Patterns, Variants, Artifacts & Pitfalls in Conventional Radionuclide Bone
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nuclide Imaging: Planar Scintigraphy, SPECT, PET
Nuclide Imaging: Planar Scintigraphy, SPECT, PET Yao Wang Polytechnic University, Brooklyn, NY 11201 Based on J. L. Prince and J. M. Links, Medical Imaging Signals and Systems, and lecture notes by Prince. Figures are from the textbook except otherwise noted. Lecture Outline • Nuclide Imaging Overview • Review of Radioactive Decay • Planar Scintigraphy – Scintillation camera – Imaging equation • Single Photon Emission Computed Tomography (SPECT) • Positron Emission Tomography (PET) • Image Quality consideration – Resolution, noise, SNR, blurring EL5823 Nuclear Imaging Yao Wang, Polytechnic U., Brooklyn 2 What is Nuclear Medicine • Also known as nuclide imaging • Introduce radioactive substance into body • Allow for distribution and uptake/metabolism of compound ⇒ Functional Imaging ! • Detect regional variations of radioactivity as indication of presence or absence of specific physiologic function • Detection by “gamma camera” or detector array • (Image reconstruction) From H. Graber, Lecture Note for BMI1, F05 EL5823 Nuclear Imaging Yao Wang, Polytechnic U., Brooklyn 3 Examples: PET vs. CT • X-ray projection and tomography: – X-ray transmitted through a body from a outside source to a detector (transmission imaging) – Measuring anatomic structure • Nuclear medicine: – Gamma rays emitted from within a body (emission imaging) From H. Graber, Lecture Note, F05 – Imaging of functional or metabolic contrasts (not anatomic) • Brain perfusion, function • Myocardial perfusion • Tumor detection (metastases) EL5823 Nuclear Imaging Yao Wang, Polytechnic -

Description of Alternative Approaches to Measure and Place a Value on Hospital Products in Seven Oecd Countries
OECD Health Working Papers No. 56 Description of Alternative Approaches to Measure Luca Lorenzoni, and Place a Value Mark Pearson on Hospital Products in Seven OECD Countries https://dx.doi.org/10.1787/5kgdt91bpq24-en Unclassified DELSA/HEA/WD/HWP(2011)2 Organisation de Coopération et de Développement Économiques Organisation for Economic Co-operation and Development 14-Apr-2011 ___________________________________________________________________________________________ _____________ English text only DIRECTORATE FOR EMPLOYMENT, LABOUR AND SOCIAL AFFAIRS HEALTH COMMITTEE Unclassified DELSA/HEA/WD/HWP(2011)2 Health Working Papers OECD HEALTH WORKING PAPERS NO. 56 DESCRIPTION OF ALTERNATIVE APPROACHES TO MEASURE AND PLACE A VALUE ON HOSPITAL PRODUCTS IN SEVEN OECD COUNTRIES Luca Lorenzoni and Mark Pearson JEL Classification: H51, I12, and I19 English text only JT03300281 Document complet disponible sur OLIS dans son format d'origine Complete document available on OLIS in its original format DELSA/HEA/WD/HWP(2011)2 DIRECTORATE FOR EMPLOYMENT, LABOUR AND SOCIAL AFFAIRS www.oecd.org/els OECD HEALTH WORKING PAPERS http://www.oecd.org/els/health/workingpapers This series is designed to make available to a wider readership health studies prepared for use within the OECD. Authorship is usually collective, but principal writers are named. The papers are generally available only in their original language – English or French – with a summary in the other. Comment on the series is welcome, and should be sent to the Directorate for Employment, Labour and Social Affairs, 2, rue André-Pascal, 75775 PARIS CEDEX 16, France. The opinions expressed and arguments employed here are the responsibility of the author(s) and do not necessarily reflect those of the OECD. -

National Imaging Associates, Inc. Clinical Guidelines FACET JOINT
National Imaging Associates, Inc. Clinical guidelines Original Date: July 1, 2015 FACET JOINT INJECTIONS OR BLOCKS Page 1 of 4 “FOR FLORIDA BLUE MEMBERS ONLY” CPT Codes: Last Review Date: May 28, 2015 Cervical/Thoracic Region: 64490 (+ 64491, +64492) Lumbar/Sacral Region: 64493 (+64494, +64495) Medical Coverage Guideline Number: Last Revised Date: 02-61000-30 Responsible Department: Implementation Date: July 2015 Clinical Operations “FOR FLORIDA BLUE MEMBERS ONLY” INTRODUCTION Facet joints (also called zygapophysial joints or z-joints), are posterior to the vertebral bodies in the spinal column and connect the vertebral bodies to each other. They are located at the junction of the inferior articular process of a more cephalad vertebra, and the superior articular process of a more caudal vertebra. These joints provide stability and enable movement, allowing the spine to bend, twist, and extend in different directions. They also restrict hyperextension and hyperflexion. Facet joints are clinically important spinal pain generators in those with chronic spinal pain. Facet joints may refer pain to adjacent structures, making the underlying diagnosis difficult, as referred pain may assume a pseudoradicular pattern. Lumbar facet joints may refer pain to the back, buttocks, and lower extremities while cervical facet joints may refer pain to the head, neck and shoulders. Imaging findings are of little value in determining the source and location of ‘facet joint syndrome’, a term referring to back pain caused by pathology at the facet joints. Imaging studies may detect changes in facet joint architecture, but correlation between radiologic findings and symptoms is unreliable. Although clinical signs are also unsuitable for diagnosing facet joint-mediated pain, they may be of value in selecting candidates for controlled local anesthetic blocks of either the medial branches or the facet joint itself. -

The Erector Spinae Plane Block a Novel Analgesic Technique in Thoracic Neuropathic Pain
CHRONIC AND INTERVENTIONAL PAIN BRIEF TECHNICAL REPORT The Erector Spinae Plane Block A Novel Analgesic Technique in Thoracic Neuropathic Pain Mauricio Forero, MD, FIPP,*Sanjib D. Adhikary, MD,† Hector Lopez, MD,‡ Calvin Tsui, BMSc,§ and Ki Jinn Chin, MBBS (Hons), MMed, FRCPC|| Case 1 Abstract: Thoracic neuropathic pain is a debilitating condition that is often poorly responsive to oral and topical pharmacotherapy. The benefit A 67-year-old man, weight 116 kg and height 188 cm [body of interventional nerve block procedures is unclear due to a paucity of ev- mass index (BMI), 32.8 kg/m2] with a history of heavy smoking idence and the invasiveness of the described techniques. In this report, we and paroxysmal supraventricular tachycardia controlled on ateno- describe a novel interfascial plane block, the erector spinae plane (ESP) lol, was referred to the chronic pain clinic with a 4-month history block, and its successful application in 2 cases of severe neuropathic pain of severe left-sided chest pain. A magnetic resonance imaging (the first resulting from metastatic disease of the ribs, and the second from scan of his thorax at initial presentation had been reported as nor- malunion of multiple rib fractures). In both cases, the ESP block also pro- mal, and the working diagnosis at the time of referral was post- duced an extensive multidermatomal sensory block. Anatomical and radio- herpetic neuralgia. He reported constant burning and stabbing logical investigation in fresh cadavers indicates that its likely site of action neuropathic pain of 10/10 severity on the numerical rating score is at the dorsal and ventral rami of the thoracic spinal nerves. -

Pain Pattern Explanation Forms
Pain Pattern Explanation Forms 1. Cervical Facet Pain Pattern 2. Cervical Radicular/Dynatome Pain Pattern 3. Costotransverse Joint Pain Pattern 4. Fibromyalgia Points 5. Hip Joint Pain Pattern 6. Lumbar Dermatomes: Chemical Radiculitis 7. Lumbar Dermatomes: Disc Pathology 8. Lumbar Disc Pathology Healed 9. Lumbar Epidural Fibrosis 10. Lumbar Facet Pain Pattern 11. Lumbar Stenosis 12. Sacroiliac Joint Pain Pattern 13. Thoracic Facet Pain Pattern 14. Upper Cervical Joint Pain Pattern The OEA pain pattern handouts are PDF files that can be used for patient education and marketing. They help you explain your diagnosis with original illustrations that the patients can take home with them. There is limited text so you can tell your explanation of the treatment plan. The pain patterns can be printed in color or black and white. Once purchased, our business card will be replaced with yours to personalize each handout. Each illustration is based on the pain patterns that have been established in books or research articles when available. Normal anatomy and pathoanatomy illustrations are shown for the clinician to explain the diagnosis to the patient and how their treatment can influence the pain generator. These can also be utilized as marketing tools. The following pages are some guidelines that can be utilized to explain the handouts to patients. Cervical Facet Pain Pattern The cervical facet joints are the joints of the neck. Neurophysiologic studies have shown that cervical facet‐joint capsules are sources of neck pain.1 Dwyer et al.2 established pain patterns of the cervical facet joints. o Parasagittal cervical and cervicothoracic pain. -
Digital Motion X-Ray Cervical Spine
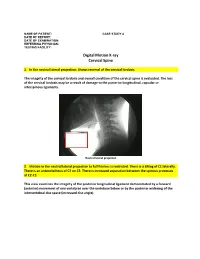
NAME OF PATIENT: CASE STUDY 4 DATE OF REPORT: DATE OF EXAMINATION: REFERRING PHYSICIAN: TESTING FACILITY: Digital Motion X-ray Cervical Spine 1. In the neutral lateral projection: Shows reversal of the cervical lordosis. The integrity of the cervical lordosis and overall condition of the cervical spine is evaluated. The loss of the cervical lordosis may be a result of damage to the posterior longitudinal, capsular or interspinous ligaments. Neutral lateral projection 2. Motion in the neutral lateral projection to full flexion: Is restricted. There is a tilting of C1 laterally. There is an anterolisthesis of C2 on C3. There is increased separation between the spinous processes at C2-C3. This view examines the integrity of the posterior longitudinal ligament demonstrated by a forward (anterior) movement of one vertebrae over the vertebrae below or by the posterior widening of the intervertebral disc space (increased disc angle). Widening of posterior disc space Anterolisthesis The integrity of the interspinous ligament is evaluated in the lateral flexion view. Damage to this ligament results in increased separation of the spinous processes in flexion. Damaged Interspinous Ligament Full flexion projection 3. Motion in the neutral lateral projection to full extension: Is restricted. There is a retrolisthesis of C4 on C5. This view examines the integrity of the anterior longitudinal ligament demonstrated by a backward (posterior) movement of one vertebrae over the vertebrae below or by the anterior widening of the intervertebral disc space (increased disc angle). Retrolisthesis Widening of the anterior disc Full Extension 4. Motion in the oblique flexion projection: Is restricted. There is gapping of the facet joints at C6-C7 bilaterally and C7-T1 bilaterally. -
Quantitative Bone Scintigraphy. a Study in Patients with Prostatic Carcinoma
i Quantitative Bone Scintigraphy A study in patients with prostatic carcinoma Gunilla Sundkvist \OO -II , Malmö 1991 Organization Document name LUND UNIVERSITY DOCTORAL DISSERTATION Department of Clinical Physiology Date of issue Malmö Allmänna Sjukhus 1991-05-08 S-214 01 Malmö, Sweden CODEN: LUMEDW-f.MEFM-lOlOU-lOO (1991) Authors) Sponsoring organization Gunilla Sundkvist Title and subtitle Quantitative Bone Scintigraphy. A study in patients with prostatic carcinoma. Abstract Quantitative bone scintigraphy was performed in patients with prostatic carcinoma before orchiectomy as well as two weeks, two and six months after operation. The count rate was recorded as serial gamma camera images over the lower thoracic and all lumbar vertebrae from 1 to 240 min and at 24 h after injection of "Tcm-MDP. In almost all abnormal vertebrae an increased count rate was observed within one hour after injection. Most of the vertebrae which were considered normal at 4 h after injection, but had an increased 24 h/4 h ratio developed into abnormal vertebrae later in the study. The patients with normal bone scintigrams showed no change in "Tcm- MDP uptake during the study. The reproducibility of quantitative bone scintigraphy was found to be ± 7% (1 SD). In response to therapy, most of the patients with abnormal bone scintigrams showed an increase in count rate two weeks after operation followed by a decrease to the pre-operative level after two months and a o further decrease after six months. This so called "flare phenomenon" was found to m ta indicate "Tc -MDP in the vascular phase as well as an active bone uptake. -

Relationship Between Endplate Defects, Modic Change, Facet Joint Degeneration, and Disc Degeneration of Cervical Spine
Neurospine 2020;17(2):443-452. Neurospine https://doi.org/10.14245/ns.2040076.038 pISSN 2586-6583 eISSN 2586-6591 Original Article Relationship Between Endplate Corresponding Author Defects, Modic Change, Facet Joint Dong Wuk Son https://orcid.org/0000-0002-9154-1923 Degeneration, and Disc Degeneration Department of Neurosurgery, Pusan of Cervical Spine National University Yangsan Hospital, 20 Geumo-ro, Mulgeum-eup, Yangsan 50612, Su-Hun Lee1,2, Dong Wuk Son1,2, Jun-Seok Lee1,2, Soon-Ki Sung1,2, Sang Weon Lee1,2, Korea Geun Sung Song1,2 E-mail: [email protected] 1Department of Neurosurgery, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea Received: February 11, 2020 2Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Revised: February 26, 2020 Hospital, Yangsan, Korea Accepted: February 27, 2020 Objective: The ‘‘disc degeneration precedes facet joint osteoarthritis’’ hypothesis and multi- dimensional analysis were actively discussed in lumbar spine. However, in cervical spine degeneration, the multifactorial analyzes of disc degeneration (DD), Modic changes (Mcs), facet degeneration, and endplate degeneration (ED) is still limited. In this cross-sectional study, we aimed to analyze the prevalence and interrelationship of cervical DD parameters. Methods: We retrospectively recruited 62 patients aged between 60 and 70 years. The disc height, segmental angle, ossified posterior longitudinal ligament (OPLL), ED, facet joint degeneration -

Procedure Guideline for Planar Radionuclide Cardiac
Procedure Guideline for Planar Radionuclide Cardiac Ventriculogram for the Assessment of Left Ventricular Systolic Function Version 2 2016 Review date 2021 a b c d e e Alice Nicol , Mike Avison , Mark Harbinson , Steve Jeans , Wendy Waddington , Simon Woldman (on behalf of BNCS, BNMS, IPEM). a b Southern General Hospital, NHS Greater Glasgow & Clyde, Glasgow, UK Bradford Royal Infirmary, c d e Bradford, UK Queens University, Belfast, UK Christie Hospital NHS Foundation Trust, Manchester, UK University College London Hospitals NHS Foundation Trust, London, UK 1 1. Introduction The purpose of this guideline is to assist specialists in nuclear medicine in recommending, performing, interpreting and reporting radionuclide cardiac ventriculograms (RNVG), also commonly known as multiple gated acquisition (MUGA) scans. It will assist individual departments in the development and formulation of their own local protocols. RNVG is a reliable and robust method of assessing cardiac function [1-5]. The basis of the study is the acquisition of a nuclear medicine procedure with multiple frames, gated by the R wave of the electrocardiogram (ECG) signal. The tracer is a blood pool agent, usually red blood cells labelled with technetium-99m (99mTc). One aim of this guideline is to foster a more uniform method of performing RNVG scans throughout the United Kingdom. This is particularly desirable since the National Institute for Health and Clinical Excellence (NICE) has mandated national protocols for the pre-assessment and monitoring of patients undergoing certain chemotherapy regimes [6, 7], based on specific left ventricular ejection fraction (LVEF) criteria. This guideline will focus on planar equilibrium RNVG scans performed for the assessment of left ventricular systolic function at rest, using data acquired in the left anterior oblique (LAO) projection by means of a frame mode, ECG-gated acquisition method. -

Ossification of the Posterior Longitudinal Ligament: Pathogenesis, Management, and Current Surgical Approaches
Neurosurg Focus 30 (3):E10, 2011 Ossification of the posterior longitudinal ligament: pathogenesis, management, and current surgical approaches A review ZACHARY A. SMITH, M.D.,1 COLIN C. BUCHANAN, M.D.,2 DAN RAPHAEL, P.A.-C.,1 AND LARRY T. KHOO, M.D.1 1Division of Neurosurgery, The Spine Clinic of Los Angeles, Good Samaritan Hospital, An Affiliate Hospital of the University of Southern California Medical School; and 2Department of Neurosurgery, Ronald Reagan–UCLA Medical Center, David Geffen School of Medicine at UCLA, Los Angeles, California Ossification of the posterior longitudinal ligament (OPLL) is an important cause of cervical myelopathy that results from bony ossification of the cervical or thoracic posterior longitudinal ligament (PLL). It has been estimated that nearly 25% of patients with cervical myelopathy will have features of OPLL. Patients commonly present in their mid-40s or 50s with clinical evidence of myelopathy. On MR and CT imaging, this can be seen as areas of ossification that commonly coalesce behind the cervical vertebral bodies, leading to direct ventral compression of the cord. While MR imaging will commonly demonstrate associated changes in the soft tissue, CT scanning will better define areas of ossification. This can also provide the clinician with evidence of possible dural ossification. The surgical management of OPLL remains a challenge to spine surgeons. Surgical alternatives include anterior, posterior, or circumferential decompression and/or stabilization. Anterior cervical stabilization options include cervical corpectomy or multilevel anterior cervical corpectomy and fusion, while posterior stabilization approaches include instrumented or noninstru- mented fusion or laminoplasty. Each of these approaches has distinct advantages and disadvantages. -

Ganglion Cyst of the Posterior Longitudinal Ligament Causing Lumbar Radiculopathy: Case Report
Spinal Cord (1997) 35, 632 ± 635 1997 International Medical Society of Paraplegia All rights reserved 1362 ± 4393/97 $12.00 Ganglion cyst of the posterior longitudinal ligament causing lumbar radiculopathy: case report Hisatoshi Baba1, Nobuaki Furusawa1, Yasuhisa Maezawa1, Kenzo Uchida1, Yasuo Kokubo1, Shinichi Imura1 and Sakon Noriki2 1Department of Orthopaedic Surgery; 2The First Department of Pathology, Fukui Medical School, Shimoaizuki 23, Matsuoka, Fukui 910-11, Japan We describe a man aged 26 years who presented with a neurological syndrome, which was found on lumbar radioculopathy to be due to a ganglion cyst originating from the posterior longitudinal ligament. Based on MRI ®ndings, a cystic lesion was suspected, a round lesion at L4 level with no connection to the adjacent facet or to the dura matter. During surgery, a liquid-containing cystic lesion was found to originate from the posterior longitudinal ligament at L4 level. The resected cyst was diagnosed histologically as a ganglion cyst. A complete cure was established after surgery and no recurrence was noted at a follow-up 1.7 years postoperatively. A ganglion cyst of the posterior longitudinal ligament should be considered in the dierential diagnosis of a cyst in the lumbar region causing neurological complications. Keywords: lumbar spine; posterior longitudinal ligament; ganglion cyst; radiculopathy Introduction Cystic lesions within the lumbosacral spinal canal can L4 dermatome. Muscle strength of the quadriceps cause symptoms and signs such as radiculopathy. femoris, tibialis anterior, extensor hallucis longus, was These cysts include ganglion1±3 and synovial cysts.4±7 assessed as normal. The straight leg raising test was To our knowledge, no report has previously been positive on the right at 508 and the femoral nerve described of a ganglion cyst in the posterior long- stretch test was also positive. -

III.2. POSITRON EMISSION TOMOGRAPHY – a NEW TECHNOLOGY in the NUCLEAR MEDICINE IMAGE DIAGNOSTICS (Short Review)
III.2. POSITRON EMISSION TOMOGRAPHY – A NEW TECHNOLOGY IN THE NUCLEAR MEDICINE IMAGE DIAGNOSTICS (Short review) Piperkova E, Georgiev R Dept.of Nuclear Medicine and Dept of Radiotherapy, National Oncological Centre Hospital, Sofia Positron Emission Tomography (PET) is a technology which makes fast advance in the field of Nuclear Medicine. It is different from the X-ray Computed Tomography and Magnetic Resonance Imaging (MRI), where mostly anatomical structures are shown and their functioning could be evaluated only indirectly. In addition, PET can visualise the biological nature and metabolite activity of the cells and tissues. It also has the capability for quantitative determination of the biochemical, physiological and pathological process in the human body (1). The spatial resolution of PET is usually 4-5mm and when the concentration of the positron emitter in the cells is high enough, it allows to see small size pathological zones with high proliferative and metabolite activity ( 3, 7, 17). Following fast and continuous improvement, PET imaging systems have advanced from the Bismuth Germanate Oxide (BGO) circular detector technology to the modern Lutetium Orthosilicate (LSO) and Gadolinium Orthosilicate (GSO) detectors (2, 7, 16). On the other hand, the construction technology has undergone significant progress in the development of new combined PET-CT and PET-MRI systems which currently replace the conventional PET systems with integrated transmission and emission detecting procedures, shown in Fig. 1. Fig. 1 A modern PET-CT system with one gantry. The sensitivity and the accuracy of PET based methods are found to be considerably higher compared to the other existing imaging methods and they can achieve 90-100% in the localisation of different oncological lesions (4, 11, 13, 14).