Cameroon Brief
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Infrastructure Causes of Road Accidents on the Yaounde – Douala Highway, Cameroon
Available online at http://www.journalijdr.com International Journal of Development Research ISSN: 2230-9926 Vol. 10, Issue, 06, pp. 36260-36266, June, 2020 https://doi.org/10.37118/ijdr.18747.06.2020 RESEARCH ARTICLE OPEN ACCESS INFRASTRUCTURE CAUSES OF ROAD ACCIDENTS ON THE YAOUNDE – DOUALA HIGHWAY, CAMEROON 1WOUNBA Jean François, 2NKENG George ELAMBO and *3MADOM DE TAMO Morrelle 1Department of Town Planning, National Advanced School of Public Works Yaounde, Ministry of Public Works, P.O. Box 510, Yaounde, Cameroon; 2Director of the National Advanced School of Public Works Yaounde, Ministry of Public Works, P.O. Box 510, Yaounde, Cameroon: 3Department of Civil Engineering, National Advanced School of Public Works Yaounde, Ministry of Public Works, P.O. Box 510, Yaounde, Cameroon ARTICLE INFO ABSTRACT ArticleArticle History: History: The overall goal of this study was to determine the causes of road crashes related to road th ReceivedReceived 24xxxxxx, March, 2019 2020 infrastructure parameters on the National Road No. 3 (N3) and provide measures to improve the ReceivedReceived inin revisedrevised formform safety of all road users. To achieve this, 225 accident reports for the years 2017 and 2018 were th 19xxxxxxxx, April, 2020 2019 th collected from the State Defense Secretariat. This accident data was analyzed using the crash AcceptedAccepted 20xxxxxxxxx May, 2020, 20 19 frequency and the injury severity density criteria to obtain the accident-prone locations (7 critical Published online 25th June, 2020 Published online xxxxx, 2019 sections and 2 critical intersections) and a map presenting these locations produced with ArcGis Key Words: 10.4.1. A site visit of these locations was then performed to obtain the road infrastructure and environment data necessary to get which parameters are responsible for road crashes. -
Report of Fact-Finding Mission to Cameroon
Report of fact-finding mission to Cameroon Country Information and Policy Unit Immigration and Nationality Directorate Home Office United Kingdom 17 – 25 January 2004 TABLE OF CONTENTS 1. Preface 1.1 2. Background 2.1 3. Opposition Political Parties / Separatist 3.1. Movements Social Democratic Front (SDF) 3.2 Southern Cameroons National Council (SCNC) 3.6 Ambazonian Restoration Movement (ARM) 3.16 Southern Cameroons Youth League (SCYL) 3.17 4. Human Rights Groups and their Activities 4.1 The National Commission for Human Rights and Freedoms 4.5 (NCHRF) Action by Christians for the Abolition of Torture (ACAT) 4.10 Action des Chrétiens pour l’Abolition de la Torture ………… Nouveaux Droits de l’Homme (NDH) 4.12 Human Rights Defence Group (HRDG) 4.16 Collectif National Contre l’Impunite (CNI) 4.20 5. Bepanda 9 5.1 6. Prison Conditions 6.1 Bamenda Central Prison 6.17 New Bell Prison, Douala 6.27 7. People in Authority 7.1 Security Forces and the Police 7.1 Operational Command 7.8 Government Officials / Public Servants 7.9 Human Rights Training 7.10 8. Freedom of Expression and the Media 8.1 Journalists 8.4 Television and Radio 8.10 9. Women’s Issues 9.1 Education and Development 9.3 Female Genital Mutilation (FGM) 9.9 Prostitution / Commercial Sex Workers 9.13 Forced Marriages 9.16 Domestic Violence 9.17 10. Children’s Rights 10.1 Health 10.3 Education 10.7 Child Protection 10.11 11. People Trafficking 11.1 12. Homosexuals 12.1 13. Tribes and Chiefdoms 13.1 14. -

Evidence from Bamenda, Cameroon
sustainability Article Urban Expansion and the Dynamics of Farmers’ Livelihoods: Evidence from Bamenda, Cameroon Akhere Solange Gwan 1 and Jude Ndzifon Kimengsi 2,3,* 1 Department of Geography and Planning, The University of Bamenda, Bambili 00237, Cameroon; [email protected] 2 Faculty of Environmental Sciences, Technische Universität Dresden, 01737 Tharandt, Germany 3 Department of Geography, The University of Bamenda, Bambili 00237, Cameroon * Correspondence: [email protected] Received: 12 June 2020; Accepted: 14 July 2020; Published: 18 July 2020 Abstract: There is growing interest in the need to understand the link between urban expansion and farmers’ livelihoods in most parts of sub-Saharan Africa (SSA), including Cameroon. This paper undertakes a qualitative investigation of the effects of urban expansion on farmers’ livelihoods in Bamenda, a primate city in Cameroon. Taking into consideration two key areas—the Mankon–Bafut axis and the Nkwen Bambui axis—this study analyzes the trends and effects of urban expansion on farmers’ livelihoods with a view to identifying ways of making the process more beneficial to the farmers. Maps were used to determine the trend of urban expansion between 2000 and 2015. Twelve farmers drawn from the target sites were interviewed, while three focus group discussions were conducted. Thematic analysis was employed to analyze perceptions of the effects and coping strategies of farmers to urban expansion. Using the livelihoods approach, farmers’ livelihoods repertoires and portfolios were analyzed for the periods before and after urban expansion. Between 2000 and 2015, the surface area for farmlands in Bamenda II and Bamenda III reduced from 3540 ha to 2100 ha and 2943 ha to 1389 ha, respectively. -

Human Settlement Dynamics in the Bamenda III Municipality, North West Region, Cameroon
Centre for Research on Settlements and Urbanism Journal of Settlements and Spatial Planning J o u r n a l h o m e p a g e: http://jssp.reviste.ubbcluj.ro Human Settlement Dynamics in the Bamenda III Municipality, North West Region, Cameroon Lawrence Akei MBANGA 1 1 The University of Bamenda, Faculty of Arts, Department of Geography and Planning, Bamenda, CAMEROON E-mail: [email protected] DOI: 10.24193/JSSP.2018.1.05 https://doi.org/10.24193/JSSP.2018.1.05 K e y w o r d s: human settlements, dynamics, sustainability, Bamenda III, Cameroon A B S T R A C T Every human settlement, from its occupation by a pioneer population continues to undergo a process of dynamism which is the result of socio economic and dynamic factors operating at the local, national and global levels. The urban metabolism model shows clearly that human settlements are the quality outputs of the transformation of inputs by an urban area through a metabolic process. This study seeks to bring to focus the drivers of human settlement dynamics in Bamenda 3, the manifestation of the dynamics and the functional evolution. The study made used of secondary data and information from published and unpublished sources. Landsat images of 1989, 1999 and 2015 were used to analyze dynamics in human settlement. Field survey was carried out. The results show multiple drivers of human settlement dynamism associated with population growth. Human settlement dynamics from 1989, 1999 and 2015 show an evolution in surface area with that of other uses like agriculture reducing. -

Report on the IDB2014 Celebrations in Cameroon
CAMEROON CELEBRATION OF THE INTERNATIONAL DAY FOR BIODIVERSITY Yaounde, Cameroon 14 May 2014 THEME: ISLAND BIODIVERSITY REPORT A cross-section of the exhibition ground including school children and the media Yaounde, 15 May 2014 1 CITATION This document will be cited as MINEPDED 2014. Report on the Celebration of the 2014 International Day for Biodiversity in Cameroon ACKNOWLEDGEMENT The organisation of the 2014 Day for Biodiversity was carried out under the supervision of the Minister of Environment, Protection of Nature and Sustainable Development Mr HELE Pierre and the Minister Delegate Mr. NANA Aboubacar DJALLOH. The contributions of the Organising Committee were highly invaluable for the success of the celebration of the 2014 International Day for Biodiversity. Members were: AKWA Patrick- Secretary General of MINEPDED- Representative of the Minister at the celebration; GALEGA Prudence- National Focal Point for the Convention on Biological Diversity- coordinator of the celebration; WADOU Angele- Sub-Director of Biodiversity and Biosafety, MINEPDED; WAYANG Raphael- Chief of Service for Biodiversity, MINEPDED NFOR Lilian- Environmental Lawyer at the Service of the Technical Adviser No1 of MINEPDED; SHEI Wilson- Project Assistant, ABS; NDIFOR Roland -Representative of IUCN- Cameroon; BANSEKA Hycinth- Representative of Global Water Partnership- Cameroon MBE TAWE Alex- Representative of World Fish Centre- Cameroon 2 TABLE of CONTENT Introduction…………………………………………………………………………………....4 Preparatory activities………………………………………………………………………..5 Media activities………………………………………………………………………………….5 Commemoration of activities…………………………………………………………….6 Exhibition………………………………………………………………………………………....7 Presentation of stands……………………………………………………………………….7 Conclusion…………………………………………………………………………………………12 Photo gallery…………………………………………………………………………………….13 3 INTRODUCTION Cameroon as a member of the 1992 Convention on Biological Diversity joined the international community to celebrate the International Day for Biodiversity 2014 under the theme ‘Island Biodiversity”. -
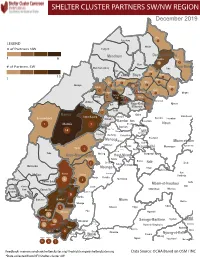
NW SW Presence Map Complete Copy
SHELTER CLUSTER PARTNERS SW/NWMap creation da tREGIONe: 06/12/2018 December 2019 Ako Furu-Awa 1 LEGEND Misaje # of Partners NW Fungom Menchum Donga-Mantung 1 6 Nkambe Nwa 3 1 Bum # of Partners SW Menchum-Valley Ndu Mayo-Banyo Wum Noni 1 Fundong Nkum 15 Boyo 1 1 Njinikom Kumbo Oku 1 Bafut 1 Belo Akwaya 1 3 1 Njikwa Bui Mbven 1 2 Mezam 2 Jakiri Mbengwi Babessi 1 Magba Bamenda Tubah 2 2 Bamenda Ndop Momo 6b 3 4 2 3 Bangourain Widikum Ngie Bamenda Bali 1 Ngo-Ketunjia Njimom Balikumbat Batibo Santa 2 Manyu Galim Upper Bayang Babadjou Malentouen Eyumodjock Wabane Koutaba Foumban Bambo7 tos Kouoptamo 1 Mamfe 7 Lebialem M ouda Noun Batcham Bafoussam Alou Fongo-Tongo 2e 14 Nkong-Ni BafouMssamif 1eir Fontem Dschang Penka-Michel Bamendjou Poumougne Foumbot MenouaFokoué Mbam-et-Kim Baham Djebem Santchou Bandja Batié Massangam Ngambé-Tikar Nguti Koung-Khi 1 Banka Bangou Kekem Toko Kupe-Manenguba Melong Haut-Nkam Bangangté Bafang Bana Bangem Banwa Bazou Baré-Bakem Ndé 1 Bakou Deuk Mundemba Nord-Makombé Moungo Tonga Makénéné Konye Nkongsamba 1er Kon Ndian Tombel Yambetta Manjo Nlonako Isangele 5 1 Nkondjock Dikome Balue Bafia Kumba Mbam-et-Inoubou Kombo Loum Kiiki Kombo Itindi Ekondo Titi Ndikiniméki Nitoukou Abedimo Meme Njombé-Penja 9 Mombo Idabato Bamusso Kumba 1 Nkam Bokito Kumba Mbanga 1 Yabassi Yingui Ndom Mbonge Muyuka Fiko Ngambé 6 Nyanon Lekié West-Coast Sanaga-Maritime Monatélé 5 Fako Dibombari Douala 55 Buea 5e Massock-Songloulou Evodoula Tiko Nguibassal Limbe1 Douala 4e Edéa 2e Okola Limbe 2 6 Douala Dibamba Limbe 3 Douala 6e Wou3rei Pouma Nyong-et-Kellé Douala 6e Dibang Limbe 1 Limbe 2 Limbe 3 Dizangué Ngwei Ngog-Mapubi Matomb Lobo 13 54 1 Feedback: [email protected]/ [email protected] Data Source: OCHA Based on OSM / INC *Data collected from NFI/Shelter cluster 4W. -

Land Use and Land Cover Changes in the Centre Region of Cameroon
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 18 February 2020 Land Use and Land Cover changes in the Centre Region of Cameroon Tchindjang Mesmin; Saha Frédéric, Voundi Eric, Mbevo Fendoung Philippes, Ngo Makak Rose, Issan Ismaël and Tchoumbou Frédéric Sédric * Correspondence: Tchindjang Mesmin, Lecturer, University of Yaoundé 1 and scientific Coordinator of Global Mapping and Environmental Monitoring [email protected] Saha Frédéric, PhD student of the University of Yaoundé 1 and project manager of Global Mapping and Environmental Monitoring [email protected] Voundi Eric, PhD student of the University of Yaoundé 1 and technical manager of Global Mapping and Environmental Monitoring [email protected] Mbevo Fendoung Philippes PhD student of the University of Yaoundé 1 and internship at University of Liège Belgium; [email protected] Ngo Makak Rose, MSC, GIS and remote sensing specialist at Global Mapping and Environmental Monitoring; [email protected] Issan Ismaël, MSC and GIS specialist, [email protected] Tchoumbou Kemeni Frédéric Sédric MSC, database specialist, [email protected] Abstract: Cameroon territory is experiencing significant land use and land cover (LULC) changes since its independence in 1960. But the main relevant impacts are recorded since 1990 due to intensification of agricultural activities and urbanization. LULC effects and dynamics vary from one region to another according to the type of vegetation cover and activities. Using remote sensing, GIS and subsidiary data, this paper attempted to model the land use and land cover (LULC) change in the Centre Region of Cameroon that host Yaoundé metropolis. The rapid expansion of the city of Yaoundé drives to the land conversion with farmland intensification and forest depletion accelerating the rate at which land use and land cover (LULC) transformations take place. -

The Anglophone Crisis in Cameroon: a Geopolitical Analysis
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by European Scientific Journal (European Scientific Institute) European Scientific Journal December 2019 edition Vol.15, No.35 ISSN: 1857 – 7881 (Print) e - ISSN 1857- 7431 The Anglophone Crisis in Cameroon: A Geopolitical Analysis Ekah Robert Ekah, Department of 'Cultural Diversity, Peace and International Cooperation' at the International Relations Institute of Cameroon (IRIC) Doi:10.19044/esj.2019.v15n35p141 URL:http://dx.doi.org/10.19044/esj.2019.v15n35p141 Abstract Anglophone Cameroon is the present-day North West and South West (English Speaking) regions of Cameroon herein referred to as No-So. These regions of Cameroon have been restive since 2016 in what is popularly referred to as the Anglophone crisis. The crisis has been transformed to a separatist movement, with some Anglophones clamoring for an independent No-So, re-baptized as “Ambazonia”. The purpose of the study is to illuminate the geopolitical perspective of the conflict which has been evaded by many scholars. Most scholarly write-ups have rather focused on the causes, course, consequences and international interventions in the crisis, with little attention to the geopolitical undertones. In terms of methodology, the paper makes use of qualitative data analysis. Unlike previous research works that link the unfolding of the crisis to Anglophone marginalization, historical and cultural difference, the findings from this paper reveals that the strategic location of No-So, the presence of resources, demographic considerations and other geopolitical parameters are proving to be responsible for the heightening of the Anglophone crisis in Cameroon and in favour of the quest for an independent Ambazonia. -

Li.I I:L Li.I Li.I
• zI- LI.I ~ I:L 9 LI.I >LI.I Q EUROPEAN COMMISSION DE 90 . February , 1997 _1&tl~~2~. The Cameroonian Economy II Cameroon in Figures II er.BIl1!lmr'qlt~_e.~t§'~~g~i'§j"~]fgm From the Treaty of Rome to the Lome Convention Lome IV IJ Lome IV II The Institutions of the European Union .• The Instruments of Cooperation II The European Development Fund II ACP States and the European Union Il!J ~A_~~~11l~Ei9.~M~r~ Trade Relations m Bilateral Cooperation with the Member States lEI Commuriications Infrastructure lEI Road Maintenance Programme II Social Services II Health Education ~~/¥W#@Muar~~ .1!i9Jjt~J!}.Bti~.!t~~~m A NewPolicy II] The EC's Contribution to Privatization 1m Restructuring the Coffee and Cocoa Sectors Em AgricLiltlir~ m .. .... ,'. R~raldevEiJoPrT1e~(m, RJraioevelopment CentreProjed ,North-East Benoue Prbj~ct . .. ...•. .• '.. '" .• ' .•. .....STABEX TheCRBP and SupportforAgronOmy Research it) Central Africa ~fiiG~_~QR~.rx~~ EnVironment and Biodivd~Sity '1:9!1. O'therAid ~ Aid to Non"Governmental OrMnizations RegionalJ:ooperation' m MiJin Community Projects in Cameroon With map' Em CommunitY Operations in Cameroon 1960-95 1m Cover: Infrastructure. medical research and cattle breeding are all areas facing difficult challenges iri.the changing economic environm~~t. (REAphoto + Commission Delegation - Yaoynde) Introduction ooperation between Europe and Cameroon, \vhich was first established in 1958, has always been carefully Cattuned to Cameroon's development priorities. Traditional technical and financial cooperation under the Conventions between the African, Caribbean and Pacific States and the European Community, the first of which, Yaounde I, was signed in the Cameroonian capital in 1963, has gone hand in-hand with an expansion in trade between the t\VO sides. -

African Development Bank Group
AFRICAN DEVELOPMENT BANK GROUP PROJECT : TRANSPORT SECTOR SUPPORT PROGRAMME PHASE 2 : REHABILITATION OF YAOUNDE-BAFOUSSAM- BAMENDA ROAD – DEVELOPMENT OF THE GRAND ZAMBI-KRIBI ROAD – DEVELOPMENT OF THE MAROUA-BOGO-POUSS ROAD COUNTRY : REPUBLIC OF CAMEROON SUMMARY FULL RESETTLEMENT PLAN (FRP) Team Leader J. K. NGUESSAN, Chief Transport Engineer OITC.1 P. MEGNE, Transport Economist OITC.1 P.H. SANON, Socio-Economist ONEC.3 M. KINANE, Environmentalist ONEC.3 S. MBA, Senior Transport Engineer OITC.1 T. DIALLO, Financial Management Expert ORPF.2 C. DJEUFO, Procurement Specialist ORPF.1 Appraisal Team O. Cheick SID, Consultant OITC.1 Sector Director A. OUMAROU OITC Regional Director M. KANGA ORCE Resident CMFO R. KANE Representative Sector Division OITC.1 J.K. KABANGUKA Manager 1 Project Name : Transport Sector Support Programme Phase 2 SAP Code: P-CM-DB0-015 Country : Cameroon Department : OITC Division : OITC-1 1. INTRODUCTION This document is a summary of the Abbreviated Resettlement Plan (ARP) of the Transport Sector Support Programme Phase 2. The ARP was prepared in accordance with AfDB requirements as the project will affect less than 200 people. It is an annex to the Yaounde- Bafoussam-Babadjou road section ESIA summary which was prepared in accordance with AfDB’s and Cameroon’s environmental and social assessment guidelines and procedures for Category 1 projects. 2. PROJECT DESCRIPTION, LOCATION AND IMPACT AREA 2.1.1 Location The Yaounde-Bafoussam-Bamenda road covers National Road 4 (RN4) and sections of National Road 1 (RN1) and National Road 6 (RN6) (Figure 1). The section to be rehabilitated is 238 kilometres long. Figure 1: Project Location Source: NCP (2015) 2 2.2 Project Description and Rationale The Yaounde-Bafoussam-Bamenda (RN1-RN4-RN6) road, which was commissioned in the 1980s, is in an advanced state of degradation (except for a few recently paved sections between Yaounde and Ebebda, Tonga and Banganté and Bafoussam-Mbouda-Babadjou). -

Wetlands Exploitation Along the Bafoussam – Bamenda Road Axis of the Western Highlands of Cameroon
© Kamla-Raj 2013 J Hum Ecol, 41(1): 25-32 (2013) Wetlands Exploitation along the Bafoussam – Bamenda Road Axis of the Western Highlands of Cameroon Sunday Shende Kometa Department of Geography, Faculty of Social and Management Sciences, University of Buea, P.O. Box 63, Buea, Cameroon E-mail: [email protected] KEYWORDS Wetland. Exploitation. Environmental Consequences. Economic Benefit ABSTRACT This paper is focused on how wetlands have been exploited for economic and environmental reasons and some resultant environmental consequences. The rapid colonization of these wet areas is the result of an ever rising density of population and continuous cultivation throughout the year. Since water is essential for plant and animal life, it is important to figure out the possibilities of regulating population pressure and wetland utilization since the water table in these wetlands and the surrounding areas within this region falls drastically in the dry season. The study utilized field surveys and measurements, interviews, questionnaires and secondary sources, data was generated and analyzed on the exploitation of these ecological niches. For the short term economic benefits, the exploitation of these areas is good but the environmental and hydrological implications in the long run are likely be disastrous. An alternative landuse for this area has to be adopted in order to maintain sustainably the importance of these wetlands ecosystem. The application of chemical fertilizers should be regulated as they contaminate and eventually pollute water bodies with increasing aspects of poor water quality in the area. INTRODUCTION The value of a wetland is an estimate, usual- Wetlands are specific ecosystems like bogs, ly subjective of the worth, merit, quality or im- bottomlands, fens, flood plains, mangroves, portance of a particular ecosystem (Mays 1996). -

Cameroon Page 1 of 19
Cameroon Page 1 of 19 Cameroon Country Reports on Human Rights Practices - 2004 Released by the Bureau of Democracy, Human Rights, and Labor February 28, 2005 Cameroon is a republic dominated by a strong presidency. Despite the country's multiparty system of government, the Cameroon People's Democratic Movement (CPDM) has remained in power since the early years of independence. In October, CPDM leader Paul Biya won re-election as President. The primary opposition parties fielded candidates; however, the election was flawed by irregularities, particularly in the voter registration process. The President retains the power to control legislation or to rule by decree. He has used his legislative control to change the Constitution and extend the term lengths of the presidency. The judiciary was subject to significant executive influence and suffered from corruption and inefficiency. The national police (DGSN), the National Intelligence Service (DGRE), the Gendarmerie, the Ministry of Territorial Administration, Military Security, the army, the civilian Minister of Defense, the civilian head of police, and, to a lesser extent, the Presidential Guard are responsible for internal security; the DGSN and Gendarmerie have primary responsibility for law enforcement. The Ministry of Defense, including the Gendarmerie, DGSN, and DRGE, are under an office of the Presidency, resulting in strong presidential control of internal security forces. Although civilian authorities generally maintained effective control of the security forces, there were frequent instances in which elements of the security forces acted independently of government authority. Members of the security forces continued to commit numerous serious human rights abuses. The majority of the population of approximately 16.3 million resided in rural areas; agriculture accounted for 24 percent of gross domestic product.