Acr–Acnm–Snmmi–Spr Practice Parameter for the Performance of Gastrointestinal Tract, Hepatic, and Splenic Scintigraphy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nuclide Imaging: Planar Scintigraphy, SPECT, PET
Nuclide Imaging: Planar Scintigraphy, SPECT, PET Yao Wang Polytechnic University, Brooklyn, NY 11201 Based on J. L. Prince and J. M. Links, Medical Imaging Signals and Systems, and lecture notes by Prince. Figures are from the textbook except otherwise noted. Lecture Outline • Nuclide Imaging Overview • Review of Radioactive Decay • Planar Scintigraphy – Scintillation camera – Imaging equation • Single Photon Emission Computed Tomography (SPECT) • Positron Emission Tomography (PET) • Image Quality consideration – Resolution, noise, SNR, blurring EL5823 Nuclear Imaging Yao Wang, Polytechnic U., Brooklyn 2 What is Nuclear Medicine • Also known as nuclide imaging • Introduce radioactive substance into body • Allow for distribution and uptake/metabolism of compound ⇒ Functional Imaging ! • Detect regional variations of radioactivity as indication of presence or absence of specific physiologic function • Detection by “gamma camera” or detector array • (Image reconstruction) From H. Graber, Lecture Note for BMI1, F05 EL5823 Nuclear Imaging Yao Wang, Polytechnic U., Brooklyn 3 Examples: PET vs. CT • X-ray projection and tomography: – X-ray transmitted through a body from a outside source to a detector (transmission imaging) – Measuring anatomic structure • Nuclear medicine: – Gamma rays emitted from within a body (emission imaging) From H. Graber, Lecture Note, F05 – Imaging of functional or metabolic contrasts (not anatomic) • Brain perfusion, function • Myocardial perfusion • Tumor detection (metastases) EL5823 Nuclear Imaging Yao Wang, Polytechnic -

Description of Alternative Approaches to Measure and Place a Value on Hospital Products in Seven Oecd Countries
OECD Health Working Papers No. 56 Description of Alternative Approaches to Measure Luca Lorenzoni, and Place a Value Mark Pearson on Hospital Products in Seven OECD Countries https://dx.doi.org/10.1787/5kgdt91bpq24-en Unclassified DELSA/HEA/WD/HWP(2011)2 Organisation de Coopération et de Développement Économiques Organisation for Economic Co-operation and Development 14-Apr-2011 ___________________________________________________________________________________________ _____________ English text only DIRECTORATE FOR EMPLOYMENT, LABOUR AND SOCIAL AFFAIRS HEALTH COMMITTEE Unclassified DELSA/HEA/WD/HWP(2011)2 Health Working Papers OECD HEALTH WORKING PAPERS NO. 56 DESCRIPTION OF ALTERNATIVE APPROACHES TO MEASURE AND PLACE A VALUE ON HOSPITAL PRODUCTS IN SEVEN OECD COUNTRIES Luca Lorenzoni and Mark Pearson JEL Classification: H51, I12, and I19 English text only JT03300281 Document complet disponible sur OLIS dans son format d'origine Complete document available on OLIS in its original format DELSA/HEA/WD/HWP(2011)2 DIRECTORATE FOR EMPLOYMENT, LABOUR AND SOCIAL AFFAIRS www.oecd.org/els OECD HEALTH WORKING PAPERS http://www.oecd.org/els/health/workingpapers This series is designed to make available to a wider readership health studies prepared for use within the OECD. Authorship is usually collective, but principal writers are named. The papers are generally available only in their original language – English or French – with a summary in the other. Comment on the series is welcome, and should be sent to the Directorate for Employment, Labour and Social Affairs, 2, rue André-Pascal, 75775 PARIS CEDEX 16, France. The opinions expressed and arguments employed here are the responsibility of the author(s) and do not necessarily reflect those of the OECD. -

Severe Gastroparesis Following Radiofrequency Catheter Ablation for Atrial Fibrillation: Suggestion for Diagnosis, Treatment, and Device for Gastroparesis After RFCA
Hindawi Publishing Corporation Case Reports in Gastrointestinal Medicine Volume 2014, Article ID 923637, 6 pages http://dx.doi.org/10.1155/2014/923637 Case Report Severe Gastroparesis following Radiofrequency Catheter Ablation for Atrial Fibrillation: Suggestion for Diagnosis, Treatment, and Device for Gastroparesis after RFCA Dong Seok Lee1 and Sang Jin Lee1,2 1 Department of Internal Medicine, Gangneung Asan Medical Center, University of Ulsan College of Medicine, Gangneung, Republic of Korea 2Department of Internal Medicine, Gangneung Asan Medical Center, Sacheon-myeon, Gangneung, Gangwon-do 210-711, Republic of Korea Correspondence should be addressed to Sang Jin Lee; [email protected] Received 18 October 2014; Accepted 11 December 2014; Published 30 December 2014 Academic Editor: Wen-xie Xu Copyright © 2014 D. S. Lee and S. J. Lee. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Gastroparesis following radiofrequency catheter ablation (RFCA) is a very rare complication, as only two cases have been reported in the English literature. A 42-year-old man underwent RFCA due to recurrent drug-resistant symptomatic atrial fibrillation. The patient complained of indigestion and early satiety 2 days after the procedure. Contrast-enhanced computed tomography and an upper gastrointestinal series of the abdomen showed a large amount of material remaining in the stomach area. All food material was removed by endoscopy, and the patient received medical treatment. We suggest a flow chart for diagnosis and treatment of AFGS based on the present case and previous cases. -

Department of Medicine Lewis Katz School of Medicine at Temple University
Department of Medicine Lewis Katz School of Medicine at Temple University 2017 Annual Fellows, Residents and Medical Students Research Symposium Sol Sherry Awards for Excellence in Research Wednesday, June 7, 2017 Medical Education and Research Building Luo Commons The Fellows and Residents Research Forum was initiated over 35 years ago to provide the Fellows and the Residents in the Department of Medicine with an opportunity to present their research effort. The Forum is a reflection of the ongoing research activities in the Department, and a year-end summation of the projects carried out by the Fellows and Residents. Dedication Dr. Sol Sherry 1916-1993 Sol Sherry, M.D., joined Temple University School of Medicine as professor and chairman of the Department of Medicine in 1968. In 1970, Dr. Sherry founded and served as director of the University's Specialized Center for Thrombosis Research, the largest of its kind in the United States, which was later named in his honor. He served as dean of the School of Medicine from 1984-86. He was a recipient of an honorary doctor of science degree, the University's first Distinguished Professor and was honored with the establishment of the Sol Sherry Chair in Medicine. For his contributions to medical research, teaching and patient care, Dr. Sherry was the recipient of other numerous awards and honors. He was Master of the American College of Physicians and The John Phillips Memorial Medalist of the American College of Physicians; a Fellow of the Royal College of Physicians (London), and recipient of the Robert P. Grant Medal of the International Society on Thrombosis and Hemostasis--a society which he founded in 1977. -

Procedure Guideline for Planar Radionuclide Cardiac
Procedure Guideline for Planar Radionuclide Cardiac Ventriculogram for the Assessment of Left Ventricular Systolic Function Version 2 2016 Review date 2021 a b c d e e Alice Nicol , Mike Avison , Mark Harbinson , Steve Jeans , Wendy Waddington , Simon Woldman (on behalf of BNCS, BNMS, IPEM). a b Southern General Hospital, NHS Greater Glasgow & Clyde, Glasgow, UK Bradford Royal Infirmary, c d e Bradford, UK Queens University, Belfast, UK Christie Hospital NHS Foundation Trust, Manchester, UK University College London Hospitals NHS Foundation Trust, London, UK 1 1. Introduction The purpose of this guideline is to assist specialists in nuclear medicine in recommending, performing, interpreting and reporting radionuclide cardiac ventriculograms (RNVG), also commonly known as multiple gated acquisition (MUGA) scans. It will assist individual departments in the development and formulation of their own local protocols. RNVG is a reliable and robust method of assessing cardiac function [1-5]. The basis of the study is the acquisition of a nuclear medicine procedure with multiple frames, gated by the R wave of the electrocardiogram (ECG) signal. The tracer is a blood pool agent, usually red blood cells labelled with technetium-99m (99mTc). One aim of this guideline is to foster a more uniform method of performing RNVG scans throughout the United Kingdom. This is particularly desirable since the National Institute for Health and Clinical Excellence (NICE) has mandated national protocols for the pre-assessment and monitoring of patients undergoing certain chemotherapy regimes [6, 7], based on specific left ventricular ejection fraction (LVEF) criteria. This guideline will focus on planar equilibrium RNVG scans performed for the assessment of left ventricular systolic function at rest, using data acquired in the left anterior oblique (LAO) projection by means of a frame mode, ECG-gated acquisition method. -

Preparation Instructions for Nuclear Medicine Scans
NUCLEAR MEDICINE UNM HEALTH SCIENCES CENTER 2211 LOMAS NE ALBUQUERQUE, NM 87106 505-272-2421 (M-F 8:00AM – 4:30PM) Preparation Instructions for Nuclear Medicine Scans (Schedulers/Technologists: Please consult with Protocol sheets for additional important details) Procedure Preparation Duration of Exam Bone Scan No Prep Injection (15 minutes), then return 3 hours later for scan (45 minutes - 1 hour) Brain SPECT No Prep 1-1½ hours Cardiac perfusion – Technetium Agents See special instructions under Cardiac 3-5 hours preparation instructions Cisternogram and Cisternogram for Leak No Prep 2-3 days, 1-2 hours each day, morning and afternoon CSF Shunt Study No Prep Depending on each individual case Gallium Scan No Prep Depending on each individual case, usually requires multiple images over several days Gastric Emptying Scan (adults and Nothing by mouth for 6 hours except small 4-5 hours children approximately 4-5 yrs old and amount of water as needed for medications. up, with standardized meal of Egg Beaters, jam, and toast Diabetic patients should bring their usual diabetes medications (insulin and/or pills). Call Nuclear Medicine if you cannot eat Egg Beaters (egg whites), jam, or toast. Gastric Emptying Scan – Liquid – with Nothing by mouth for 4 hours 1-5 hours depending on protocol or without reflux (typically children Less time (2 hours) may be OK for infants and under 2-3 years old) very small children. Call Nuclear Medicine with questions. Gastrointestinal (GI) Bleeding Study No Prep 2-3 hours Glomerular Filtration Rate -- GFR (Gates Drink lots of fluids before the exam 15 minutes Method) Hemangioma No Prep 2-3 hours Hepatobiliary (HIDA) Scan For acute or chronic cholecystitis: 2 hours; may have to return for additional 1. -

Current Diagnosis and Treatment of Gastroparesis: a Systematic Literature Review
DOI: https://doi.org/10.22516/25007440.561 Review article Current diagnosis and treatment of gastroparesis: A systematic literature review Viviana Mayor,1* Diego Aponte,2 Robin Prieto,3 Emmanuel Orjuela.4 Abstract OPEN ACCESS Normal gastric emptying reflects a coordinated effort between different Citation: regions of the stomach and the duodenum, and also an extrinsic modu- Mayor V, Aponte D, Prieto R, Orjuela E. Current diagnosis and treatment of gastroparesis: lation by the central nervous system and distal bowel factors. The main A systematic literature review . Rev Colomb Gastroenterol. 2020;35(4):471-484. https://doi. org/10.22516/25007440.561 events related to normal gastric emptying include relaxation of the fundus to accommodate food, antral contractions to triturate large food particles, ............................................................................ the opening of the pyloric sphincter to allow the release of food from the 1 Internist and professor, Clínica Versailles, Universidad Javeriana. Cali, Colombia. stomach, and anthropyloroduodenal coordination for motor relaxation. 2 Gastroenterology Service, Area Coordinator, Clínica Universitaria Colombia. Bogotá, Colombia. Gastric dysmotility includes delayed emptying of the stomach (gastropare- 3 Gastroenterologist, Clínica Universitaria Colombia. Bogotá, Colombia. sis), accelerated gastric emptying (dumping syndrome), and other motor 4 Medical doctor. Universidad Javeriana. Clínica Versalles. Cali, Colombia. dysfunctions, e.g., deterioration of the distending fundus, -

III.2. POSITRON EMISSION TOMOGRAPHY – a NEW TECHNOLOGY in the NUCLEAR MEDICINE IMAGE DIAGNOSTICS (Short Review)
III.2. POSITRON EMISSION TOMOGRAPHY – A NEW TECHNOLOGY IN THE NUCLEAR MEDICINE IMAGE DIAGNOSTICS (Short review) Piperkova E, Georgiev R Dept.of Nuclear Medicine and Dept of Radiotherapy, National Oncological Centre Hospital, Sofia Positron Emission Tomography (PET) is a technology which makes fast advance in the field of Nuclear Medicine. It is different from the X-ray Computed Tomography and Magnetic Resonance Imaging (MRI), where mostly anatomical structures are shown and their functioning could be evaluated only indirectly. In addition, PET can visualise the biological nature and metabolite activity of the cells and tissues. It also has the capability for quantitative determination of the biochemical, physiological and pathological process in the human body (1). The spatial resolution of PET is usually 4-5mm and when the concentration of the positron emitter in the cells is high enough, it allows to see small size pathological zones with high proliferative and metabolite activity ( 3, 7, 17). Following fast and continuous improvement, PET imaging systems have advanced from the Bismuth Germanate Oxide (BGO) circular detector technology to the modern Lutetium Orthosilicate (LSO) and Gadolinium Orthosilicate (GSO) detectors (2, 7, 16). On the other hand, the construction technology has undergone significant progress in the development of new combined PET-CT and PET-MRI systems which currently replace the conventional PET systems with integrated transmission and emission detecting procedures, shown in Fig. 1. Fig. 1 A modern PET-CT system with one gantry. The sensitivity and the accuracy of PET based methods are found to be considerably higher compared to the other existing imaging methods and they can achieve 90-100% in the localisation of different oncological lesions (4, 11, 13, 14). -

Insurances, Precertification Requirements, Services Offered, As Well As Guidelines, Fees, and Education Information
This resource book is presented to provide you and your staff with basic information regarding: Insurances, precertification requirements, services offered, as well as guidelines, fees, and education information. This does not intend to be all encompassing, and some information does have limitations as well and expirations. Radiology Associates intends to keep you abreast of the newest and most up-to-date fees, guidelines, and regulations as we can. Please contact us if you have any further questions or we can be of further service to you. 887-7000 Radiology Associates, LLP Toll Free Phone 887-626-8678 General Correspondence and Billing Address: P.O. Box 5608 Corpus Christi, TX 78465 Patient Payment Address: P.O. Box 6010 Corpus Christi, TX 78466-6010 Business Office Physical Address: 1812 S. Alameda Corpus Christi, TX 78404 Mammogram Payment Guidelines Medicare Age 35–39 Baseline Mammogram Age 40+ Mammogram every year – (eleven full months must have elapsed following the month of the last mammogram) Note: Count months between mammographies beginning the month after the date of the examination. For example, screening mammogram received January 20, 2004; begin counting next month (February 2004) until 11 months have elapsed. Payment can be made for another screening mammogram beginning January 1, 2005. Medicaid (See Medicaid Guide) Age 35-39 Baseline Mammogram Age 45+ Mammogram every year (must be one full year) Tricare (Champus) (See Attached) Age 39+ Mammogram every year Age 35 High Risk and annually thereafter Note: women at high risk (family history of breast cancer in a first degree relative) baseline mammogram is payable at age 35 and then annually. -

Procedure Guideline for Equilibrium Radionuclide Ventriculography
Procedure Guideline for Equilibrium Radionuclide Ventriculography Mark D. Wittry, Jack E. Juni, Henry D. Royal, Gary V. Heller and Steven C. Port Saint Louis University, St. Louis, Missouri; William Beaumont Hospital, Royal Oak, Michigan; Mallinckrodt Institute of Radiology, St. Louis, Missouri; Hartford Hospital, Hartford, Connecticut; and Cardiovascular Associates, Ltd., Milwaukee, Wisconsin a. To distinguish ischemie from nonischemic causes. Key Words: gated blood-pool imaging;practice guideline;radionu- b. To distinguish systolic from diastolic causes. clide ventriculography; cardiac function; heart 3. Evaluation of cardiac function in patients undergoing J NucÃMed 1997; 38:1658-1661 chemotherapy. 4. Assessment of ventricular function in patients with PART I: PURPOSE valvular stenosis and/or insufficiency. The purpose of this guideline is to assist nuclear medicine An RVG may be used in the conditions listed above for: practitioners in recommending, performing, interpreting and (a) determining long-term prognosis, (b) assessing short- reporting the results of gated equilibrium radionuclide ventricu term risk (e.g., pre-operative evaluation) and (c) moni lography. toring the response to surgery or other therapeutic inter ventions. PART II: BACKGROUND INFORMATION AND DEFINITIONS Gated equilibrium radionuclide ventriculography (RVG) is a PART IV: PROCEDURE procedure in which the patient's blood is radiolabeled and A. Patient Preparation ECG-gated cardiac scintigraphy is obtained. Single or multiple 1. Rest measurements of left and/or right ventricular function are made. No special preparation is required for a resting RVG. Alternative terminologies for this technique include gated A fasting state is generally preferred. It is not neces cardiac blood-pool imaging, multigated acquisition (MUGA) sary to withhold any medications. -

Pet/Ct) Imaging
The American College of Radiology, with more than 30,000 members, is the principal organization of radiologists, radiation oncologists, and clinical medical physicists in the United States. The College is a nonprofit professional society whose primary purposes are to advance the science of radiology, improve radiologic services to the patient, study the socioeconomic aspects of the practice of radiology, and encourage continuing education for radiologists, radiation oncologists, medical physicists, and persons practicing in allied professional fields. The American College of Radiology will periodically define new practice parameters and technical standards for radiologic practice to help advance the science of radiology and to improve the quality of service to patients throughout the United States. Existing practice parameters and technical standards will be reviewed for revision or renewal, as appropriate, on their fifth anniversary or sooner, if indicated. Each practice parameter and technical standard, representing a policy statement by the College, has undergone a thorough consensus process in which it has been subjected to extensive review and approval. The practice parameters and technical standards recognize that the safe and effective use of diagnostic and therapeutic radiology requires specific training, skills, and techniques, as described in each document. Reproduction or modification of the published practice parameter and technical standard by those entities not providing these services is not authorized. Adopted 2017 (Resolution 26)* ACR–SPR–STR PRACTICE PARAMETER FOR THE PERFORMANCE OF CARDIAC POSITRON EMISSION TOMOGRAPHY - COMPUTED TOMOGRAPHY (PET/CT) IMAGING PREAMBLE This document is an educational tool designed to assist practitioners in providing appropriate radiologic care for patients. Practice Parameters and Technical Standards are not inflexible rules or requirements of practice and are not intended, nor should they be used, to establish a legal standard of care1. -
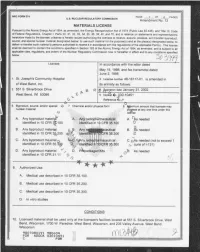
Matls Licensing Package for Amend 12 to License 48-16117-01 for St
_ _---____ -___ _ - _ _ _ _ _ _ _ _ - - _ _ _ _ _ _ - _ _ _ _ - _ _ - - - - _ _ - - - - _ _ - - - - - _ _ _ _ _ - - - - - - - - - - - - - - - - - - - - - - - - - - . u.S. NUCLEAR REGULATORY Commission g g MATERIALS LICENSE Pursuant to the Atomic Energy Act of 1954, as amended, the Energy Reorganization Act of 1974 (Public Law 93-438), and Title 10 Code of Fed:ral Regulations, Chapter I, Parts 30,31,32,33,34,35,36,39,40, and 70, and in reliance on statements and representations heretofore made by the licensee, a license is hereby issued authorizing the licensee to receive, acquire, possess, and transfer byproduct, source, and special nuclear material designated below; to use such material for the purpose (s) and at the place (s) designated below; to deliver or transfer such material to persons authorized to receive it in accordance with the regulations of the applicable Part(s). This license , sh:ll be deemed to contain the conditions specified in Section 183 of the Atomic Energy Act of 1954, as amended, and is subject to all I applicable rules, regulations, and orders of the Nuclear Regulatory Commission now or hereafter in effect and to any conditions specif'e d c. Ucensee In accordance with the letter dated May 19,1998, and fax transmittal dated June 2,1998 1. St. Joseph's Community Hospital 3. Ucense number 48-16117-01 is amended in of West Bend, Inc. Its entirety as follows: 2. 551 S. Silverbrook Drive g R le. gpiration date January 31,2002 W st Bend, WI 53095 Y- b 5.