Palliative Care Program Data in Nova Scotia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

PC Candidate
Political Contributions Regime Annual Report, January 1, 2016 to December 31, 2016 Disclosure Statement of Registered Canddiates: The Progressive Conservative Association of Nova Scotia 01 Annapolis No registered candidate 02 Antigonish Candidate: Ray Mattie Official Agent: Rachel MacDonald Date Filed: march 29 2017 Contributions: NIL Last Name of Individual First Name Community Amount ($) Total of all contributions $200 or less Total NIL 03 Argyle-Barrington No registered candidate 04 Bedford Candidate: Valerie White Official Agent: Sandy Stevens Date Filed: March 16 2017 Contributions: NIL Last Name of Individual First Name Community Amount ($) Total of all contributions $200 or less Total NIL 05 Cape Breton Centre No registered candidate 06 Cape Breton-Richmond No registered candidate 07 Chester-St. Margaret’s No registered candidate 08 Clare-Digby No registered candidate 09 Clayton Park West Candidate: Paul Kimball Official Agent: Len MacKeigan Date Filed: March 16 2017 Contributions: NIL Last Name of Individual First Name Community Amount ($) Total of all contributions $200 or less Total NIL 10 Colchester-Musquodoboit Valley Candidate: William Harrison Official Agent: Penny Gilbert Date Filed: March 24 2017 Contributions: NIL Last Name of Individual First Name Community Amount ($) Total of all contributions $200 or less Total NIL 11 Colchester North No registered candidate Disclosure Statement of Registered Candidates: The Progressive Conservative Association of Nova Scotia, Continued 12 Cole Harbour-Eastern Passage Candidate: Barbara -

Accession 1985-110 Roads and Bridges Photographs. – 1908-1958. – 12,648 P
Roads and Bridges photographs. – 1908-1958. – 12,648 photographs & other material. (forms part of Department of Highways & Public Works fonds) (ACC 1985-110) File Items County Title Date Range Prints corresp. with Negs (x) Prints Nitrate Negatives (Box/Env) Acetate Negatives Plate Glass Negatives Textual Records Scanned Image Nos. Items Total 0001 001-015 Annapolis Allan Creek Bridge, near Annapolis Town Line 1920-1922 vol 001 75/289 201000001- 30 X 201000015 0001 016-021 Annapolis Allan Creek Bridge, near Annapolis Town Line 1920-1922 vol 001 6 0001 022-023 Annapolis Allan Creek Bridge, near Annapolis Town Line 1920-1922 75/289 201000016- 2 201000017 0002 001-002 Annapolis Anderson Bridge, 2.5 miles from Parkers Cove on undated vol 001 75/290 2 X road to Litchfield 0002 003-006 Annapolis Anderson Bridge, 2.5 miles from Parkers Cove on undated vol 001 4 road to Litchfield 0003 001-044 Annapolis Annapolis Bridge 1920-1923 vol 001 75/289 201000018- 88 X 201000061 0003 045-066 Annapolis Annapolis Bridge 1920-1923 vol 003 21 0003 068-071 Annapolis Annapolis Bridge 1920-1923 75/289 201000062- 4 201000065 0003 072-074 Annapolis Annapolis Bridge 1923 vol 003 3 0004 001 Annapolis Baker Bridge 1914 vol 001 75/291 201000066 2 X 0005 001 Annapolis Bath Bridge, four miles from Bridgetown on road undated vol 001 75/290 2 X to Annapolis 0006 001-002 Annapolis Bishop Brook Bridge, Round Hill 1929 vol 001 75/291 201000067- 3 X 201000068 0006 003 Annapolis Bishop Brook Bridge, Round Hill undated vol 001 1 0006 004 Annapolis Bishop Brook Bridge, Round Hill undated 75/291 201000069 1 0007 001 Annapolis Bishop (Wm) Bridge, Paradise undated 75/291 1 201000070 https://memoryns.ca/roads-and-bridges-photographs Accession 1985-110 Nova Scotia Archives. -

October 8, 2013 Nova Scotia Provincial General
47.1° N 59.2° W Cape Dauphin Point Aconi Sackville-Beaver Bank Middle Sackville Windsor μ Alder Junction Point Sackville-Cobequid Waverley Bay St. Lawrence Lower Meat Cove Capstick Sackville Florence Bras d'Or Waverley- North Preston New Waterford Hammonds Plains- Fall River- Lake Echo Aspy Bay Sydney Mines Dingwall Lucasville Beaver Bank Lingan Cape North Dartmouth White Point South Harbour Bedford East Cape Breton Centre Red River Big Intervale Hammonds Plains Cape North Preston-Dartmouth Pleasant Bay Bedford North Neils Harbour Sydney Preston Gardiner Mines Glace Bay Dartmouth North South Bar Glace Bay Burnside Donkin Ingonish Minesville Reserve Mines Ingonish Beach Petit Étang Ingonish Chéticamp Ferry Upper Marconi Lawrencetown La Pointe Northside- Towers Belle-Marche Clayton Cole Point Cross Victoria-The Lakes Westmount Whitney Pier Park Dartmouth Harbour- Halifax Sydney- Grand Lake Road Grand Étang Wreck Cove St. Joseph Leitches Creek du Moine West Portland Valley Eastern Shore Whitney Timberlea Needham Westmount French River Fairview- Port Morien Cap Le Moine Dartmouth Pier Cole Balls Creek Birch Grove Clayton Harbour Breton Cove South Sydney Belle Côte Kingross Park Halifax ^ Halifax Margaree Harbour North Shore Portree Chebucto Margaree Chimney Corner Beechville Halifax Citadel- Indian Brook Margaree Valley Tarbotvale Margaree Centre See CBRM Inset Halifax Armdale Cole Harbour-Eastern Passage St. Rose River Bennet Cape Dauphin Sable Island Point Aconi Cow Bay Sydney River Mira Road Sydney River-Mira-Louisbourg Margaree Forks Egypt Road North River BridgeJersey Cove Homeville Alder Point North East Margaree Dunvegan Englishtown Big Bras d'Or Florence Quarry St. Anns Eastern Passage South West Margaree Broad Cove Sydney New Waterford Bras d'Or Chapel MacLeods Point Mines Lingan Timberlea-Prospect Gold Brook St. -

Constitution of the Progressive Conservative Association of Nova Scotia
CONSTITUTION OF THE PROGRESSIVE CONSERVATIVE ASSOCIATION OF NOVA SCOTIA Consolidated to November 1, 2008 Amended on November 26, 2011 Amended on February 11, 2012 Amended on February 8, 2014 Amended on November 2, 2019 ARTICLE 1 - NAME 1.1 The name of the Association is “The Progressive Conservative Association of Nova Scotia”, hereinafter called “the Association”. ARTICLE 2 - INTERPRETATION 2.1 Provincial Electoral District, Constituency or Riding, means an electoral district as defined in the Elections Act, and the boundaries of such shall conform with the electoral districts entitled to elect members to serve in the House of Assembly. 2.2 Member of the House of Assembly means a member of the Nova Scotia House of Assembly as defined in the Elections Act. 2.3 Constituency Association means a group of individuals within one electoral district who are members of the Association, who have joined to promote the interests of the Progressive Conservative Party and the Progressive Conservative Association of Nova Scotia, and which has been duly recognized by the Association in accordance with this Constitution. 2.4 Party means the Progressive Conservative Party of Nova Scotia. 2.5 Standing Committee means any committee designated in this Constitution as a Standing Committee, or which the Association or Executive Committee may annually designate by resolution. 2.6 Recognized Group means an organized group of members of the Association, other than a constituency association, which has been recognized in accordance with this Constitution. 2.7 In the event of an inconsistency between this Constitution and any by-law, constituency association constitution or rule, or other decision made under this Constitution, the provisions of this Constitution shall prevail. -

PAGE 2 SOUTH CUMBERLAND NEWS - AUGUST, 2021 Mayor Scott Provided This Comment When Completing the Election Questionnaire on the Needs of Cumberland County
PAGE 2 SOUTH CUMBERLAND NEWS - AUGUST, 2021 Mayor Scott provided this comment when completing the Election Questionnaire on the needs of Cumberland County. The Shoreline Journal and South Cumberland News sent questionnaires to Mayors in Colchester and Cumberland Counties and to identifiable candidates in Truro Bible Hill Salmon River Millbrook; Colchester North and Cumberland South. Only Mayor Scott and Larry Duchesne, NDP Candidate in Cumberland South responded. Mayor Scott’s completed questionnaire is presented below: 1. Considering the needs of Municipality of Cumberland, what is the most important election promise made, to date, and must be fulfilled Mayor Murray Scott delivered by government formed following August 17th election? Several issues face our municipality and citizens. From what I hear regularly from residents, one issue is healthcare concerns regarding doctors and emergency health services. As always, we have issues on aging The dozens of geese at Newville Lake have a habit of crossing the road for better grass, and morning fog showed especially why the sign a infrastructure like roads and bridges, sewer and water that continue to be kind person has put up is even a better idea. The third photo shows several geese actually crossing the road. (Lawrence R Nicoll Photo) topics that concern voters in this area. 2. What item in the election platforms, indicated so far, which one is the least beneficial to businesses and residents of Municipality of Cumberland? All political parties do polling to determine the issues most important to people in specific ridings and across the province. I prefer to look at the positive side and I see where there are opportunities that all the parties have identified so far in health care, tolls, and infrastructure to move our province forward. -

Provincial Legislatures
PROVINCIAL LEGISLATURES ◆ PROVINCIAL & TERRITORIAL LEGISLATORS ◆ PROVINCIAL & TERRITORIAL MINISTRIES ◆ COMPLETE CONTACT NUMBERS & ADDRESSES Completely updated with latest cabinet changes! 86 / PROVINCIAL RIDINGS PROVINCIAL RIDINGS British Columbia Surrey-Green Timbers ............................Sue Hammell ......................................96 Surrey-Newton........................................Harry Bains.........................................94 Total number of seats ................79 Surrey-Panorama Ridge..........................Jagrup Brar..........................................95 Liberal..........................................46 Surrey-Tynehead.....................................Dave S. Hayer.....................................96 New Democratic Party ...............33 Surrey-Whalley.......................................Bruce Ralston......................................98 Abbotsford-Clayburn..............................John van Dongen ................................99 Surrey-White Rock .................................Gordon Hogg ......................................96 Abbotsford-Mount Lehman....................Michael de Jong..................................96 Vancouver-Burrard.................................Lorne Mayencourt ..............................98 Alberni-Qualicum...................................Scott Fraser .........................................96 Vancouver-Fairview ...............................Gregor Robertson................................98 Bulkley Valley-Stikine ...........................Dennis -

Electoral District of Cumberland South
Map 1 of 2 16 - Electoral District of Cumberland South K l o n d i k Tr e av R is d R Mansfield R M d i t Fage Rd p P l e le a s D Hastings East y i a c 1 k Mansfield Rd n son 5 Rd Leicester t d L R R o d e r o u p t s a John King Rd Minudie P Hastings Rd g Upper Mount i West 020 B d ack R Brookdale and B Nappan Pleasant ke Leicester 008 La Thornewaite Rd d 1 R 5 - C c um p M be be 019 o ol rla Bi Lo a K n r d p Kolbec d l N P Salem e 16 o o 022 r Highway 204 L - C r t Fenwick t e u h n m r b d e e R s rl a R a d d n R d S h o P u d C t . h Fe i 018 nwick d Little River e N R Lower Nappan Highway 104 R o i d l Roslin R Maccan e H ve s Stanley Oxford o Ripley Br an C R s r d f e d o r R d w n o Barronsfield a Sugar L n S L c e i c pl d a Lower T a i ri M n M d g r e Oxford e River r Rd R w C o d L Chignecto Inset r Lower Hebert Hansford o w d Black le R y R Cove d t R d s n River Road 024 d Little Forks H rk Salt Springs e Ha Harrison o m R nsford Rd H i el g F t i e H ghw 2 t 4 h ay 2 Lake n e e i l i w t g 8 Lower a t S H i 025 h 6 w L M River a d i i y 3 g a e Wentworth e 2 y h o Streets Ridge 017 y Hebert R J Big w Springhill a 3 a Lake w 0 y 7 East h 12 - Colchester North Junction South 15 - Cumberland North Oxford g n 3 i Maccan Highway 204 e i 0 Birchwood H t P t R 2 023 Victoria d 009 Junction x Mattatall Kelly Rd Glenville E OldH Highway 4 028 d Mattatall a nter R Lake Lake d li u d fa H R x R Maccan 021 R d t d d k R R n c Woods d o J Rd ch d a u le d l Fis R d m ng n e e R re i B h er 42 R r f 1 la 1 r F s 2 te s s y C 3 West -

EDA Registration Status
Status of Electoral Districts Associations This webpage contains the registration status of electoral district associations (EDA) for all registered political parties, as of January 14, 2021. EDAs that have not registered The table below (based on the electoral districts as defined in the 2019 House of Assembly Act) lists, by electoral district and by party, the EDA registration status. Party: • Atlantica: Atlantica Party Association of Nova Scotia (No registered EDAs) • Green: Green Party of Nova Scotia • Liberal: Nova Scotia Liberal Party • NDP: Nova Scotia New Democratic Party • PC: The Progressive Conservative Association of Nova Scotia Status: • “Registered” indicates that the appropriate financial report and EDA registration form has been filed (Form 4 or Form 4-1) and accepted. • Grey (blank) indicates that the appropriate EDA registration form has not been filed and accepted. • “Suspended” indicates that an EDA has not filed their financial reports for the previous calendar year. Electoral District Green Liberal NDP PC 1 Annapolis Registered Registered Registered 2 Antigonish Registered Registered Registered 3 Argyle Registered Registered Registered 4 Bedford Basin Registered Registered Registered 5 Bedford South Registered Registered Registered 6 Cape Breton-Whitney Pier Registered Registered 7 Cape Breton East Registered Registered 8 Chester-St. Margaret's Registered Registered Registered 9 Clare Registered Registered Registered 10 Clayton Park West Registered Registered Registered 11 Colchester-Musquodoboit Valley Registered -

Journals and Proceedings
MEMBERS OF THE LEGISLATIVE ASSEMBLY First Session of the Fifty-Ninth General Assembly Speaker: The Honourable Murray Scott Constituency Member Annapolis Stephen McNeil Antigonish Hon. Angus MacIsaac Argyle Hon. Chris d’Entremont Bedford Hon. Peter Christie Cape Breton Centre Frank Corbett Cape Breton North Hon. Cecil Clarke Cape Breton Nova Gordie Gosse Cape Breton South Manning MacDonald Cape Breton West Russell MacKinnon Chester-St. Margaret’s John Chataway Clare Wayne Gaudet Colchester-Musquodoboit Valley Brooke Taylor Colchester North Bill Langille Cole Harbour Darrell Dexter Cole Harbour-Eastern Passage Kevin Deveaux Cumberland North Hon. Ernie Fage Cumberland South Hon. Murray Scott Dartmouth East Joan Massey Dartmouth North Jerry Pye Dartmouth South-Portland Valley Marilyn More Digby-Annapolis Harold Theriault Eastern Shore Bill Dooks Glace Bay H. David Wilson Guysborough- Sheet Harbour Ron Chisholm Halifax Atlantic Michele Raymond Halifax Chebucto Howard Epstein Halifax Citadel Danny Graham Halifax Clayton Park Diana Whalen Halifax Fairview Graham Steele Halifax Needham Maureen MacDonald Hammonds Plains-Upper Sackville Hon. Barry Barnet Hants East John MacDonell Hants West Hon. Ronald Russell Inverness Hon. Rodney MacDonald Kings North Mark Parent Kings South Hon. David Morse Kings West Leo Glavine Lunenburg Hon. Michael Baker Lunenburg West Hon. Carolyn Bolivar-Getson Pictou Centre Hon. John Hamm Pictou East Jim DeWolfe Pictou West Charlie Parker Preston Keith Colwell Queens Hon. Kerry Morash Richmond Michel Samson Sackville-Cobequid David A. Wilson Shelburne Cecil O’Donnell Timberlea-Prospect Bill Estabrooks Truro-Bible Hill Hon. Jamie Muir Victoria-The Lakes Gerald Sampson Waverley-Fall River-Beaverbank Gary Hines Yarmouth Hon. Richard Hurlburt OFFICERS OF THE ASSEMBLY Roderick K. -
Riding by Riding-Breakdown
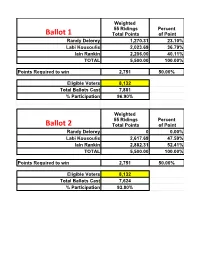
Weighted 55 Ridings Percent Total Points of Point Randy Delorey 1,270.31 23.10% Labi Kousoulis 2,023.69 36.79% Iain Rankin 2,206.00 40.11% TOTAL 5,500.00 100.00% Points Required to win 2,751 50.00% Eligible Voters 8,132 Total Ballots Cast 7,881 % Participation 96.90% Weighted 55 Ridings Percent Total Points of Point Randy Delorey 0 0.00% Labi Kousoulis 2,617.69 47.59% Iain Rankin 2,882.31 52.41% TOTAL 5,500.00 100.00% Points Required to win 2,751 50.00% Eligible Voters 8,132 Total Ballots Cast 7,624 % Participation 93.80% DISTRICT Candidate Final Votes Points 01 - ANNAPOLIS Randy DELOREY 31 26.5 01 - ANNAPOLIS Labi KOUSOULIS 34 29.06 01 - ANNAPOLIS Iain RANKIN 52 44.44 01 - ANNAPOLIS Total 117 100 Candidate Final Votes Points 02 - ANTIGONISH Randy DELOREY 176 53.01 02 - ANTIGONISH Labi KOUSOULIS 35 10.54 02 - ANTIGONISH Iain RANKIN 121 36.45 02 - ANTIGONISH Total 332 100 Candidate Final Votes Points 03 - ARGYLE Randy DELOREY 37 41.11 03 - ARGYLE Labi KOUSOULIS 24 26.67 03 - ARGYLE Iain RANKIN 29 32.22 03 - ARGYLE Total 90 100 Candidate Final Votes Points 04 - BEDFORD BASIN Randy DELOREY 92 34.72 04 - BEDFORD BASIN Labi KOUSOULIS 100 37.74 04 - BEDFORD BASIN Iain RANKIN 73 27.55 04 - BEDFORD BASIN Total 265 100 Candidate Final Votes Points 05 - BEDFORD SOUTH Randy DELOREY 116 39.59 05 - BEDFORD SOUTH Labi KOUSOULIS 108 36.86 05 - BEDFORD SOUTH Iain RANKIN 69 23.55 05 - BEDFORD SOUTH Total 293 100 Candidate Final Votes Points 06 - CAPE BRETON CENTRE - WHITNEY PIER Randy DELOREY 11 12.36 06 - CAPE BRETON CENTRE - WHITNEY PIER Labi KOUSOULIS 30 33.71 06 - CAPE BRETON CENTRE - WHITNEY PIER Iain RANKIN 48 53.93 06 - CAPE BRETON CENTRE - WHITNEY PIER Total 89 100 Candidate Final Votes Points 07 - CAPE BRETON EAST Randy DELOREY 22 19.47 07 - CAPE BRETON EAST Labi KOUSOULIS 32 28.32 07 - CAPE BRETON EAST Iain RANKIN 59 52.21 07 - CAPE BRETON EAST Total 113 100 Candidate Final Votes Points 08 - CHESTER - St. -

NS Royal Gazette Part I
Nova Scotia Published by Authority PART 1 VOLUME 216, NO. 3 HALIFAX, NOVA SCOTIA, WEDNESDAY, JANUARY 17, 2007 A certified copy of an Order in Council IN THE MATTER OF: The Companies Act, dated January 12, 2007 Chapter 81, R.S.N.S., 1989, as amended; - and - 2007-30 IN THE MATTER OF: An Application by 3077578 Nova Scotia Company for Leave to The Governor in Council is pleased to appoint, Surrender its Certificate of Amalgamation confirm and ratify the actions of the following Minister: To be Acting Minister of Service Nova Scotia and NOTICE IS HEREBY GIVEN that 3077578 Nova Municipal Relations, Acting Minister responsible for Scotia Company intends to make an application to the the Residential Tenancies Act, and to be responsible for Registrar of Joint Stock Companies for leave to surrender any and all other duties assigned to that Minister from its Certificate of Amalgamation. 10:45 p.m., Friday, January 12, 2007 until 2:30 p.m., Sunday, January 21, 2007: the Honourable Angus DATED this January 17, 2007. MacIsaac. Charles S. Reagh / Stewart McKelvey Certified to be a true copy Solicitor for 3077578 Nova Scotia Company sgd: Paul LaFleche Paul LaFleche 114 January 17-2007 Clerk of the Executive Council IN THE MATTER OF: The Companies Act IN THE MATTER OF: The Companies Act, (Nova Scotia) Chapter 81, R.S.N.S., 1989, as amended; - and - - and - IN THE MATTER OF: An Application by IN THE MATTER OF: An Application by 3097430 Nova Scotia Limited for Leave to 3058351 Nova Scotia Corp. for Leave to Surrender its Certificate of Incorporation Surrender its Certificate of Incorporation NOTICE IS HEREBY GIVEN that 3097430 Nova NOTICE IS HEREBY GIVEN that 3058351 Nova Scotia Limited intends to make an application to the Scotia Corp. -

Status of Electoral District Associations, June 24, 2021
Status of Electoral Districts Associations This webpage contains the registration status of electoral district associations (EDA) for all registered political parties, as of June 24, 2021. EDAs that have not registered The table below (based on the electoral districts as defined in the 2019 House of Assembly Act) lists, by electoral district and by party, the EDA registration status. Party: • Atlantica: Atlantica Party Association of Nova Scotia (No registered EDAs) • Green: Green Party of Nova Scotia • Liberal: Nova Scotia Liberal Party • NDP: Nova Scotia New Democratic Party • PC: The Progressive Conservative Association of Nova Scotia Status: • “Registered” indicates that the appropriate financial report and EDA registration form has been filed (Form 4 or Form 4-1) and accepted. • Grey (blank) indicates that the appropriate EDA registration form has not been filed and accepted. • “Suspended” indicates that an EDA has not filed their financial reports for the previous calendar year. Electoral District Green Liberal NDP PC 1 Annapolis Registered Registered Registered 2 Antigonish Registered Registered Registered 3 Argyle Registered Registered Registered 4 Bedford Basin Registered Registered Registered 5 Bedford South Registered Registered Registered 6 Cape Breton-Whitney Pier Registered Registered 7 Cape Breton East Registered Registered Registered 8 Chester-St. Margaret's Registered Registered Registered 9 Clare Registered Registered Registered 10 Clayton Park West Registered Registered Registered 11 Colchester-Musquodoboit Valley Registered