Proceedings from the 15Th Scandinavian Conference on Health Informatics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Vessel Import to Norway in the First Millennium AD Composition And
VESSEL IMPORT TO NORWAY IN THE FIRST MILLENNIUM A.D Composition and context. by Ingegerd Roland Ph.D. thesis. Institute of Archaeology, University College London, June 1996. ProQuest Number: 10017303 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a complete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. uest. ProQuest 10017303 Published by ProQuest LLC(2016). Copyright of the Dissertation is held by the Author. All rights reserved. This work is protected against unauthorized copying under Title 17, United States Code. Microform Edition © ProQuest LLC. ProQuest LLC 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106-1346 Abstract : More than 1100 complete or fragmentary imported vessels in bronze, glass, wood, horn, clay and silver from the first millennium A.D. have been found in Norway, approximately 80% of them in graves. The extensive research already carried out has produced a vast body of literature, which generally keeps within strict chronological boundaries, concentrating on vessels from either the Roman Period, the Migration Period, or the Viking Age. Two main approaches to the material have traditionally been applied: 1) typo logical studies, on the basis of which trade connections and systems have been discussed from different theoretical perspectives, and 2) imports as status markers, from which hierarchical social systems of a general kind have been inferred. Only very rarely have their function as vessels attracted any serious consideration, and even more rarely their actual local context. -

Lillesand-Flaksvandsbanen 1896-1953 Og Annet Med Tilknytning Til Flaksvatn
Veiledningstjenesten ved Birkenes Skolestyrekontor: Lillesand-Flaksvandsbanen 1896-1953 og annet med tilknytning til Flaksvatn Åsmund Knutson Lokale ressurser i undervisningen Forord «Lillesand – Flaksvandsbanen og annet med tilknytning til Flaksvatn» er et nytt hefte av pensjonert skolesjef Åsmund Knutson. En del av stoffet har stått i årsskriftet til Birkenes Historielag (Årsskrift 7, 1988), mens de andre kapitlene ikke har vært utgitt før. Hensikten med heftet er å gjøre stoffet tilgjengelig for skoleelevene i Birkenes og andre interesserte. De siste årene er det flere som har spurt etter stoff om «Lillesand – Flaksvandsbanen». I tillegg til stoffet i dette heftet viser vi til det tidligere utgitte heftet «Flaksvand Dampsag og Høvleri». De fleste bildene er ved Johannes Agerbo. Veiledningstjenesten ved Birkenes Skolestyrekontor 07.02.94 Einar Ytrehus - ped. kons. - INNHOLD Lillesand-Flaksvandsbanen 1896-1953 s. 2 Kjerraten ved Flaksvatn 1896-1953 s. 13 Flaksvand bom 1671-1981 s. 20 Osen s. 22 Det første industristedet i Birkenes s. 26 1 Lillesand-Flaksvandsbanen 1896-1953 av Åsmund Knutson Lillesand-Flaksvandsbanen (LFB) skapte ei optimistisk stemning og en tiltakslyst også utenfor anleggskommunene Lillesand, Vestre Moland og Birkenes. Det viser protokollen etter et jernbanemøte 22. oktober 1889 i Åmlid i Søre Herefoss. På det møtet ble anleggskostnaden for jernbanen fordelt mellom de interesserte kommunene. I den fordelinga, som siden ble noe forandra, tok også disse kommunene sin del av utgiftene: Herefoss, Vegusdal, Mykland, Åmli og Lille Tovdal. Men det var i Birkenes virkningen av jernbanen ble mest synlig. Der ble anlagt store bedrifter og bygd nye handelshus. Og nybyggere strømte til bygda, særlig til Birkeland, og slo seg ned med nye virksomheter. -
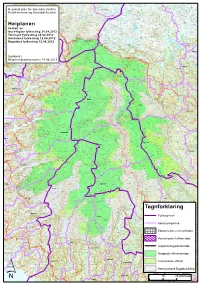
Tegnforklaring
Synken Mårs- Furebergsdalen Kallungsjå- Rosjå hovda Mosdalen Krokavasshallet Blyvarden hovdun Mårsnos Dargesjå- brotet Såta Litlosvatnet Ysteinsbu Krokavatni nutane Skardbu Reksjå Stegaros Hansbu Roflott Gjerdmunds- Svoldal Ænesdalen Fonnabu Breiabu Darge- Kringlesjåen Slettedalsbu Hauge Storekoll Kalhovd hamn Lyng- Svartavass- Odda sjåen Sletteåi Kalhovdfjorden Juklavassrusti Kvenno Gjuvsjåen Reksjåeggen turisthytte Sauhovd Langa- Vassdalsvatni Stordals- stranda horga Ruklenuten Juklavotni Kvennsjøen Skardvatnet Bondhus- Nusstjønn Gygrastolen vatnet Breia- Nordre nutan Hatlestranda Årsnes Mannsåker Kvanntjørnsbu Vetlekoll Storfjell Stordalsbu brea Eide vatnet Belebotnen L å v e n Kringlesjå- Nordlifjellet Mjågevatn Gryslehovda Viervatnet Geitebu- Bjørnsbu Jordal Holmavassnuten Søre Grinde- Steinbu- Rossnos nuten fjorden Ruklenuten Hovlandsstølen Sandvatn Vråsjålega Kils- Buerdalen Sandve- Stridfalls- tangen fjellet Nesflott Ask Myrdalsvatnet Kvennedalen Grytefjorden hovde Folgefonna nasjonalpark vatnet Ullensvang Honserud- Nedsta Kilsfjorden Kortmark Nordvollen Strond nuten Juklavass- Solfonn Vråsjåen Teigen nibba Graveide Løfalls- Sjausetedalen Holmavatnet Øvsta Bjørnabu Sandbekk RegionalKvinnherad plan for Setesdal Vesthei nutane Gunleiksbu- Vollehytta Haraldsjå stranda Bjørnavatnet Mogen Belganuten vatnet Argehovd store Skarvatun Melderskin Hildalsdalen Brasfetnuten Briskevatnet vesle S k a r d - Bjørnadalen Simle- Kvenna Lii Saure Saure Haraldsjå Møra Bjørndals- Sandvin Svervenuten Vollevatnet Gøystavatnet store Hildalselvi Eltar- -

Birkenes, Herefoss Og Vegusdal 2015
Nr. 4 2015 49. årgang BLADET MENIGHETSBirkenes, Herefoss og Vegusdal God Jul! På den andre sida God jul Kirkebussen Dette blir en julehilsen fra meg til deg. Kirkebussen til Birkenes Og jeg legger ved en skisse av Mollestadeika i Birkenes. Denne eika som kirke er et tilbud som mange er ca. 1000 år gammel, er Norges tredje største tre med en omkrets på benytter seg av. Men vi skulle 10,5 meter (målt i 50 cm. høyde). Denne kjempen får stå som et symbol så gjerne hatt flere sjåfører på julebudskapet, godt rotfestet, gammelt, men med nye spirer. med minibuss-sertifikat. Dersom du kunne tenkt deg å For meg blir eika et symbol på noe som står fast, juleevangeliet gjelder bidra noen få ganger i løpet av som en evig beskjed til menneskeheten om at Gud har bøyd seg ned og et år, ber vi deg kontakte Olav iverksatt sin redningsplan. Birkeland eller kirkekontoret. Dette nummeret inneholder mange bilder av jubilerende konfirmanter. Ellers minner vi alle brukere 50 år har gått siden dåpsløftet ble fornyet. Eika står, – og løftet gjelder av tilbudet om at bussen fortsatt. Og Herefoss kirke er 150 år. starter ved sykehjemmet, beveger seg ned Strøket før den Dagens konfirmanter har vært på konfirmantleir på Evjetun. Eika er finner korteste vegen til kirka. gammel nå, men også siste sommer maktet den å produsere nye skudd. Tur/retur koster 20 kroner. La oss som menighet stelle godt med ungdommen. Troen skapes ofte i unge år. Vi møter den nye presten. Hvordan skal han makte å kombinere tradisjon og nytenking. -
Innkalling Til Styremøte I Aust-Agder Utviklings- Og Kompetansefond
Aust-Agder utviklings- og kompetansefond (16.02.2018) Saksdokumenter med vedlegg Saksliste Godkjenning av innkalling Godkjenning av sakskart Styresaker 24/18 Godkjenning av protokoll fra forrige styremøte 2.2.2018 3 25/18 Oppfølging av tildelte tilskudd til 16. februar 2018 26 26/18 Avkastning på fondets kapital pr. 31.1.2018 34 27/18 Digitalt Innovasjonsprogram for USUS-bedrifter - Oppdatert prosjektbeskrivelse 2018 40 28/18 Søknad fra Setesdal regionråd – Distriktsvenleg helsesøsterutdanning 53 29/18 Søknad fra FK Jerv og Blå Kors: Holdningskampanjer 90 30/18 Søknad fra Universitetet i Agder: Innføring av velferdsteknologi, Agder 112 31/18 Søknad fra Universitetet i Agder: Flyktningbarns møte med barnehager og lokalmiljøer på Agder 124 32/18 Søknad fra Universitetet i Agder: På vei mot uføre? 140 33/18 Søknad fra Agderforskning AS: Våre strender - vår velferd 153 34/18 Søknad fra Evjeklinikken AS: Ny livsstil - Ung Folkehelse - Folkehøgskolen Helse 169 35/18 Søknad fra Durapart AS: Minoritetsspråklige menn i arbeid 216 36/18 Søknad fra Fafo: Virksomheters samfunnsansvar og likestilt arbeidsliv 229 37/18 Søknad fra Refugee+ AS: Refugee + 242 38/18 Diverse søknader til Aust-Agder utviklings- og kompetansefond 2017/18 260 39/18 Søknad unntatt offentlighet 470 40/18 Eventuelt til 16.02.2018 482 24/18 Godkjenning av protokoll fra forrige styremøte 2.2.2018 - 17/10871-24 Godkjenning av protokoll fra forrige styremøte 2.2.2018 : Godkjenning av protokoll fra forrige styremøte 2.2.2018 Saksframlegg Arkivsak-dok. 17/10871-24 Saksbehandler Lisbeth Ramsdal Utvalg Møtedato Aust-Agder utviklings- og kompetansefond 16.02.2018 Godkjenning av protokoll fra forrige styremøte 2.2.2018 1. -

Temaplan KULTURMINNER I BIRKENES KOMMUNE
Lillesand- Flaksvandsbanen gikk mellom Flaksvann og Lillesand fra 1896 til 1953 og toget fraktet blant annet tømmer fra Flaksvann Temaplan KULTURMINNER I BIRKENES KOMMUNE 2020-2028 1 Forord Riksantikvarens definisjon av et kulturminne sier at «Kulturminner er alle spor etter menneskers liv og virke i vårt fysiske miljø. Begrepet omfatter også steder knyttet til historiske hendelser, tro eller tradisjon. Også naturelementer med kulturhistorisk verdi er kulturminner, eller kan inngå som en del av et kulturminne.» Temaplan for kulturminner er den første kulturminneplan som er laget for Birkenes kommune. Tekstdelen i planen munner ut i en 4-årig tiltaksplan samt en langtidsplan, som må koples til økonomiplanen ved årlig rullering. Både kommuneplan, økonomiplan og regionale og statlige retningslinjer legger føringer for arbeidet med kulturminner. Det er et ønske at man gjennom en vedtatt kulturminneplan får tatt vare på noen av våre viktigste kulturminner. Ordfører Gyro Heia 2 Innhold 1. Innledning ................................................................................................................................................. 5 1.1. Mål for planen.................................................................................................................................. 5 1.2. Plantype, avgrensning av planen ............................................................................................. 5 1.2.1 Verneverdig bebyggelse ....................................................................................................