Vermont Primary Care Sourcebook Bi-State Primary Care Association January 2016 5Th Edition
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Legislative Advisory Committee on the State House Draft Report
Legislative Advisory Committee on the State House Draft Report Report to the Vermont General Assembly Pursuant to 2021 Acts and Resolves No. 50, Section 32 Prepared by the Office of Legislative Counsel August 17, 2021 VT LEG #357238 v.4 2 Table of Contents A. Introduction ............................................................................................................................3 B. Statutory Charge of the Legislative Advisory Committee on the State House .......................4 C. Functions of the Legislative Advisory Committee on the State House ..................................5 D. Members of the Legislative Advisory Committee on the State House ...................................6 E. Summary of Advisory Committee Proceedings ......................................................................7 F. Advisory Committee Recommendations ................................................................................9 G. Conclusion ...........................................................................................................................16 VT LEG #357238 v.4 3 A. Introduction The Legislative Advisory Committee on the State House has met weekly for almost two months and members have had robust and productive discussions about how best to return to the State House in January. We have benefited greatly from the support from legislative staff who work in the State House and from staff at BGS. Our task was to make recommendations how to return to work in the State House, recognizing that the State House is the proper place for us to conduct legislative business, while also a workplace and a living museum. In these extraordinary times, these different roles may conflict, and we have done our best to make recommendations to resolve these conflicts or to identify issues that should be resolved in other venues or at a later time. We haven’t agreed on everything and our report reflects that. However, we are all in agreement that meeting in the State House next January will require flexibility and a willingness to adapt. -

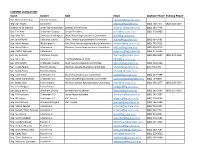
Federally-Qualified Health Centers in Districts of House Health Care Members
House Committee on Health Care Rep. William J. Lippert (D) Chittenden-4-2, Chair Rep. Douglas Gage (R) Rutland-5-4 Community Health Centers of Burlington Community Health Centers of the Rutland Region Alison Calderara, Interim CEO Grant Whitmer, Executive Director 617 Riverside Avenue 71 Allen Pond Street, Suite 101 Burlington, VT 05401 Rutland, VT 05701 [email protected]; (802) 264-8190 [email protected]; (802) 855-2083 Rep. Anne B. Donahue (R) Washington-1, Vice-Chair Rep. Michael Hebert (R) Windham-1 The Health Center Springfield Medical Care Systems John Matthew, MD, CEO Timothy Ford, CEO 157 Towne Avenue, PO Box 320 25 Ridgewood Road Plainfield, VT 05667 Springfield, VT 05156 [email protected]; (802) 454-8336 [email protected]; (802) 885-2151 Rep. Timothy Briglin (D) Windsor-Orange-2, Ranking Rep. Lori Houghton (D) Chittenden-8-2 Member Community Health Centers of Burlington Gifford Health Care Inc. Alison Calderara, Interim CEO Daniel Bennett, CEO 617 Riverside Avenue 44 South Main Street, PO Box 2000 Burlington, VT 05401 Randolph, VT 05060 [email protected]; (802) 264-8190 [email protected]; (802) 728-2304 Rep. Ben Jickling (I) Orange-Washington-Addison Rep. Annmarie Christensen (D) Windsor-2 Gifford Health Care Inc. Springfield Medical Care Systems Daniel Bennett, CEO Timothy Ford, CEO 44 South Main Street, PO Box 2000 25 Ridgewood Road Randolph, VT 05060 Springfield, VT 05156 [email protected]; (802) 728-2304 [email protected]; (802) 885-2151 Rep. Brian Cina (P) Chittenden-6-4 Community Health Centers of Burlington Alison Calderara, Interim CEO 617 Riverside Avenue Burlington, VT 05401 [email protected]; (802) 264-8190 Rep. -

Transmittal Email to House and Senate Members
Sent: Monday, March 5, 2018 1:47 PM To: David Ainsworth; Robert Bancroft; John Bartholomew; Fred Baser; Lynn Batchelor; Scott Beck; Paul Belaski; Steve Beyor; Clem Bissonnette; Thomas Bock; Bill Botzow; Patrick Brennan; Tim Briglin; Cynthia Browning; Jessica Brumsted; Susan Buckholz; Tom Burditt; Mollie Burke; William Canfield; Stephen Carr; Robin Chesnut-Tangerman; Annmarie Christensen; Kevin Christie; Brian Cina; Selene Colburn; Jim Condon; Peter Conlon; Daniel Connor; Chip Conquest; Sarah CopelandHanzas; Timothy Corcoran; Larry Cupoli; Maureen Dakin; David Deen; Dennis Devereux; Eileen Dickinson; Anne Donahue; Johannah Donovan; Betsy Dunn; Alyson Eastman; Alice Emmons; Peter Fagan; Rachael Fields; Robert Forguites; Robert Frenier; Douglas Gage; Marianna Gamache; John Gannon; Marcia Gardner; Dylan Giambatista; Diana Gonzalez; Maxine Grad; Rodney Graham; Adam Greshin; Sandy Haas; James Harrison; Mike Hebert; Robert Helm; Mark Higley; Matthew Hill; Mary Hooper; Jay Hooper; Lori Houghton; Mary Howard; Ronald Hubert; Kimberly Jessup; Ben Jickling; Mitzi Johnson; Ben Joseph; Bernie Juskiewicz; Brian Keefe; Kathleen Keenan; Charlie Kimbell; Warren Kitzmiller; Jill Krowinski; Rob LaClair; Martin LaLonde; Diane Lanpher; Richard Lawrence; Paul Lefebvre; Patti Lewis; William Lippert; Emily Long; Gabrielle Lucke; Terence Macaig; Michael Marcotte; Marcia Martel; Jim Masland; Christopher Mattos; Curt McCormack; Patricia McCoy; Francis McFaun; Alice Miller; Kiah Morris; Mary Morrissey; Mike Mrowicki; Barbara Murphy; Linda Myers; Gary Nolan; Terry -

Senate Standing Committees 2017 Govt
Senate Standing Committees 2017 Govt. Operations Sen. Jeanette White, Chair Agriculture Sen. Brian Collamore, V-Chair Sen. Bobby Starr, Chair Sen. Claire Ayer Sen. Anthony Pollina, V-Chair Sen. Alison Clarkson Sen. Brian Collamore Sen. Chris Pearson Sen. Carolyn Branagan Sen. Francis Brooks Health and Welfare Sen. Claire Ayer, Chair Appropriations Sen. Virginia Lyons, V-Chair Sen. Jane Kitchel, Chair Sen. Anne Cummings Sen. Alice Nitka, V-Chair Sen. Dick McCormack Sen. Richard Sears Sen. Debra Ingram Sen. Bobby Starr Sen. Dick McCormack Institutions Sen. Tim Ashe Sen. Peg Flory, Chair Sen. Richie Westman Sen. John Rogers, V-Chair Sen. Dick Mazza Econ Dev, Housing, and General Affairs Sen. Carolyn Branagan Sen. Kevin Mullin, Chair Sen. Francis Brooks Sen. Michael Sirotkin, V-Chair Sen. Philip Baruth Judiciary Sen. Becca Balint Sen. Dick Sears, Chair Sen. Alison Clarkson Sen. Joe Benning, V-Chair Sen. Jeanette White Education Sen. Alice Nitka Sen. Philip Baruth, Chair Sen. Tim Ashe Sen. Becca Balint, V-Chair Sen. Kevin Mullin Natural Resources Sen. Joe Benning Sen. Chris Bray, Chair Sen. Chris Bray Sen. Brian Campion, V-Chair Sen. Debra Ingram Sen. Mark MacDonald Sen. John Rogers Finance Sen. Chris Pearson Sen. Anne Cummings, Chair Sen. Mark MacDonald, V-Chair Transportation Sen. Virginia Lyons Sen. Dick Mazza, Chair Sen. Anthony Pollina Sen. Richie Westman, V-Chair Sen. Michael Sirotkin Sen. Jane Kitchel Sen. Brian Campion Sen. Peg Flory Sen. Dustin Degree Sen. Dustin Degree . -

Citizen Initiatives Teacher Training Gas Taxes
DEFENDING AGAINST SECURITY BREACHES PAGE 5 March 2015 Citizen Initiatives Teacher Training Gas Taxes AmericA’s innovAtors believe in nuclear energy’s future. DR. LESLIE DEWAN technology innovAtor Forbes 30 under 30 I’m developing innovative technology that takes used nuclear fuel and generates electricity to power our future and protect the environment. America’s innovators are discovering advanced nuclear energy supplies nearly one-fifth nuclear energy technologies to smartly and of our electricity. in a recent poll, 85% of safely meet our growing electricity needs Americans believe nuclear energy should play while preventing greenhouse gases. the same or greater future role. bill gates and Jose reyes are also advancing nuclear energy options that are scalable and incorporate new safety approaches. these designs will power future generations and solve global challenges, such as water desalination. Get the facts at nei.org/future #futureofenergy CLIENT: NEI (Nuclear Energy Institute) PUB: State Legislatures Magazine RUN DATE: February SIZE: 7.5” x 9.875” Full Page VER.: Future/Leslie - Full Page Ad 4CP: Executive Director MARCH 2015 VOL. 41 NO. 3 | CONTENTS William T. Pound Director of Communications Karen Hansen Editor Julie Lays STATE LEGISLATURES Contributing Editors Jane Carroll Andrade Mary Winter NCSL’s national magazine of policy and politics Web Editors Edward P. Smith Mark Wolf Copy Editor Leann Stelzer Advertising Sales FEATURES DEPARTMENTS Manager LeAnn Hoff (303) 364-7700 Contributors 14 A LACK OF INITIATIVE 4 SHORT TAKES ON -
Refer to This List for Area Legislators and Candidates
CURRENT LEGISLATORS Name District Role Email Daytime Phone Evening Phone Sen. Richard Westman Lamoille County [email protected] Rep. Dan Noyes Lamoille-2 [email protected] (802) 730-7171 (802) 644-2297 Speaker Mitzi Johnson Grand Isle-Chittenden Speaker of the House [email protected] (802) 363-4448 Sen. Tim Ashe Chittenden County Senate President [email protected] (802) 318-0903 Rep. Kitty Toll Caledona-Washington Chair, House Appropriations Committee [email protected] Sen. Jane Kitchel Caledonia County Chair, Senate Appropriations Committee [email protected] (802) 684-3482 Rep. Mary Hooper Washington-4 Vice Chair, House Appropriations Committee [email protected] (802) 793-9512 Rep. Marty Feltus Caledonia-4 Member, House Appropriations Committee [email protected] (802) 626-9516 Rep. Patrick Seymour Caledonia-4 [email protected] (802) 274-5000 Sen. Joe Benning Caledonia County [email protected] (802) 626-3600 (802) 274-1346 Rep. Matt Hill Lamoille 2 *NOT RUNNING IN 2020 [email protected] Sen. Phil Baruth Chittenden County Chair, Senate Education Committee [email protected] (802) 503-5266 Sen. Corey Parent Franklin County Member, Senate Education Committee [email protected] 802-370-0494 Sen. Randy Brock Franklin County [email protected] Rep. Kate Webb Chittenden 5-1 Chair, House Education Committee [email protected] (802) 233-7798 Rep. Dylan Giambatista Chittenden 8-2 House Leadership/Education Committee [email protected] (802) 734-8841 Sen. Bobby Starr Essex-Orleans Member, Senate Appropriations Committee [email protected] (802) 988-2877 (802) 309-3354 Sen. -
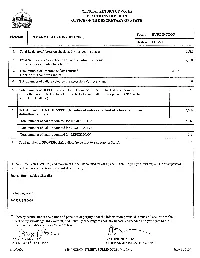
State Primary
OFFICIAL RETURN OF VOTES ELECTIONS DIVISION OFFICE OF THE SECRETARY OF STATE Town BURLINGTON Election PRIMARY ELECTION (08/11/2020) District CHI-6-1 1. Total Registered Voters on checklist for this polling place: 6,582 2. Total Number of Voters checked off on the entrance checklist: 2,790 (this includes absentee ballots) 3. Total number of absentee ballots returned: 2,016 (Include this count in Line 2) 4. Total number of ballots voted by the Accessible Voting System: 0 5. Total number of DEFECTIVE ballots (not counted but name checked off checklist): 133 (Enter the Total Defective ballots from the Defective Ballot Envelope. -- DO NOT include REPLACED ballots.) 6. TOTAL BALLOTS COUNTED: (Number of voters checked off checklist minus 2,666 defective ballots.) I Total number of ballots counted for DEMOCRATIC 2,042 I I Total number of ballots counted for PROGRESSIVE 13 I Total number of ballots counted for REPUBLICAN 611 I 7. Total number of PROVISIONAL ballots (to be sent to Secretary of State): 0 If line 6 (Total Votes Counted.) and the sum of the ballots counted for each party DO NOT agree, you must explain the discrepancies below and continue - Line 6 will be adjusted accordingly: .Human Error marking Checklist . ! Ballot bag seal#: 266931, 1296636 0 I hereby certify, under the pains and penalties of perjury, that the information provided is true and accurate to the best of my knowledge, information, and belief.By checking this box, no signature is needed and you agree to the terms and conditions under Vermont law. lr?J-v L:1i!!t~ KATHERINE SCHAD ~:T~ I1YCLERK CHIEF ADMINISTRATIVE OFFICER 11/10/2020 149 CHURCH STREET, BURLINGTON, VT, 05401 Page 1of109 Town BURLINGTON Election PRIMARY ELECTION District CHI-6-1 RALPH "CARCAJOU" CORBO DEMOCRATIC WALLINGFORD 90 I PETER WELCH DEMOCRATIC NORWICH 1,880 I TOTAL WRITE IN COUNTS DEMOCRATIC Si CHRIS BRIMMER (Write-in) DEMOCRATIC 3 ---· -- GREG DUSABLON (Write-in) DEMOCRATIC j TIM ASHE (Write-in) DEMOCRATIC OTHER WRITE IN COUNTS 0 OVERVOTES I~PH "CARCAJOU" CORBO DEMOCRATIC REBECCA HOLCOMBE DEMOCRATIC . -

YANKEE POST ANTHONY ROY, President March, 2021 TIM WEINLAND DAN COUGHLIN, Co-Editors
CONNECTICUT COUNCIL FOR THE SOCIAL STUDIES YANKEE POST ANTHONY ROY, President March, 2021 TIM WEINLAND DAN COUGHLIN, Co-editors President’s Message Editors’ Note Last summer, the Connecticut January 6 - what a start to 2021 ! This issue has several Council for the Social Studies articles devoted to the issues raised by politicians committed to look inward to and educators responding to the events of that day. evaluate our organization through Significant in that discussion is a letter sent to the an antiracist lens. The board of Connecticut legislature by President Tony Roy ( see directors said they would look Page 4) Adding to the discussion, on page 5 we raise at our programs, processes, and concerns we have voiced before: in what ways and to board composition to ensure that what degree are Social Studies classrooms to be held we are upholding a high standard responsible for promoting thoughtful, responsible of equity. This commitment is citizenship. At least one of us it old enough to remember long term and will be mostly when Social Studies was actually called Citizenship conducted behind the scenes, especially within the Education – at the time, it seemed that such a department early stages. Our course of action so far has been to seek title seemed one step shy of indoctrination. And a few help from an outside organization to guide us through of us can recall when the “Social” in Social Studies was strategic planning. Just last month, we signed a contract considered by the radical right as code for socialism . with the Nonprofit Center at LaSalle University and, by Whatever the history of department titles, it seems that the end of this academic year, the board will engage in we are called once again to help “cure” the nation’s ills. -

HOUSE COMMITTEES 2019 - 2020 Legislative Session
HOUSE COMMITTEES 2019 - 2020 Legislative Session Agriculture & Forestry Education Health Care Rep. Carolyn W. Partridge, Chair Rep. Kathryn Webb, Chair Rep. William J. Lippert Jr., Chair Rep. Rodney Graham, Vice Chair Rep. Lawrence Cupoli, Vice Chair Rep. Anne B. Donahue, Vice Chair Rep. John L. Bartholomew, Ranking Mbr Rep. Peter Conlon, Ranking Member Rep. Lori Houghton, Ranking Member Rep. Thomas Bock Rep. Sarita Austin Rep. Annmarie Christensen Rep. Charen Fegard Rep. Lynn Batchelor Rep. Brian Cina Rep. Terry Norris Rep. Caleb Elder Rep. Mari Cordes Rep. John O'Brien Rep. Dylan Giambatista Rep. David Durfee Rep. Vicki Strong Rep. Kathleen James Rep. Benjamin Jickling Rep. Philip Jay Hooper Rep. Woodman Page Appropriations Rep. Christopher Mattos Rep. Lucy Rogers Rep. Catherine Toll, Chair Rep. Casey Toof Rep. Brian Smith Rep. Mary S. Hooper, Vice Chair Rep. Peter J. Fagan, Ranking Member Energy & Technology Human Services Rep. Charles Conquest Rep. Timothy Briglin, Chair Rep. Ann Pugh, Chair Rep. Martha Feltus Rep. Laura Sibilia, Vice Chair Rep. Sandy Haas, Vice Chair Rep. Robert Helm Rep. Robin Chesnut-Tangerman, Rep. Francis McFaun, Ranking Member Rep. Diane Lanpher Ranking Member Rep. Jessica Brumsted Rep. Linda K. Myers Rep. R. Scott Campbell Rep. James Gregoire Rep. Maida Townsend Rep. Seth Chase Rep. Logan Nicoll Rep. Matthew Trieber Rep. Mark Higley Rep. Daniel Noyes Rep. David Yacovone Rep. Avram Patt Rep. Kelly Pajala Rep. Heidi E. Scheuermann Rep. Marybeth Redmond Commerce & Rep. Michael Yantachka Rep. Carl Rosenquist Rep. Theresa Wood Economic Development General, Housing, & Military Affairs Rep. Michael Marcotte, Chair Judiciary Rep. Thomas Stevens, Chair Rep. Jean O'Sullivan, Vice Chair Rep. -

Vermont Environmental Scorecard 2013-2014 Legislative Biennium Vermont Environmental Scorecard
Vermont Environmental Scorecard 2013-2014 Legislative Biennium Vermont Environmental Scorecard Dear Vermonter, We have prepared this Scorecard to let you know how your state legislators voted on environmental issues in 2013-2014. The legislative process can be complicated, and our objective is to distill the results so you, as a voter, can see which lawmakers are representing your interests – and which are not. The legislature made some notable progress on environmental priorities Vermont Conservation Voters this session. Positive steps included new protections for our shorelands, (VCV) is the non-partisan reducing children’s exposure to toxic chemicals, and helping more political action arm of Vermont’s Vermonters to go solar. However, significant work remains to be done on key priorities – including the need to take bolder action on climate change and environmental community. cleaning up Lake Champlain. Since 1982, our mission has been to defend and strengthen the laws that The votes included in this Scorecard represent a range of priorities of the environmental community, and were selected after consulting with partner safeguard our environment. We work organizations, including the Vermont Natural Resources Council, Vermont to elect environmentally responsible Public Interest Research Group, Conservation Law Foundation, Vermont candidates. We then hold legislators Chapter of the Sierra Club, and others. The particular votes included were accountable for the decisions based on whether the vote was substantive or procedural, and which vote had the greatest effect on the outcome of the legislation. they make affecting our air, water, communities, land, and wildlife. The scorecard does have limitations. For example, we can only score “roll call” votes where individual lawmakers vote yes or no on a given bill. -

Meet Dean Corren Anti-Union 'Think Tank' Wrong About Vermont
Meet Dean Corren Dean Corren talks to board of directors recently. When your board of directors voted single payer health care.” ourselves,” he said in a recent interview to recommend Dean Corren for at Vermont-NEA headquarters. “If Corren, a Progressive who also has the lieutenant governor, the decision we are going to have a functioning backing of Democrats, wants to be a was easy. democracy, we need to restore the lieutenant governor who “will work to meaning of politics.” “He really gets it,” President Martha restore the meaning of politics.” By that, Allen said. “Dean is an unabashed he wants to transform “politics” from This is not Corren’s first stab at elected union supporter. He is a believer in angry, partisan wrangling to a platform office. He served four terms in the the importance of public education. where people of differing views House from 1993-2000; he also was And he, alone among all of the exchange ideas, debate, and agree on an aide to then-Congressman Bernie statewide candidates out there, is a course of action that serves only one Sanders. For more than a decade, dedicated to ensuring our members purpose: to better the lives of everyone. he’s been the chief technology officer are treated fairly in the transition to “Politics, at its core, is how we govern continued on p. 7 Vol. 81 No. 2 • Oct., 2013 www.vtnea.orgThe Official Publication of the Vermont-National EducationAssociation Anti-Union ‘Think Tank’ Wrong About Vermont Vermont-NEA Vermont-NEA Editor’s Note: Vermont-NEA President course let alone reality. -

S.50 Memorandum to Agencies
115 STATE STREET REP. WILLIAM J. LIPPERT, CHAIR MONTPELIER, VT 05633 REP. ANNE B. DONAHUE, VICE CHAIR TEL: (802) 828-2228 REP. TIMOTHY BRIGLIN, RANKING MEMBER FAX: (802) 828-2424 REP. LORI HOUGHTON, CLERK REP. ANNMARIE CHRISTENSEN REP. BRIAN CINA REP. SARAH COPELAND-HANZAS REP. ELIZABETH "BETSY" DUNN REP. DOUGLAS GAGE STATE OF VERMONT REP. MICHAEL HEBERT GENERAL ASSEMBLY REP. BENJAMIN JICKLING HOUSE COMMITTEE ON HEALTH CARE MEMORANDUM To: Susan Gretkowski, Senior Government Affairs Strategist, MVP Healthcare Cory Gustafson, Commissioner, Department of Vermont Health Access Samantha Nelson, Government Affairs Consultant, BCBSVT Jill Olson, Executive Director, VNAs of Vermont From: Representative Bill Lippej CJu House Committee on Health Care Date: May 3, 2017 Subject: Home health provider-facilitated telemedicine The House Committee on Health Care has focused recent efforts on increasing access to health care services by expanding health insurance coverage for telemedicine to include services delivered to Vermonters in their homes. In the course of the Committee's deliberations on S.50, An act relating to insurance coverage for telemedicine services delivered in or outside a health care facility, the VNAs of Vermont identified home health providers as having the potential to play an important role in assisting their clients in using telemedicine at home. The Committee therefore respectfully requests that the VNAs of Vermont, in consultation with and with cooperation from the Department of Vermont Health Access, the Blueprint for Health, MVP Healthcare, BlueCross and Blue Shield of Vermont, and other interested public and private stakeholders, review existing literature and consider whether and under what circumstances home health providers should be reimbursed by Medicaid and commercial health insurance plans for facilitating and supporting the use of telemedicine in their clients' homes.