Update on Electrocardiographic Data in Junctional Rhythm
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinical Significance of Exit Block*
Clinical Significance of Exit Block* IRANY M. DE AZEVEDO, M.D. YOSHIO WATANABE, M.D. LEONARD S. DREIFUS, M.D. From the Departments of Medicine, Physiology, and Biophysics, Hahnemann Medical College, Philadelphia, Pennsylvania The confinement of an ectopic discharge to its ily reserved for ectopic pacemakers, rather than the focus, and its consequent inability to invade the ad sinus node. jacent myocardium when falling outside of the re High Grade Atrioventricular Block. In vi rtu fractory period of the heart, is a well established ally all instances, exit block occurs in the presence phenomenon called "exit block." This cardiac ar of higher degrees of A-V block. Failure of the rhythmia was originally described by Kaufmann impulse to propagate from the subsidiary ectopic and Rothberger ( 8) to explain the failure of a para focus to either the ventricles, atria, or both is char systolic focus to activate the heart. All pacemakers acteristic of this form of exit block. Several exam are subject to exit block (9, 13, 15, 14, 11 , 16, 12, ples are illustrated. In figure 2, there is high grade 3, 10, 7, 1), however, by convention, conduction A-V block causing A-V dissociation. The atria are disturbances involving the sinus node (S-A block) under the control of the sinus node at a rate of 71 are usually excluded from this concept, and the term per minute, and the ventricles are controlled by a is reserved for ectopic pacemakers. Recent electro subsidiary ectopic pacemaker, probably originating physiological and clinical studies have shown that in the right bundle branch at a rate of approximately exit block may complicate reentrant arrhythmias and 40 per minute. -

Wide Flbs & QRS Tachycardias
Wide FLB’s and QRS Tachycardias Reading Assignment (p30-41 and 42-44) Welcome to the “5-Step Method” ECG #: Mearurements: Rhythm (s): Conduction: Waveform: Interpretation: A= V= PR= QRS= QT= Axis= 1. Compute the 5 basic measurements: HR, PR interval, QRS duration, QT interval, Axis 2. What’s the basic rhythm and other rhythm statements (e.g., PACs and PVC’s) 3. Any conduction abnormalities (SA blocks, AV blocks (Types I or II), and IV blocks 4. Waveform abnormalities beginning with P waves, QRS complexes, ST-T, and U waves 5. Final interpretations: Normal ECG or Borderline or Abnormal ECG (list final conclusions) 44 Year old man in the ER with palpitations and lightheadedness 7-1 rsR’ Mearurements: Rhythm (s): Conduction: Waveform: Interpretation: A= V=210 Wide QRS tachycardia • IVCD • rsR‘ in V1 Abnormal ECG: • Late S (rightward forces) in 1. High probability SVT with RBBB PR= I, aVL, V6 Clues: classic triphasic (rsR‘) RBBB QRS=1120 morphology in V1 is very unlikely to be VT. The most likely SVT mechanism in this QT=240 ECG is AVNRT with RBBB. 7-1 Axis= indeterminate 65 Year old man in the ICU with hypotension 7-2 qR in V1 rS in V6 Mearurements: Rhythm (s): Conduction: Waveform: Interpretation: A= V=140 Wide QRS tachycardia • IVCD • Northwest quadrant axis Abnormal ECG: (lead I and II both negative) • Left ventricular tachycardia PR= • qR pattern in V1 • rS pattern in V6 ECG Clues for VT in this case: 1) NW QRS=150 quadrant axis; 2) qR in V1; rS in V6. QT=340 Clinical clues: hypotension 7-2 Axis= -120 (NW Quadrant) I II III 7-3 75 Year old man in the ICU with recent acute coronary syndrome Mearurements: Rhythm (s): Conduction: Waveform: Interpretation: A= V= 135 Wide QRS tachycardia • IVCD • fat R in V1 (red arrows) Abnormal ECG: • Notch on downstroke of S 1. -

Accelerated Junctional Rhythm on a Routine Electrocardiogram: an Unusual Presentation of Cardiac Sarcoidosis
10 The Open Cardiovascular Imaging Journal, 2011, 3, 10-12 Open Access Accelerated Junctional Rhythm on a Routine Electrocardiogram: An Unusual Presentation of Cardiac Sarcoidosis Srikanth Seethalaa, Kara Albrightb, Srinivasa V. Jampanab and Jan Nmec*,c aDepartment of Internal Medicine, Texas Tech University Health Sciences Center-El Paso; bUniversity of Pittsburgh- MedicalCenters-MercyHospital; cCardiovascular Institute, University of Pittsburgh, 200 Lothrop St, Pittsburgh, PA 15213, USA Abstract: Cardiac sarcoidosis is an uncommon cause of cardiac arrhythmias and cardiomyopathy. We describe a case of cardiac sarcoidosis presenting as an accelerated junctional rhythm and complete atrioventricular (AV) block, without se- vere left ventricular (LV) dysfunction or pulmonary symptoms. Computer tomography (CT) of the chest and mediastinal lymph node biopsy confirmed the diagnosis. Dual-chamber implantable cardioverter-defibrillator was implanted due to reported risk of sudden cardiac death due to ventricular tachyarrhythmia despite negative programmed ventricular stimula- tion. Keywords: Cardiac sarcoidosis, Accelerated junctional rhythm, AV block. CASE REPORT: Placement of dual-chamber pacemaker was considered because of probably symptomatic complete heart block. An A 66-year old male was noted to have an abnormal elec- echocardiogram repeated prior to pacemaker implantation trocardiogram (ECG) during a routine insurance exam. again showed low-normal left ventricular ejection fraction Subsequent ECG obtained in his primary care physician’s (LVEF) with regional wall motion abnormalities and mild office revealed junctional rhythm at 56 beats/minute (bpm) LV enlargement (LV diastolic diameter of 60 mm). and a slightly faster sinus rhythm with atrioventricular (AV) dissociation, suggestive of possible heart block (Fig. 1a). An A baseline chest roentgenogram (CXR) performed on the ECG obtained during another office visit again showed AV day of the device placement (Fig. -

Basic Rhythm Recognition
Electrocardiographic Interpretation Basic Rhythm Recognition William Brady, MD Department of Emergency Medicine Cardiac Rhythms Anatomy of a Rhythm Strip A Review of the Electrical System Intrinsic Pacemakers Cells These cells have property known as “Automaticity”— means they can spontaneously depolarize. Sinus Node Primary pacemaker Fires at a rate of 60-100 bpm AV Junction Fires at a rate of 40-60 bpm Ventricular (Purkinje Fibers) Less than 40 bpm What’s Normal P Wave Atrial Depolarization PR Interval (Normal 0.12-0.20) Beginning of the P to onset of QRS QRS Ventricular Depolarization QRS Interval (Normal <0.10) Period (or length of time) it takes for the ventricles to depolarize The Key to Success… …A systematic approach! Rate Rhythm P Waves PR Interval P and QRS Correlation QRS Rate Pacemaker A rather ill patient……… Very apparent inferolateral STEMI……with less apparent complete heart block RATE . Fast vs Slow . QRS Width Narrow QRS Wide QRS Narrow QRS Wide QRS Tachycardia Tachycardia Bradycardia Bradycardia Regular Irregular Regular Irregular Sinus Brady Idioventricular A-Fib / Flutter Bradycardia w/ BBB Sinus Tach A-Fib VT PVT Junctional 2 AVB / II PSVT A-Flutter SVT aberrant A-Fib 1 AVB 3 AVB A-Flutter MAT 2 AVB / I or II PAT PAT 3 AVB ST PAC / PVC Stability Hypotension / hypoperfusion Altered mental status Chest pain – Coronary ischemic Dyspnea – Pulmonary edema Sinus Rhythm Sinus Rhythm P Wave PR Interval QRS Rate Rhythm Pacemaker Comment . Before . Constant, . Rate 60-100 . Regular . SA Node Upright in each QRS regular . Interval =/< leads I, II, . Look . Interval .12- .10 & III alike .20 Conduction Image reference: Cardionetics/ http://www.cardionetics.com/docs/healthcr/ecg/arrhy/0100_bd.htm Sinus Pause A delay of activation within the atria for a period between 1.7 and 3 seconds A palpitation is likely to be felt by the patient as the sinus beat following the pause may be a heavy beat. -

Rhythms & Cardiac Emergencies
Rhythm & 12 Lead EKG Review March 2011 CE Condell Medical Center EMS System Site code # 107200E-1211 Prepared by: FF/PMD Michael Mounts – Lake Forest Fire Revised By: Sharon Hopkins, RN, BSN, EMT-P Objectives Upon successful completion of this module, the EMS provider will be able to: • Identify the components of a rhythm strip • Identify what the components represent on the rhythm strip • Identify criteria for sinus rhythms • Identify criteria for atrial rhythms • Identify AV/junctional rhythms Objectives cont. • Identify ventricular rhythms • Identify rhythms with AV blocks • Identify treatments for different rhythms • Identify criteria for identification of ST elevation on 12 lead EKG’s • Identify EMS treatment for patients with acute coronary syndrome (ST elevation) • Demonstrate standard & alternate placement of ECG electrodes for monitoring Objectives cont. • Demonstrate placement of electrodes for obtaining a 12 lead EKG • Demonstrate the ability to identify a variety of static or dynamic EKG rhythm strips • Demonstrate the ability to identify the presence or absence of ST elevation when presented with a 12 lead EKG • Review department’s process to transmit 12 lead EKG to hospital, if capable • Successfully complete the post quiz with a score of 80% or better. ECG Paper • What do the boxes represent? • How do you measure time & amplitude? Components of the Rhythm Strip • ECG Paper • Wave forms • Wave complexes • Wave segments • Wave intervals Wave Forms, Complexes, Segments & Intervals • P wave – atrial depolarization • QRS – Ventricular -

View Pdf Copy of Original Document
Phenotype definition for the Vanderbilt Genome-Electronic Records project Identifying genetics determinants of normal QRS duration (QRSd) Patient population: • Patients with DNA whose first electrocardiogram (ECG) is designated as “normal” and lacking an exclusion criteria. • For this study, case and control are drawn from the same population and analyzed via continuous trait analysis. The only difference will be the QRSd. Hypothetical timeline for a single patient: Notes: • The study ECG is the first normal ECG. • The “Mildly abnormal” ECG cannot be abnormal by presence of heart disease. It can have abnormal rate, be recorded in the presence of Na-channel blocking meds, etc. For instance, a HR >100 is OK but not a bundle branch block. • Y duration = from first entry in the electronic medical record (EMR) until one month following normal ECG • Z duration = most recent clinic visit or problem list (if present) to one week following the normal ECG. Labs values, though, must be +/- 48h from the ECG time Criteria to be included in the analysis: Criteria Source/Method “Normal” ECG must be: • QRSd between 65-120ms ECG calculations • ECG designed as “NORMAL” ECG classification • Heart Rate between 50-100 ECG calculations • ECG Impression must not contain Natural Language Processing (NLP) on evidence of heart disease concepts (see ECG impression. Will exclude all but list below) negated terms (e.g., exclude those with possible, probable, or asserted bundle branch blocks). Should also exclude normalization negations like “LBBB no longer present.” -

The Spectrum of COVID-19-Associated Myocarditis: a Patient-Tailored Multidisciplinary Approach
Journal of Clinical Medicine Article The Spectrum of COVID-19-Associated Myocarditis: A Patient-Tailored Multidisciplinary Approach Giovanni Peretto 1,2,3,*, Andrea Villatore 3 , Stefania Rizzo 4, Antonio Esposito 2,3,5, Giacomo De Luca 2,6, Anna Palmisano 2,5, Davide Vignale 2,5, Alberto Maria Cappelletti 7, Moreno Tresoldi 8,9, Corrado Campochiaro 2,6 , Silvia Sartorelli 2,6, Marco Ripa 9,10 , Monica De Gaspari 4 , Elena Busnardo 2,11, Paola Ferro 11, Maria Grazia Calabrò 12, Evgeny Fominskiy 12 , Fabrizio Monaco 12 , Giulio Cavalli 6, Luigi Gianolli 11, Francesco De Cobelli 3,5 , Alberto Margonato 7, Lorenzo Dagna 3,6, Mara Scandroglio 12, Paolo Guido Camici 3, Patrizio Mazzone 1, Paolo Della Bella 1, Cristina Basso 4 and Simone Sala 1,2 1 Department of Cardiac Electrophysiology and Arrhythmology, IRCCS San Raffaele Scientific Institute, 20132 Milan, Italy; [email protected] (P.M.); [email protected] (P.D.B.); [email protected] (S.S.) 2 Myocarditis Disease Unit, IRCCS San Raffaele Scientific Institute, 20132 Milan, Italy; [email protected] (A.E.); [email protected] (G.D.L.); [email protected] (A.P.); [email protected] (D.V.); [email protected] (C.C.); [email protected] (S.S.); [email protected] (E.B.) 3 School of Medicine, San Raffaele Vita-Salute University, 20132 Milan, Italy; [email protected] (A.V.); [email protected] (F.D.C.); [email protected] (L.D.); [email protected] (P.G.C.) 4 Department of Cardiac Thoracic Vascular Sciences and Public Health, -

Wolff - Parkinson-White Syndrome Presenting As Atrial Fibrillation with Broad-QRS Complexes
Journal of College of Medical Sciences-Nepal,2010,Vol-6,No-3, 52-57 Case Report Wolff - Parkinson-White syndrome presenting as atrial fibrillation with broad-QRS complexes M.P. Gautam1, L. Thapa2, S. Gautam3 Department of Cardiology1, Department of Neurology2, Department of Internal medicine3 College of Medical Sciences, Bharatpur, Chitwan, Nepal Abstract The Wolff-Parkinson-White (WPW) syndrome is the commonest form of ventricular pre-excitation and is characterised by the presence of an accessory pathway between atria and ventricles. The term WPW syndrome is applied to patients with both pre-excitation on the ECG and paroxysmal tachycardia. Usually the conducting properties of bypass tracts and the AV node differ, the ventricular response during atrial flutter or fibrillation may be unusually rapid and may cause ventricular fibrillation. Atrial fibrillation (AF) is not an uncommon presentation in emergency department. Moreover, AF associated with WPW syndrome as an underlying condition is also not a rare occurrence; it is seen in 20-25% of WPW Syndrome. Recognition of this condition is very crucial in terms of emergency management. Its early recognition and initial treatment allows rapid restoration to sinus rhythm. Acute management of WPW syndrome with atrial fibrillation with hypotension is DC cardioversion. In haemodynamically stable patients, the drugs of choice are Amiodarone and class Ic anti- arrhythmic agents. Key words: Paroxysmal tachycardias, pre-excitation, tachycardia. Introduction Conduction from the atria to the ventricles syndrome (WPW) is the commonest form of ventricular normally occurs via the atrio-ventricular node (AV)- pre-excitation. It is characterised by the presence His-Purkinje system. Patients with a pre-excitation WPW pattern of electrocardiographic (ECG) changes Syndrome have an additional or alternative pathway, and paroxysmal tachycardia. -

Day 9: Rhythms: Cardiac Arrhythmias
1. 2. 1. 1. Sinus rhythm @ ~90 bpm (arrows) 2. Junctional escape rhythm (50 bpm) with LBBB 3. Complete AV dissociation (due to 3rd degree AV block) 2. 1. Sinus rhythm 80 bpm) 2. Type II (Mobitz) 2nd degree AV block with 3:2 and 2:1 conduction 3. RBBB V1 3. 4. II V1 * * 3. 1. Sinus rhythm @ 75 bpm (arrows); 2 sinus captures (*) with RBBB aberration 2. Accelerated junctional rhythm @ 80 bpm 3. Incomplete AV dissociation due to the faster junctional rhythm; note: there is no AV block; the sinus captures whenever there is an opportunity for conduction. * * * 4. II Sinus rhythm with nonconducted PAC’s (*) in a pattern of bigeminy 5. V1 6. * * * 5. V1 1. Normal sinus rhythm (PR=220ms, QRS=120 ms) 2. Late (i.e., end-diastolic) PVC’s (*) of LV origin rsR’ 6. 1. Atrial fibrillation with one aberrantly conducted (RBBB) beat (note long cycle-short cycle rule of aberrancy, aka Ashman phenomenon) 7. V1 8. V1 7. V1 * * 1. Sinus rhythm (~70 bpm) with 2 nonconducted PAC’s (arrows) 2. Aborted 2nd degree AV block (Type I); note the PAC’s are early and they reset the sinus timing) 3. Two junctional escapes (*) 8. V1 Atrial flutter (240 bpm) with variable conduction V1 9. 10. V1 V1 9. 2:1 3:1 1. Sinus tachycardia (105 bpm) 2. 2nd degree AV block (type II); note 2:1 and 3:1 conduction ratios 3. LBBB * * * * 10. 2:1 AVB V1 F 1. Sinus rhythm (75 bpm) 2. 2nd degree AV block (2:1 conduction) with RBBB (it’s Mobitz II because the last beat has same PR interval ) 3. -
ACLS Rhythms for the ACLS Algorithms
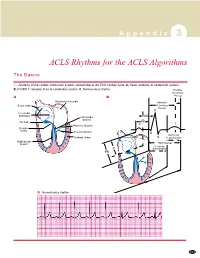
A p p e n d i x 3 ACLS Rhythms for the ACLS Algorithms The Basics 1. Anatomy of the cardiac conduction system: relationship to the ECG cardiac cycle. A, Heart: anatomy of conduction system. B, P-QRS-T complex: lines to conduction system. C, Normal sinus rhythm. Relative Refractory A B Period Bachmann’s bundle Absolute Sinus node Refractory Period R Internodal pathways Left bundle AVN branch AV node PR T Posterior division P Bundle of His Anterior division Q Ventricular Purkinje fibers S Repolarization Right bundle branch QT Interval Ventricular P Depolarization PR C Normal sinus rhythm 253 A p p e n d i x 3 The Cardiac Arrest Rhythms 2. Ventricular Fibrillation/Pulseless Ventricular Tachycardia Pathophysiology ■ Ventricles consist of areas of normal myocardium alternating with areas of ischemic, injured, or infarcted myocardium, leading to chaotic pattern of ventricular depolarization Defining Criteria per ECG ■ Rate/QRS complex: unable to determine; no recognizable P, QRS, or T waves ■ Rhythm: indeterminate; pattern of sharp up (peak) and down (trough) deflections ■ Amplitude: measured from peak-to-trough; often used subjectively to describe VF as fine (peak-to- trough 2 to <5 mm), medium-moderate (5 to <10 mm), coarse (10 to <15 mm), very coarse (>15 mm) Clinical Manifestations ■ Pulse disappears with onset of VF ■ Collapse, unconsciousness ■ Agonal breaths ➔ apnea in <5 min ■ Onset of reversible death Common Etiologies ■ Acute coronary syndromes leading to ischemic areas of myocardium ■ Stable-to-unstable VT, untreated ■ PVCs with -

Non-Sinus Bradyarrhythmias in Very Low Birth Weight Infants
Journal of Perinatology (2007) 27,65–67 r 2007 Nature Publishing Group All rights reserved. 0743-8346/07 $30 www.nature.com/jp PERINATAL/NEONATAL CASE PRESENTATION Non-sinus bradyarrhythmias in very low birth weight infants YD Gamble, WP Lutin and OP Mathew Department of Pediatrics, Sections of Neonatology and Pediatric cardiology, Medical College of Georgia, Augusta, GA, USA min and oxygen saturation less than 85% were considered Transient bradycardias occur frequently in preterm infants with apnea of clinically significant and further reviewed. Segments of the stored prematurity. However, occurrence of non-sinus bradyarrhythmias in very 24-h waveforms meeting one or both criteria were displayed, low birth weight (VLBW) infants has received very little attention. This case amplified if necessary and analyzed during the study period of 6 series documents transient bradyarrhythmias in VLBW infants. Most months. Isolated abnormal beats such as premature atrial and frequently observed arrhythmia was a non-sinus atrial rhythm followed by ventricular contractions were not evaluated. Only periods without junctional escape rhythm. Ventricular rhythm with wide QRS complexes artifacts were considered for analysis. Periods with movement occurred rarely. The majority of these episodes occurred in the absence of artifacts as indicated by changes in baseline, lack of clarity of EKG oxygen desaturation. Increase in vagal tone is presumed to mediate this signals due to increased muscle activity or loss of signal were response. excluded from analysis. Our ability to amplify the signal assured Journal of Perinatology (2007) 27, 65–67. doi:10.1038/sj.jp.7211623 that the quality of EKG signal was adequate for the intended Keywords: cardiac arrhythmia; prematurity; aphea purpose. -

Dysrhythmias
CARDIOVASCULAR DISORDERS DYSRHYTHMIAS I. BASIC PRINCIPLES OF CARDIAC CONDUCTION DISTURBANCES A. Standard ECG and rhythm strips 1. Recordings are obtained at a paper speed of 25 mm/sec. 2. The vertical axis measures distance; the smallest divisions are 1 mm ×1 mm. 3. The horizontal axis measures time; each small division is 0.04 sec/mm. B. Normal morphology Courtesy of Dr. Michael McCrea 1. P wave = atrial depolarization a. Upright in leads I, II, III, aVL, and aVF; inverted in lead aVR b. Measures <0.10 seconds wide and <3 mm high c. Normal PR interval is 0.12–0.20 seconds. 2. QRS complex = ventricular depolarization a. Measures 0.06-0.10 seconds wide b. Q wave (1) <0.04 seconds wide and <3 mm deep (2) Abnormal if it is >3 mm deep or >1/3 of the QRS complex. c. R wave ≤7.5 mm high 3. QT interval varies with rate and sex but is usually 0.33–0.42 seconds; at normal heart rates, it is normally <1/2 the preceding RR interval. 4. T wave = ventricular repolarization a. Upright in leads I, II, V3–V6; inverted in aVR b. Slightly rounded and asymmetric in configuration c. Measures ≤5 mm high in limb leads and ≤10 mm high in the chest leads 5. U wave = a ventricular afterpotential a. Any deflection after the T wave (usually low voltage) b. Same polarity as the T wave c. Most easily detected in lead V3 d. Can be a normal component of the ECG e. Prominent U waves may indicate one of the following: (1) Hypokalemia (<3 mEq/L) (2) Hypercalcemia (3) Therapy with digitalis, phenothiazines, quinidine, epinephrine, inotropic agents, or amiodarone (4) Thyrotoxicosis f.