL CATIONIC DRUG TRANSPORT WITH AMANTADINE BY LEO T. Y. WONG A Tnrsrs SuslrrmEo ro rHE Fecurrv or Gn¡ouer¡ Sruoles tN P¿nr¡er- Fulrlnu¡NT oF THE R¡eutRptttn¡¡-rs ronr¡mD¡GREE oF DOCTOR OF PHIT,OSOPFTY Dpp¡nrue¡rr or PrunuacoI-ocy & THrn¡pEUTrcs Facurrv orMeotcl¡¡¡ UNrvensrrv on M¡Nrros¿ WrNNrno, Maì¡rrone R3E 0W3 C¡,N¡oe DecBr'an¡n 199L ¡.L Bibliothèque nationale E*E |'t:îå'o'Jo'"t du Canada Acquisitions and Direction des acquisitions et Bibliographic Services Branch des services bibliographiques 395 Wellington Street 395, rue Wellington Ottawa, Ontario Ottawa (Ontar¡o) K1A ON4 K1A ON4 Yout lile Volrc relërence Oú lile Nolrc relércnce The author has granted an L'auteur a accordé une licence irrevocable non-exclus¡ve licence irrévocable et non exclusive allowing the National Library of permettant à la Bibliothèque Canada to reproduce, loan, nationale du Canada de distribute or sell cop¡es of reproduire, prêter, distribuer ou his/her thesis by any means and vendre des copies de sa thèse in any form or format, making de quelque manière et sous this thesis available to interested quelque forme que ce soit pour persons. mettre des exemplaires de cette thèse à la disposition des personnes intéressées. The author retains ownership of L'auteur conserve la propriété du the copyright in his/her thesis. droit d'auteur qu¡ protège sa Neither the thesis nor substantial thèse. Ni la thèse ni des extraits extracts from it may be printed or substantiels de celle-ci ne otherwise reproduced without doivent être imprimés ou his/her permission. -

Solanum Alkaloids and Their Pharmaceutical Roles: a Review
Journal of Analytical & Pharmaceutical Research Solanum Alkaloids and their Pharmaceutical Roles: A Review Abstract Review Article The genus Solanum is treated to be one of the hypergenus among the flowering epithets. The genus is well represented in the tropical and warmer temperate Volume 3 Issue 6 - 2016 families and is comprised of about 1500 species with at least 5000 published Solanum species are endemic to the northeastern region. 1Department of Botany, India Many Solanum species are widely used in popular medicine or as vegetables. The 2Department of Botany, Trivandrum University College, India presenceregions. About of the 20 steroidal of these alkaloid solasodine, which is potentially an important starting material for the synthesis of steroid hormones, is characteristic of *Corresponding author: Murugan K, Plant Biochemistry the genus Solanum. Soladodine, and its glocosylated forms like solamargine, and Molecular Biology Lab, Department of Botany, solosonine and other compounds of potential therapeutic values. India, Email: Keywords: Solanum; Steroidal alkaloid; Solasodine; Hypergenus; Glocosylated; Trivandrum University College, Trivandrum 695 034, Kerala, Injuries; Infections Received: | Published: October 21, 2016 December 15, 2016 Abbreviations: TGA: Total Glycoalkaloid; SGA: Steroidal range of biological activities such as antimicrobial, antirheumatics, Glycoalkaloid; SGT: Sergeant; HMG: Hydroxy Methylglutaryl; LDL: Low Density Lipoprotein; ACAT: Assistive Context Aware Further, these alkaloids are of paramount importance in drug Toolkit; HMDM: Human Monocyte Derived Macrophage; industriesanticonvulsants, as they anti-inflammatory, serve as precursors antioxidant or lead molecules and anticancer. for the synthesis of many of the steroidal drugs which have been used CE: Cholesterol Ester; CCl4: Carbon Tetrachloride; 6-OHDA: 6-hydroxydopamine; IL: Interleukin; TNF: Tumor Necrosis Factor; DPPH: Diphenyl-2-Picryl Hydrazyl; FRAP: Fluorescence treatments. -

Neuronal Nicotinic Receptors
NEURONAL NICOTINIC RECEPTORS Dr Christopher G V Sharples and preparations lend themselves to physiological and pharmacological investigations, and there followed a Professor Susan Wonnacott period of intense study of the properties of nAChR- mediating transmission at these sites. nAChRs at the Department of Biology and Biochemistry, muscle endplate and in sympathetic ganglia could be University of Bath, Bath BA2 7AY, UK distinguished by their respective preferences for C10 and C6 polymethylene bistrimethylammonium Susan Wonnacott is Professor of compounds, notably decamethonium and Neuroscience and Christopher Sharples is a hexamethonium,5 providing the first hint of diversity post-doctoral research officer within the among nAChRs. Department of Biology and Biochemistry at Biochemical approaches to elucidate the structure the University of Bath. Their research and function of the nAChR protein in the 1970’s were focuses on understanding the molecular and facilitated by the abundance of nicotinic synapses cellular events underlying the effects of akin to the muscle endplate, in electric organs of the acute and chronic nicotinic receptor electric ray,Torpedo , and eel, Electrophorus . High stimulation. This is with the goal of affinity snakea -toxins, principallyaa -bungarotoxin ( - Bgt), enabled the nAChR protein to be purified, and elucidating the structure, function and subsequently resolved into 4 different subunits regulation of neuronal nicotinic receptors. designateda ,bg , and d .6 An additional subunit, e , was subsequently identified in adult muscle. In the early 1980’s, these subunits were cloned and sequenced, The nicotinic acetylcholine receptor (nAChR) arguably and the era of the molecular analysis of the nAChR has the longest history of experimental study of any commenced. -

Bioactive Marine Drugs and Marine Biomaterials for Brain Diseases
Mar. Drugs 2014, 12, 2539-2589; doi:10.3390/md12052539 OPEN ACCESS marine drugs ISSN 1660–3397 www.mdpi.com/journal/marinedrugs Review Bioactive Marine Drugs and Marine Biomaterials for Brain Diseases Clara Grosso 1, Patrícia Valentão 1, Federico Ferreres 2 and Paula B. Andrade 1,* 1 REQUIMTE/Laboratory of Pharmacognosy, Department of Chemistry, Faculty of Pharmacy, University of Porto, Rua de Jorge Viterbo Ferreira, no. 228, 4050-313 Porto, Portugal; E-Mails: [email protected] (C.G.); [email protected] (P.V.) 2 Research Group on Quality, Safety and Bioactivity of Plant Foods, Department of Food Science and Technology, CEBAS (CSIC), P.O. Box 164, Campus University Espinardo, Murcia 30100, Spain; E-Mail: [email protected] * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +351-22042-8654; Fax: +351-22609-3390. Received: 30 January 2014; in revised form: 10 April 2014 / Accepted: 16 April 2014 / Published: 2 May 2014 Abstract: Marine invertebrates produce a plethora of bioactive compounds, which serve as inspiration for marine biotechnology, particularly in drug discovery programs and biomaterials development. This review aims to summarize the potential of drugs derived from marine invertebrates in the field of neuroscience. Therefore, some examples of neuroprotective drugs and neurotoxins will be discussed. Their role in neuroscience research and development of new therapies targeting the central nervous system will be addressed, with particular focus on neuroinflammation and neurodegeneration. In addition, the neuronal growth promoted by marine drugs, as well as the recent advances in neural tissue engineering, will be highlighted. Keywords: aragonite; conotoxins; neurodegeneration; neuroinflammation; Aβ peptide; tau hyperphosphorylation; protein kinases; receptors; voltage-dependent ion channels; cyclooxygenases Mar. -

The Relationship Between Nicotine and Body Weight: Implications for Tobacco Regulatory Policy from Rats & Humans
THE RELATIONSHIP BETWEEN NICOTINE AND BODY WEIGHT: IMPLICATIONS FOR TOBACCO REGULATORY POLICY FROM RATS & HUMANS by Laura Eloise Rupprecht Bachelor of Science, Juniata College, 2010 Submitted to the Graduate Faculty of the Deitrich School of Arts and Sciences in partial fulfillment of the requirements for the degree of Doctor of Philosophy University of Pittsburgh 2017 UNIVERSITY OF PITTSBURGH DEITRICH SCHOOL OF ARTS AND SCIENCES This dissertation was presented by Laura Eloise Rupprecht It was defended on March 29, 2017 and approved by Judy L. Cameron, Professor, Psychiatry Eric C. Donny, Professor, Psychology Mary M. Torregrossa, Assistant Professor, Psychiatry Julie A. Blendy, Professor, University of Pennsylvania, Pharmacology Dissertation Advisor: Alan F. Sved, Chairman and Professor, Neuroscience Dissertation Chair: Linda Rinaman, Professor, Neuroscience ii Copyright © by Laura Eloise Rupprecht 2017 iii THE RELATIONSHIP BETWEEN NICOTINE AND BODY WEIGHT: IMPLICATIONS FOR TOBACCO REGULATORY POLICY FROM RATS & HUMANS Laura Eloise Rupprecht, PhD University of Pittsburgh, 2017 Smokers weigh less than non-smokers and former smokers, an observation that has been attributed to nicotine in cigarette smoke. Despite the ability of nicotine to suppress weight gain, body mass index (BMI) is positively associated with smoking intensity. These phenomena suggest a complex relationship between nicotine and body weight: that nicotine impacts body weight, and that body weight may modify nicotine reinforcement. This dissertation tests the hypotheses that self-administered nicotine suppresses body weight and that body weight impacts nicotine reinforcement in rats and human smokers. Experiments tested these hypotheses in a rat model of nicotine self-administration and in human smokers. Experiments in Chapter 2 demonstrate that self-administered nicotine suppressed body weight gain independent of food intake in rats.