Respiratory System Respiratory System the Major Respiratory Organs
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Correlation Between Tidal Volume Measured by Spirometry and Impedance Pneumography
New Jersey Institute of Technology Digital Commons @ NJIT Theses Electronic Theses and Dissertations Fall 10-31-1994 Correlation between tidal volume measured by spirometry and impedance pneumography Krithika Seshadri New Jersey Institute of Technology Follow this and additional works at: https://digitalcommons.njit.edu/theses Part of the Biomedical Engineering and Bioengineering Commons Recommended Citation Seshadri, Krithika, "Correlation between tidal volume measured by spirometry and impedance pneumography" (1994). Theses. 1696. https://digitalcommons.njit.edu/theses/1696 This Thesis is brought to you for free and open access by the Electronic Theses and Dissertations at Digital Commons @ NJIT. It has been accepted for inclusion in Theses by an authorized administrator of Digital Commons @ NJIT. For more information, please contact [email protected]. Copyright Warning & Restrictions The copyright law of the United States (Title 17, United States Code) governs the making of photocopies or other reproductions of copyrighted material. Under certain conditions specified in the law, libraries and archives are authorized to furnish a photocopy or other reproduction. One of these specified conditions is that the photocopy or reproduction is not to be “used for any purpose other than private study, scholarship, or research.” If a, user makes a request for, or later uses, a photocopy or reproduction for purposes in excess of “fair use” that user may be liable for copyright infringement, This institution reserves the right to refuse to -

Chapter 22 We Won't Do Much Anatomy Here (Left Column; 22.1-22.3)
Chapter 22 Marieb & Hoehn (2019), p. 8181 We won’t do much anatomy here (left column; 22.1-22.3). Main issues (in lecture and lab): mechanics and measurement of breathing (22.4-22.5), chemoreceptor control of ventilation (22.8), and a few respiratory disorders (22.10). *** Sections 22.6-22.7 were briefly covered in Chapter 17. 1 Ch. 22: Test Question Templates • Q1. If given an appropriate graph of volume of air in lung vs. time, estimate or calculate FEV1/FVC ratio, FVC, residual volume, TLC, tidal volume, and/or minute ventilation. • Example (from Winter 2019 exam): 2 Q1. There are multiple ways to do this. The key is to choose a respiratory rate (breaths per minute) and a tidal volume (milliliters of air per breath) that, when multiplied together, give you 4000 mL air/minute. For example, I can draw a curve to show a tidal volume of 400 mL and a respiratory rate of 10 breaths/minute. Minute ventilation = (tidal volume)*(respiratory rate) = (400 mL air/breath)*(10 breaths/min) = 4000 mL air/min. 2 • Q2. If given two of the three values, calculate the third one: minute ventilation, respiratory rate, and tidal volume. • Example: Lola takes 10 breaths per minute, and her minute ventilation is 6000 mL air per minute. What is her tidal volume? • Q3. If given spirometry data and reference values, determine whether the data are consistent with obstructive pulmonary disease, restrictive pulmonary disease, both, or neither. • Example [from Fall 2019 test]: Rik is put through various pulmonary function tests. At time 0 in the table below, he begins deflating his fully inflated lungs as forcefully and rapidly as he can. -

Mechanisms of Pulmonary Gas Exchange Abnormalities During Experimental Group B Streptococcal Infusion
003 I -3998/85/1909-0922$02.00/0 PEDIATRIC RESEARCH Vol. 19, No. 9, I985 Copyright 0 1985 International Pediatric Research Foundation, Inc. Printed in (I.S. A. Mechanisms of Pulmonary Gas Exchange Abnormalities during Experimental Group B Streptococcal Infusion GREGORY K. SORENSEN, GREGORY J. REDDING, AND WILLIAM E. TRUOG ABSTRACT. Group B streptococcal sepsis in newborns obtained from GBS (5, 6). Arterial Poz fell by 9 torr in association produces pulmonary arterial hypertension and hypoxemia. with the increase in pulmonary arterial pressure (4). In contrast, The purpose of this study was to investigate the mecha- the neonatal piglet infused with GBS demonstrated both pul- nisms by which hypoxemia occurs. Ten anesthetized, ven- monary arterial hypertension and profound arterial hypoxemia tilated piglets were infused with 2 x lo9 colony forming (7). These results suggest that the neonatal pulmonary vascula- unitstkg of Group B streptococci over a 30-min period. ture may respond to bacteremia differently from that of adults. Pulmonary arterial pressure rose from 14 ? 2.8 to 38 ? The relationship between Ppa and the matching of alveolar 6.7 torr after 20 min of the bacterial infusion (p< 0.01). ventilation and pulmonary perfusion, a major determinant of During the same period, cardiac output fell from 295 to arterial oxygenation during room air breathing (8), has not been 184 ml/kg/min (p< 0.02). Arterial Po2 declined from 97 studied in newborns. The predictable rise in Ppa with an infusion 2 7 to 56 2 11 torr (p< 0.02) and mixed venous Po2 fell of group B streptococcus offers an opportunity to delineate the from 39.6 2 5 to 28 2 8 torr (p< 0.05). -

Oxygenation and Oxygen Therapy
Rules on Oxygen Therapy: Physiology: 1. PO2, SaO2, CaO2 are all related but different. 2. PaO2 is a sensitive and non-specific indicator of the lungs’ ability to exchange gases with the atmosphere. 3. FIO2 is the same at all altitudes 4. Normal PaO2 decreases with age 5. The body does not store oxygen Therapy & Diagnosis: 1. Supplemental O2 is an FIO2 > 21% and is a drug. 2. A reduced PaO2 is a non-specific finding. 3. A normal PaO2 and alveolar-arterial PO2 difference (A-a gradient) do NOT rule out pulmonary embolism. 4. High FIO2 doesn’t affect COPD hypoxic drive 5. A given liter flow rate of nasal O2 does not equal any specific FIO2. 6. Face masks cannot deliver 100% oxygen unless there is a tight seal. 7. No need to humidify if flow of 4 LPM or less Indications for Oxygen Therapy: 1. Hypoxemia 2. Increased work of breathing 3. Increased myocardial work 4. Pulmonary hypertension Delivery Devices: 1. Nasal Cannula a. 1 – 6 LPM b. FIO2 0.24 – 0.44 (approx 4% per liter flow) c. FIO2 decreases as Ve increases 2. Simple Mask a. 5 – 8 LPM b. FIO2 0.35 – 0.55 (approx 4% per liter flow) c. Minimum flow 5 LPM to flush CO2 from mask 3. Venturi Mask a. Variable LPM b. FIO2 0.24 – 0.50 c. Flow and corresponding FIO2 varies by manufacturer 4. Partial Rebreather a. 6 – 10 LPM b. FIO2 0.50 – 0.70 c. Flow must be sufficient to keep reservoir bag from deflating upon inspiration 5. -

Pressure-Controlled Ventilation in Children with Severe Status Asthmaticus*
Feature Articles Pressure-controlled ventilation in children with severe status asthmaticus* Ashok P. Sarnaik, MD, FAAP, FCCM; Kshama M. Daphtary, MD; Kathleen L. Meert, MD, FAAP; Mary W. Lieh-Lai, MD, FAAP; Sabrina M. Heidemann, MD, FAAP Objective: The optimum strategy for mechanical ventilation in trolled ventilation, median pH increased to 7.31 (6.98–7.45, p < a child with status asthmaticus is not established. Volume-con- .005), and PCO2 decreased to 41 torr (21–118 torr, p < .005). For trolled ventilation continues to be the traditional approach in such patients with respiratory acidosis (PCO2 >45 torr) within 1 hr of children. Pressure-controlled ventilation may be theoretically starting pressure-controlled ventilation, the median length of time more advantageous in allowing for more uniform ventilation. We until PCO2 decreased to <45 torr was 5 hrs (1–51 hrs). Oxygen describe our experience with pressure-controlled ventilation in saturation was maintained >95% in all patients. Two patients had children with severe respiratory failure from status asthmaticus. pneumomediastinum before pressure-controlled ventilation. One Design: Retrospective review. patient each developed pneumothorax and subcutaneous emphy- Setting: Pediatric intensive care unit in a university-affiliated sema after initiation of pressure-controlled ventilation. All pa- children’s hospital. tients survived without any neurologic morbidity. Median duration Patients: All patients who received mechanical ventilation for of mechanical ventilation was 29 hrs (4–107 hrs), intensive care status asthmaticus. stay was 56 hrs (17–183 hrs), and hospitalization was 5 days Interventions: Pressure-controlled ventilation was used as the (2–20 days). initial ventilatory strategy. The optimum pressure control, rate, Conclusions: Based on this retrospective study, we suggest and inspiratory and expiratory time were determined based on that pressure-controlled ventilation is an effective ventilatory blood gas values, flow waveform, and exhaled tidal volume. -

Respiratory Therapy Pocket Reference
Pulmonary Physiology Volume Control Pressure Control Pressure Support Respiratory Therapy “AC” Assist Control; AC-VC, ~CMV (controlled mandatory Measure of static lung compliance. If in AC-VC, perform a.k.a. a.k.a. AC-PC; Assist Control Pressure Control; ~CMV-PC a.k.a PS (~BiPAP). Spontaneous: Pressure-present inspiratory pause (when there is no flow, there is no effect ventilation = all modes with RR and fixed Ti) PPlateau of Resistance; Pplat@Palv); or set Pause Time ~0.5s; RR, Pinsp, PEEP, FiO2, Flow Trigger, rise time, I:E (set Pocket Reference RR, Vt, PEEP, FiO2, Flow Trigger, Flow pattern, I:E (either Settings Pinsp, PEEP, FiO2, Flow Trigger, Rise time Target: < 30, Optimal: ~ 25 Settings directly or by inspiratory time Ti) Settings directly or via peak flow, Ti settings) Decreasing Ramp (potentially more physiologic) PIP: Total inspiratory work by vent; Reflects resistance & - Decreasing Ramp (potentially more physiologic) Card design by Respiratory care providers from: Square wave/constant vs Decreasing Ramp (potentially Flow Determined by: 1) PS level, 2) R, Rise Time ( rise time ® PPeak inspiratory compliance; Normal ~20 cmH20 (@8cc/kg and adult ETT); - Peak Flow determined by 1) Pinsp level, 2) R, 3)Ti (shorter Flow more physiologic) ¯ peak flow and 3.) pt effort Resp failure 30-40 (low VT use); Concern if >40. Flow = more flow), 4) pressure rise time (¯ Rise Time ® Peak v 0.9 Flow), 5) pt effort ( effort ® peak flow) Pplat-PEEP: tidal stress (lung injury & mortality risk). Target Determined by set RR, Vt, & Flow Pattern (i.e. for any set I:E Determined by patient effort & flow termination (“Esens” – PDriving peak flow, Square (¯ Ti) & Ramp ( Ti); Normal Ti: 1-1.5s; see below “Breath Termination”) < 15 cmH2O. -

The Effects of Bronchodilators on Pulmonary Ventilation and Diffusion in Asthma and Emphysema
Thorax: first published as 10.1136/thx.14.2.146 on 1 June 1959. Downloaded from Thorax (1959), 14, 146. THE EFFECTS OF BRONCHODILATORS ON PULMONARY VENTILATION AND DIFFUSION IN ASTHMA AND EMPHYSEMA BY GERARD LORRIMAN From Brompton Hospital and the Institute of Diseases of the Chest, London (RECEIVED FOR PUBLICATION SEPTEMBER 22, 1958) Impairment of ventilation and of the distribution capacity. The proportionate responsibility of of inspired air in asthma and emphysema has these two factors is, however, unknown. Little has been reported by many authors (Beitzke, 1925; been published on the diffusing capacity in asthma. Kountz and Alexander, 1934; Darling, Cournand, Bates (1952) measured the percentage uptake of and Richards, 1944; Baldwin, Cournand, and carbon monoxide in 13 young asthmatics aged Richards, 1949; Bates and Christie, 1950; Beale, 12-19 years and found an abnormally low figure Fowler, and Comroe, 1952), and is the result in only one. Ogilvie and others (1957) mention mainly, if not entirely, of obstruction of the one asthmatic patient whose diffusing capacity was airway. Antispasmodics can relieve the obstruction normal. in asthma, and have also been recommended in The objects of the present investigation were to emphysema (Baldwin and others, 1949; Christie, examine the effects of two drugs, isoprenalinecopyright. 1952). Corticotrophin and cortisone - like given by inhalation and prednisone orally, on the substances have been used with benefit in acute ventilation and diffusing capacity in patients with and chronic asthma (Bordley, Carey, Harvey, asthma and emphysema, and to attempt to assess Howard, Kattus, Newman, and Winkenwerder, the degree to which airway obstruction can depress 1949; Friedlaender and Friedlaender, 1951; the diffusing capacity in these disorders. -
Department of Internal Medicine, Both to End This Pandemic and to Ensure That Racial Inequities Are Ameliorated, E
DEPARTMENTVitals OF INTERNAL MEDICINE internalmedicineiowa.org Vitals Table of Contents From the chair .....................................................................................................................3 RESEARCH ...........................................................................................................................4 UI nephrologists collaborate on new textbook ......................................................6 Gehlbach, Richerson to investigate carbon dioxide role in SUDEP ................7 Abel to lead one of four AHA research networks .................................................8 Model developed to calculate patient risk for NAFLD decompensation .....9 Clinical trials in cancer at Iowa barely lose a step ..............................................10 EDUCATION .....................................................................................................................12 Grand Rounds expands its reach ..............................................................................14 Residency committees spotlight ...............................................................................16 On the cover OSCE gets national exposure, refines and expands again ..............................18 Microscopic image of a mouse lung expressing human ACE2, the receptor PATIENT CARE ................................................................................................................20 for SARS-CoV2. The blue staining represents the normal mouse lung, UI Hospitals & Clinics provides -

Lung Volume Kit Be-Lungkit
LUNG VOLUME KIT BE-LUNGKIT Lung Volume is a broad term that actually refers to several different respiratory measurements: Tidal Volume - volume of air that is exhaled when breathing out normally. Expiratory Reserve - volume of air that that can still be exhaled after having breathed out normally. Inspiratory Reserve - additional volume of air that is available for strenuous activity. This is the volume of air that can still enter your lungs after taking a normal breath. Vital Capacity - total useable volume of air. Residual Volume - unusable volume of air. (Residual volume cannot be measured with this kit.) Assembly You can measure the lung volumes of an individual using this kit. To assemble it, please follow these instructions: 1. Insert the mouthpiece halfway through the opening of the volume bag. Secure the mouthpiece with the rubber bands. 2. While sitting, hold the bag on your knee and press a paper towel against it to force the air out of the bag. Start with the sealed end and push the air out toward the mouthpiece. Measure Tidal Volume 1. Wipe the mouthpiece with a cotton ball dipped in alcohol to clean it. 2. Take a normal breath in, hold your nose and take a normal breath out into the lung volume bag mouthpiece. Slide a paper towel along the bag to push all the air to the lower end and measure the volume of air it contains. (The bag has liter and 1/10 liter graduations.) Record this as tidal volume. 3. Remove all the air from the lung volume bag by sliding the paper towel along its length. -

Development of Ventilatory Response to Transient Hypercapnia and Hypercapnic Hypoxia in Term Infants
0031-3998/04/5502-0302 PEDIATRIC RESEARCH Vol. 55, No. 2, 2004 Copyright © 2004 International Pediatric Research Foundation, Inc. Printed in U.S.A. Development of Ventilatory Response to Transient Hypercapnia and Hypercapnic Hypoxia in Term Infants SIGNE SØVIK AND KRISTIN LOSSIUS Department of Physiology, Institute of Basic Medical Sciences, University of Oslo, NO-0317 Oslo [S.S.], and Section of Neonatology, Department of Pediatrics, Rikshospitalet, NO–0027 Oslo [K.L.], Norway ABSTRACT Whereas peripheral chemoreceptor oxygen sensitivity in- was unchanged for hypoxia. Response magnitude was unchanged creases markedly after birth, previous studies of ventilatory for hypercapnia, but increased for the two hypoxic stimuli. In responses to CO2 in term infants have shown no postnatal conclusion, an interaction between the effects of hypercapnia and development. However, the hypercapnic challenges applied have hypoxia on ventilatory response rate emerged between postnatal usually been long-term, which meant that the effect of central d 2 and wk 8 in term infants. Concomitantly, stimulus-response chemoreceptors dominated. Oscillatory breathing, apneas, and time to hypercapnic stimuli declined markedly. The development sighs cause transient PCO2 changes, probably primarily stimulat- of a prompt response to transient hypercapnia may be important ing peripheral chemoreceptors. We wanted to assess whether the for infant respiratory stability. (Pediatr Res 55: 302–309, 2004) immediate ventilatory responses to step changes in inspired CO2 and O2 in term infants undergo postnatal developmental changes. Twenty-six healthy term infants were studied during natural Abbreviations sleep 2 d and 8 wk postnatally. Ventilatory responses to a FiCO2, fraction of inspired carbon dioxide randomized sequence of 15 s hypercapnia (3% CO2), hypoxia fR, respiratory rate ϩ (15% O2), and hypercapnic hypoxia (3% CO2 15% O2) were PaCO2, partial pressure of arterial carbon dioxide recorded breath-by-breath using a pneumotachometer. -

Effects of Intrapulmonary Percussive Ventilation on Airway Mucus Clearance: a Bench Model 11/2/17, 7�22 AM
Effects of intrapulmonary percussive ventilation on airway mucus clearance: A bench model 11/2/17, 7'22 AM World J Crit Care Med. 2017 Aug 4; 6(3): 164–171. PMCID: PMC5547430 Published online 2017 Aug 4. doi: 10.5492/wjccm.v6.i3.164 Effects of intrapulmonary percussive ventilation on airway mucus clearance: A bench model Lorena Fernandez-Restrepo, Lauren Shaffer, Bravein Amalakuhan, Marcos I Restrepo, Jay Peters, and Ruben Restrepo Lorena Fernandez-Restrepo, Lauren Shaffer, Bravein Amalakuhan, Marcos I Restrepo, Jay Peters, Ruben Restrepo, Division of Pediatric Critical Care, Division of Pulmonary and Critical Care, and Department of Respiratory Care, University of Texas Health Science Center and the South Texas Veterans Health Care System, San Antonio, TX 78240, United States Author contributions: All authors contributed equally to the literature search, data collection, study design and analysis, manuscript preparation and final review. Correspondence to: Dr. Bravein Amalakuhan, MD, Division of Pediatric Critical Care, Division of Pulmonary and Critical Care, and Department of Respiratory Care, University of Texas Health Science Center and the South Texas Veterans Health Care System, 7400 Merton Minter Blvd, San Antonio, TX 78240, United States. [email protected] Telephone: +1-210-5675792 Fax: +1-210-9493006 Received 2017 May 7; Revised 2017 Jun 1; Accepted 2017 Jun 30. Copyright ©The Author(s) 2017. Published by Baishideng Publishing Group Inc. All rights reserved. Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. -
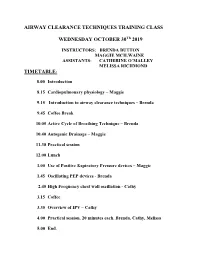
Introduction to Airway Clearance Techniques – Brenda
AIRWAY CLEARANCE TECHNIQUES TRAINING CLASS WEDNESDAY OCTOBER 30Th 2019 INSTRUCTORS: BRENDA BUTTON MAGGIE MCILWAINE ASSISTANTS: CATHERINE O’MALLEY MELISSA RICHMOND TIMETABLE: 8.00 Introduction 8.15 Cardiopulmonary physiology – Maggie 9.15 Introduction to airway clearance techniques – Brenda 9.45 Coffee Break 10.05 Active Cycle of Breathing Technique – Brenda 10.40 Autogenic Drainage – Maggie 11.30 Practical session 12.00 Lunch 1.00 Use of Positive Expiratory Pressure devices – Maggie 1.45 Oscillating PEP devices - Brenda 2.45 High Frequency chest wall oscillation - Cathy 3.15 Coffee 3.35 Overview of IPV – Cathy 4.00 Practical session. 20 minutes each. Brenda, Cathy, Melissa 5.00 End. 8/1/2019 Airway Clearance Techniques Training class Dr Maggie McIlwaine and Dr Brenda Button Catherine O’Malley Melissa Richmond Objectives • Explain the physiology, and theory behind airway clearance techniques currently used in the treatment of cystic fibrosis. • Demonstrate the airway clearance techniques of Active cycle of breathing techniques, autogenic drainage, PEP, oscillating PEP, HFCWO and IPV. • Compose the scientific evidence supporting the use of each of these techniques. Timetable • 8.00 Introduction: Maggie • 8.15 Cardiopulmonary physiology – Maggie • 9.15 Introduction to airway clearance and breathing techniques – Brenda • 9.45 Coffee break • 10.05 The Active Cycle of Breathing Techniques - Brenda • 10.40 Autogenic Drainage Maggie • 11.30 Practical session • 12.00 Lunch M. McIlwaine 1 8/1/2019 Timetable • 1.00 Use of Positive Expiratory Pressure Devices – Maggie • 1.45 Oscillating PEP Devices – Brenda • 2.45 C High Frequency Chest wall Oscillation (HFCWO) therapy-Coffee • 3.15 Coffee • 3.35 Overview of IPV – Cathy • 4.00 Practical session.