Nutrition in Cirrhosis: a Guide for Patients
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
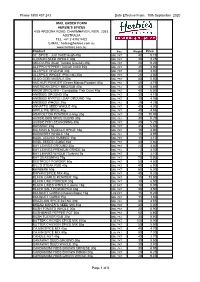
10Th September 2020 MAIL ORDER FORM
Phone 1800 437 243 Date Effective From: 10th September 2020 MAIL ORDER FORM HERBIE'S SPICES 4/25 ARIZONA ROAD, CHARMHAVEN, NSW, 2263, AUSTRALIA TEL: +61 2 4392 9422 E-MAIL: [email protected] www.herbies.com.au Product Size Weight Price 32° SPICE - Just Hot Enough 40g SML PKT 40 5.10 AJOWAN SEED WHOLE 30g SML PKT 30 3.25 AKUDJURA (Bush Tomato Ground) 20g SML PKT 20 9.20 ALEPPO PEPPER (Turkish Chilli) 35g SML PKT 35 4.90 ALLSPICE GROUND 30g SML PKT 30 3.60 ALLSPICE WHOLE (Pimento) 25g SML PKT 25 3.50 ALOO GOBI MASALA 40g SML PKT 40 5.50 AMCHUR POWDER (Green Mango Powder) 45g SML PKT 45 4.75 AMERICAN SPICY BBQ RUB 40g SML PKT 40 5.85 AMOK SPICE MIX - Cambodian Fish Curry 40g SML PKT 40 6.50 ANISEED GROUND 30g SML PKT 30 4.10 ANISEED MYRTLE LEAF GROUND 10g SML PKT 10 4.95 ANISEED WHOLE 25g SML PKT 25 4.25 ANNATTO SEED WHOLE 40g SML PKT 40 4.30 APPLE PIE SPICE 40g SML PKT 40 4.95 ASAFOETIDA POWDER (Hing) 20g SML PKT 20 10.95 AUSSIE BBQ SPICE BLEND 30g SML PKT 30 5.20 AUSSIE FISH SEASONING 30g SML PKT 30 5.20 BAHARAT 45g SML PKT 45 5.50 BALMAIN & ROZELLE SPICE 18g SML PKT 18 4.90 BARBERRY WHOLE 15g SML PKT 15 3.95 BASIL LEAVES RUBBED 15g SML PKT 15 3.10 BASIL SEEDS (Subja) 40g SML PKT 40 5.80 BAY LEAVES GROUND 20g SML PKT 20 4.80 BAY LEAVES PREMIUM GRADE 3g SML PKT 3 4.00 BAY LEAVES WHOLE (Turkish) 7g SML PKT 7 3.10 BAY SEASONING 75g SML PKT 75 5.50 BEETROOT POWDER 50g SML PKT 50 4.80 BILL'S STEAK RUB 40g SML PKT 40 6.90 BERBERE 50g SML PKT 50 5.30 BIRYANI SPICE MIX 40g SML PKT 40 5.20 BLACK GARLIC POWDER 15g SML PKT 15 13.50 BLACK LIME -

Cured and Air Dried 1
Cured and Air Dried 1. Sobrasada Bellota Ibérico 2. Jamón Serrano 18 month 3. Mini Cooking Chorizo 4. Morcilla 5. Chorizo Ibérico Bellota Cure and simple Good meat, salt, smoke, time. The fundamentals of great curing are not complicated, so it’s extraordinary just how many different styles, flavours and textures can be found around the world. We’ve spent 20 years tracking down the very best in a cured meat odyssey that has seen us wander beneath holm oak trees in the Spanish dehesa, climb mountains in Italy and get hopelessly lost in the Scottish Highlands. The meaty treasures we’ve brought back range from hams and sausages to salamis and coppas, each with their own story to tell and unique flavours that are specific to a particular place. 1. An ancient art 4. The practice of preserving meat by drying, salting or smoking stretches back thousands of years and while the process has evolved, there has been a renaissance in traditional skills and techniques in recent years. Many of our artisan producers work in much the same way as their forefathers would have, creating truly authentic, exquisite flavours. If you would like to order from our range or want to know more about a product, please contact your Harvey & Brockless account manager or speak to our customer support team. 3. 2. 5. Smoked Air Dried Pork Loin Sliced 90g CA248 British Suffolk Salami, Brundish, Suffolk The latest edition to the Suffolk Salami range, cured and There’s been a cured meat revolution in the UK in recent years smoked on the farm it is a delicate finely textured meat that with a new generation of artisan producers developing air dried should be savoured as the focus of an antipasti board. -
The Effects of Beef Liver on the Growth of Catfish and Goldfish
THE EFFECTS OF BEEF LIVER ON THE GROWTH OF CATFISH AND GOLDFISH by MARION ISABELL CAMPBELL B. S., Kansas State Teachers College, Pittsburg, 1924 A THESIS submitted in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE KANSAS STATE AGRICULTURAL COLLEGE 1930 2 TABLE OF CONTENTS page INTRODUCTION 2 REVIEW OF LITERATURE 3 METHODS 4 DISCUSSION 8 SUMMARY 18 ACKNOWLEDGMENTS 19 BIBLIOGRAPHY 20 PLATES 21 INTRODUCTION In experiments worked out by Edward Schneberger, under the direction of Dr. Minna E. Jewell in 1928-29 at the Kansas State Agricultural College, fish fed a diet contain- ing liver gained more in growth than those fed a non-liver diet. These results suggested the following questions: 1. Is liver just a desirable source of protein in the diet of catfish and goldfish or is some other growth factor contained in it? 2. Is the amount of liver a factor in the rate of growth of catfish and goldfish? 3 These studies were made under the direction of Dr. Edward J. Wimmer of the Kansas State Agricultural College under the auspices of the Zoology Department of the Kansas State Agricultural College. REVIEW OF LITERATURE The field of fish nutrition is comparatively new. Liver has always been a favorite food among hatchery people, because fish eat it readily and it has fulfilled the requirements of an adequate diet. Pearse (1925) worked out the chemical composition of certain fresh water fishes and found the body to contain an average of 2.44 per cent nitrogen for the year. This would be supplied by the protein content of the food. -

Liver-Healthy Shopping Guide
Liver-healthy Shopping Guide The liver is the world’s most efficient battery. It helps power your body by storing and releasing energy when you need it. Your liver plays a key role in converting food into the chemicals essential for life and it is therefore important to make food choices that optimize liver health. Although there is no specific ‘liver health diet’, these general guidelines will help ensure that your liver is functioning at its best: General Guidelines: • Choose a variety of foods from all four food groups of Canada’s Food Guide to Healthy Eating (http://www.hc-sc.gc.ca/fn-an/food-guide- aliment/index_e.html ). Focus on lower fat choices within each food group. • Eat at least 2 servings from the Meat & Alternatives food group (meat, fish, poultry, peanut butter, dried beans, peas, lentils). • Eat small regular meals. Do not skip meals or over-eat. • Drink 6 to 8 glasses of fluids (preferably water) a day. • Avoid alcohol – or if you drink, do not have more than one to two drinks per occasion (and never on a daily basis). • Consult your doctor if you are considering taking vitamins or herbal supplements. Particular herbal supplements have the potential to cause liver damage and certain vitamins may be harmful to the liver if taken in high doses, particularly vitamin A. • Choose organic foods whenever possible: The less pesticides/chemicals/antibiotics/hormones, the less your liver has to filter. • Fresh is generally best e.g. firm and clean, organic and in-season produce • Wash fruit and vegetables right before use to remove pesticides. -
Meat Curing and Sodium Nitrite
MEDIA MYTHCRUSHER Meat Curing and Sodium Nitrite The use of nitrite to produce cured meats like salami, ham, bacon and hot dogs, is a safe, regulated practice that has distinct public health benefits. However, much confusion and even mythology surrounds nitrite. Being mindful of key words and statistics and providing appropriate context can help reporters improve the accuracy of their coverage and the information that is passed on to readers and viewers. We’ve compiled ten tips to improve accuracy when writing about the use of sodium nitrite in cured meats. #1: Nitrite is not ‘unnatural’. Before the terms nitrate and nitrite are often used refrigeration was available, humans salted and interchangeably, meat companies mainly use dried meat to preserve it. It was discovered sodium nitrite to cure meat, not sodium nitrate. that the nitrate in saltpeter was extremely At the turn of the 20th century, German effective in causing a chemical reaction known scientists discovered nitrite (and not nitrate) as “curing.” Not only did this give meat a was the active form of these curing salts. When distinct taste and flavor, it also preserved it and added directly, rather than as nitrate, meat prevented the growth of Clostridium botulinum, processors can have better control of this which causes botulism. important curing ingredient and more closely manage how much they are adding. Later on, scientists came to understand that nitrate naturally found in the environment #3: Cured meats are a miniscule source of converts to nitrite when in the presence of total human nitrite intake. Scientists say that certain bacteria. -

Retail Catalog
MONTANA TEA & SPICE TRADING LLC SPRING 2020 RETAIL PRICE GUIDE VIRUS: OUTLET STORE WHILE THE STORE IS NOT OPEN FOR WALK-INS, YOU CAN: CALL, ORDER, PAY THEN PICK UP 10:30 - 3:30 Mon-Fri TO ORDER : E MAIL , F AX , C ALL US or MAIL IN ONLINE ORDERING UNAVAILABLE P.O. B OX 8082 MISSOULA MT 59807 Phone 406/721-4882 Fax 406/543-1126 [email protected] BLENDING TEAS SINCE 1972 G H T B 1lb bulk loose tea: 20.00 ERBA MAT% BLENDS Herbal Packages: 1oz 2.00 3oz 4.55 and ROOIBOS BLENDS Tea Teabags (if available ) 1 lb 21.25 1oz 2.10 3oz 4.85 Prices: ♥6pk teabags 2.10 ♥24pk teabags 4.65 teabags: ♥6pk 2.20 ♥24pk 4.95 PREMIER BLENDS MO,HA BLENDS ERBA MAT% . BLENDS Blueberry Hill ocha Almandine Green Caribbean Afternoon ocha Blac) ,aspberry ,oasted Copperfield ocha .ouble Chocolate 0erba Chocolate Hazelnut Early Light ocha .ouble Vanilla 0erba Cinnamon Chocolate Evening In issoula 1 lb 21.25 ocha Ginseng 0erba Citrus Fruit Of The Plain ocha Gingersnap 0erba Five Valleys Chai 1 lb 25.50 Harvest Time ocha Hazelnut 1 oz 2.35 3 oz 5.65 ontana Gold 1 lb 21.25 ocha int 0erba Huc)leberry orning eadows ocha L'Orange 0erba ocha Chocolate ountain Huc)leberry ocha ,um ,oyal 0erba Orange int Night On Glacier Bay MO-NTAIN SPI,E BLENDS 0erba ,aspberry Spice Purple ountains ajesty ountain Apple Spice ROOIBOS . BLENDS ,aspberry Sunrise ♥ ountain Apricot Spice ,ooibos Red Bush tea Africa ,ed ,over ountain Blac)berry Spice Anise Bush Starfire Licorice ountain Cherry Spice Apple Bush Strawberry Sunset ountain Orange Spice Apricot Bush Summer -

Atypical Abdominal Pain in a Patient with Liver Cirrhosis
IMAGE IN HEPATOLOGY January-February, Vol. 17 No. 1, 2018: 162-164 The Official Journal of the Mexican Association of Hepatology, the Latin-American Association for Study of the Liver and the Canadian Association for the Study of the Liver Atypical Abdominal Pain in a Patient With Liver Cirrhosis Liz Toapanta-Yanchapaxi,* Eid-Lidt Guering,** Ignacio García-Juárez* * Gastroenterology Department. National Institute of Medical Science and Nutrition “Salvador Zubirán”. Mexico City. Mexico. ** Interventional Cardiology. National Institute of Cardiology “Ignacio Chávez”. Mexico City. Mexico. ABSTRACTABSTABSTABSTRACT The causes of abdominal pain in patients with liver cirrhosis and ascites are well-known but occasionally, atypical causes arise. We report the case of a patient with a ruptured, confined abdominal aortic aneurysm. KeyK words.o d .K .Key Liver cirrhosis. Abdominal aortic aneurysm. INTRODUCTION CASE REPORT Abdominal pain in cirrhotic patients is a challenge. A 47-year-old male with the established diagnosis of Clinical presentation can be non-specific and the need for alcohol-related liver cirrhosis, presented to the emer- early surgical exploration may be difficult to assess. Coag- gency department for abdominal pain. He was classified ulopathy, thrombocytopenia, varices, and ascites need to as Child Pugh (CP) C stage (10 points) and had a model be taken into account, since they can increase the surgical for end stage liver disease (MELD) - sodium (Na) of 21 risk. Possible differential diagnoses include: Complicated points. The pain was referred to the left iliac fossa, with umbilical, inguinal or postoperative incisional hernias, an intensity of 10/10. It was associated to low back pain acute cholecystitis, spontaneous bacterial peritonitis, pep- with radicular stigmata (primarily S1). -

Starters & Sharers the Rest from the Sea Sides Salads
WEDNESDAYS FRIDAYS SATURDAYS SUNDAYS GOURMET STEAK NIGHT SEAFOOD SATURDAYS SUNDAY SOCIAL BURGER NIGHT 21 day aged steaks cooked over charcoal 3 seafood specials, Relax and enjoy our fabulous brunch menu Sirloin, Fillet and T-Bone from the pier to the pan as fast as we can! whilst catching up on the Sunday papers All burgers £10, for one night only 3 fish specials from today’s catch Look out for our locally sourced specials Served from 6.30pm till 9.30pm Available from 5pm Served 10.30am till 12.30pm STARTERS & SHARERS FROM THE SEA — — TRIO OF HAGGIS £6.99 CRISPY FRIED ISLE OF MULL SCALLOPS GOURMET SCAMPI Haggis pakora, mini haggis pie and MORANGIE BRIE £6.99 £17.99 & CHIPS £13.99 haggis bon bon Ripe Scottish Brie, crispy fried in rosemary Creamy mash, venison chorizo and a wild Bread crumbed whole langoustine tails . crumb and served with whisky apple mushroom sauce served with Cuan fries and homemade SEAFOOD PLATTER chutney . tartare sauce FOR 2 £14.99 . FISH AND CHIPS £10.99 . Hot smoked Scottish salmon, smoked TASTER PLATTER Chunky fillet of haddock, crispy fried in TODAY’S TRIO £13.99 mackerel, prawn cocktail, rollmop herring our special recipe batter and served with Served over rumbledethump potatoes with FOR 2 £14.99 Cuan fries and home- made tartare sauce and crab timbale. Served with dips and Mini haggis pie, Great Glen Venison a Arran cheddar and chive cream sauce . crusty bread Salami, Cuan Mor Pate, black pudding . scotch egg and crispy fried Morangie Brie. SCRABSTER LANDED LOCAL SALMON FILLET GREAT GLEN VENISON Served with chutneys and crusty bread COLEY FILLET £12.50 £13.50 SALAMI CROSTINI £6.99 . -

The Evaluation of Pathogen Survival in Dry Cured Charcuterie Style Sausages
University of Kentucky UKnowledge Theses and Dissertations--Animal and Food Sciences Animal and Food Sciences 2019 THE EVALUATION OF PATHOGEN SURVIVAL IN DRY CURED CHARCUTERIE STYLE SAUSAGES Jennifer Michelle McNeil University of Kentucky, [email protected] Digital Object Identifier: https://doi.org/10.13023/etd.2019.074 Right click to open a feedback form in a new tab to let us know how this document benefits ou.y Recommended Citation McNeil, Jennifer Michelle, "THE EVALUATION OF PATHOGEN SURVIVAL IN DRY CURED CHARCUTERIE STYLE SAUSAGES" (2019). Theses and Dissertations--Animal and Food Sciences. 102. https://uknowledge.uky.edu/animalsci_etds/102 This Master's Thesis is brought to you for free and open access by the Animal and Food Sciences at UKnowledge. It has been accepted for inclusion in Theses and Dissertations--Animal and Food Sciences by an authorized administrator of UKnowledge. For more information, please contact [email protected]. STUDENT AGREEMENT: I represent that my thesis or dissertation and abstract are my original work. Proper attribution has been given to all outside sources. I understand that I am solely responsible for obtaining any needed copyright permissions. I have obtained needed written permission statement(s) from the owner(s) of each third-party copyrighted matter to be included in my work, allowing electronic distribution (if such use is not permitted by the fair use doctrine) which will be submitted to UKnowledge as Additional File. I hereby grant to The University of Kentucky and its agents the irrevocable, non-exclusive, and royalty-free license to archive and make accessible my work in whole or in part in all forms of media, now or hereafter known. -

High Risk Percutaneous Endoscopic Gastrostomy Tubes: Issues to Consider
NUTRITIONINFLAMMATORY ISSUES BOWEL IN GASTROENTEROLOGY, DISEASE: A PRACTICAL SERIES APPROACH, #105 SERIES #73 Carol Rees Parrish, M.S., R.D., Series Editor High Risk Percutaneous Endoscopic Gastrostomy Tubes: Issues to Consider Iris Vance Neeral Shah Percutaneous endoscopy gastrostomy (PEG) tubes are a valuable tool for providing long- term enteral nutrition or gastric decompression; certain circumstances that complicate PEG placement warrant novel approaches and merit review and discussion. Ascites and portal hypertension with varices have been associated with poorer outcomes. Bleeding is one of the most common serious complications affecting approximately 2.5% of all procedures. This article will review what evidence exists in these high risk scenarios and attempt to provide more clarity when considering these challenging clinical circumstances. INTRODUCTION ince the first Percutaneous Endoscopic has been found by multiple authors to portend a poor Gastrostomy tube was placed in 1979 (1), they prognosis in PEG placement (3,4, 5,6,7,8). This review Shave become an invaluable tool for providing will endeavor to provide more clarity when considering long-term enteral nutrition (EN) and are commonly used these challenging clinical circumstances. in patients with dysphagia following stroke, disabling motor neuron diseases such as multiple sclerosis and Ascites & Gastric Varices amyotrophic lateral sclerosis, and in those with head The presence of ascites is frequently viewed as a and neck cancer.They are also used for patients with relative, if not absolute, contraindication to PEG prolonged mechanical intubation, as well as gastric placement. Ascites adds technical difficulties and the decompression in those with severe gastroparesis, risk for potential complications (see Table 1). -

Heart Health Through Whole Foods
Heart Health Through Whole Foods Certain whole foods in a diet can ultimately provide heart-healthy benefits. The right foods consumed in the right amounts can help lower cholesterol and/or triglycerides. They may also help to reduce risk for heart disease. Even though the benefits of whole foods may be known, too often individuals turn to over-the-counter supplements instead. It is important to discuss all supplements prior to ingestion with your physician. Individuals may not realize that taking some supplements with certain medications may be harmful or that taking too much of a good thing can be bad. The purpose of this session is to educate how to obtain certain nutrients through whole foods rather then through supplements. It must be noted that some individuals may still need supplements in addition to diet. Once again this should be guided by a physician. Supplement Health Benefits Caution Dietary Alternative Omega-3 Fatty Acids: Fish oil is used for There are some safety concerns Consuming fish oil from dietary Fish Oils reduction in cholesterol about using high doses of fish oil. sources such as fatty fish (e.g., and triglycerides. It is Doses greater than 3 grams per tuna, salmon), two servings Fish oils contain used for hyperlipidemia, day can inhibit blood coagulation per week, is associated with Eicosapentaenoic hypertriglyceridemia, and potentially increase the risk a reduced risk of developing Acid (EPA) and coronary heart disease of bleeding. Doses greater than 3 cardiovascular disease Docosahexaenoic and hypertension. grams per day might also suppress (primary prevention). Acid (DHA) immune response. -

Non-Alcoholic Fatty Liver Disease
NON-ALCOHOLIC FATTY LIVER DISEASE — A GUIDE TO — WHAT& HOW TO E AT TABLE OF CONTENTS PART 1 PART 2 • THE NORMAL LIVER • NUTRITION BASICS • THE LIVER WITH NON-ALCOHOLIC • WHAT ARE THE DIFFERENT FATTY LIVER DISEASE (NAFLD) FOOD GROUPS? • STAGES OF NON-ALCOHOLIC FATTY LIVER DISEASE PART 3 PART 4 • FOUR WAYS TO COOK VEGETABLES • TAKE A LOOK AT YOUR PLATE —MAKING RECIPES LIVER FRIENDLY • SAMPLE MEAL PLAN • GROCERY SHOPPING AND PLANNING MEALS • SNACKS & SMOOTHIES PART PART 1 THE LIVER AND NAFLD WHERE IS THE LIVER? The Iiver is one of the largest organs in the body. It is located in the upper right side of the belly. The liver is the only organ able to repair itself after injury. Your liver is essential to your life. You cannot live without it. THE LIVER— ASSISTS IN DIGESTION OF PROTEINS, FATS AND CARBOHYDRATES IS ESSENTIAL FOR DEVELOPING PROTEINS THAT SUPPORT OUR MUSCLE AND IMMUNE SYSTEM STORES AND RELEASES ENERGY, VITAMINS AND MINERALS HELPS MAINTAIN BLOOD SUGAR REMOVES TOXINS FROM THE BLOOD STREAM 2 WHAT IS NON-ALCOHOLIC FATTY LIVER DISEASE? Non-Alcoholic Fatty Liver Disease (NAFLD) results when liver cells become filled with fat. This fat can cause injury to the liver which can lead to cirrhosis, a severe condition where the liver is permanently scarred and damaged. Cirrhosis can lead to liver cancer or liver failure. You can control the progression of NAFLD by making the choice to change your diet and engage in daily activity. Most people do not know About 30% of U.S adults they have NAFLD, signs and have non-alcoholic fatty liver symptoms do not appear until disease.