A Case of Pulmonary MALT Lymphoma Arising From
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Ocular HIV/AIDS Related Diseases (Initial and Follow-Up Evaluation)
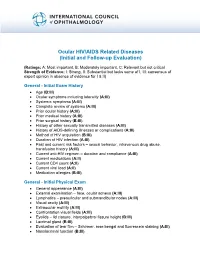
Ocular HIV/AIDS Related Diseases (Initial and Follow-up Evaluation) (Ratings: A: Most important, B: Moderately important, C: Relevant but not critical Strength of Evidence: I: Strong, II: Substantial but lacks some of I, III: consensus of expert opinion in absence of evidence for I & II) General - Initial Exam History Age (B:III) Ocular symptoms including laterality (A:III) Systemic symptoms (A:III) Complete review of systems (A:III) Prior ocular history (A:III) Prior medical history (A:III) Prior surgical history (B:III) History of other sexually transmitted diseases (A:III) History of AIDS-defining illnesses or complications (A:III) Method of HIV acquisition (B:III) Duration of HIV infection (A:III) Past and current risk factors – sexual behavior, intravenous drug abuse, transfusion history (A:III) Current anti-HIV regimen – duration and compliance (A:III) Current medications (A:II) Current CD4 count (A:II) Current viral load (A:II) Medication allergies (B:III) General - Initial Physical Exam General appearance (A:III) External examination – face, ocular adnexa (A:III) Lymphatics – preauricular and submandibular nodes (A:III) Visual acuity (A:III) Extraocular motility (A:III) Confrontation visual fields (A:III) Eyelids – lid closure, interpalpebral fissure height (B:III) Lacrimal gland (B:III) Evaluation of tear film – Schirmer, rose bengal and fluorescein staining (A:III) Nasolacrimal function (B:III) Slit-lamp examination o Eyelid margins (A:III) o Conjunctiva (A:III) o Sclera (A:III) o Cornea (A:III) o -

Immunoglobulin and T Cell Receptor Genes: IMGT(®) and the Birth and Rise of Immunoinformatics Marie-Paule Lefranc
Immunoglobulin and T Cell Receptor Genes: IMGT(®) and the Birth and Rise of Immunoinformatics Marie-Paule Lefranc To cite this version: Marie-Paule Lefranc. Immunoglobulin and T Cell Receptor Genes: IMGT(®) and the Birth and Rise of Immunoinformatics. Frontiers in Immunology, Frontiers, 2014, 5, pp.22. 10.3389/fimmu.2014.00022. hal-00957520 HAL Id: hal-00957520 https://hal.archives-ouvertes.fr/hal-00957520 Submitted on 28 May 2021 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Distributed under a Creative Commons Attribution| 4.0 International License CLASSIFICATION ARTICLE published: 05 February 2014 doi: 10.3389/fimmu.2014.00022 Immunoglobulin and T cell receptor genes: IMGT® and the birth and rise of immunoinformatics Marie-Paule Lefranc* The International ImMunoGenetics Information System® (IMGT®), Laboratoire d’ImmunoGénétique Moléculaire (LIGM), Institut de Génétique Humaine, UPR CNRS, Université Montpellier 2, Montpellier, France Edited by: IMGT®, the international ImMunoGeneTics information system®1, (CNRS and Université Kendall A. Smith, Weill Cornell Montpellier 2) is the global reference in immunogenetics and immunoinformatics. By its Medical College of Cornell University, ® USA creation in 1989, IMGT marked the advent of immunoinformatics, which emerged at ® Reviewed by: the interface between immunogenetics and bioinformatics. -

Immunoglobulin and T Cell Receptor Genes: IMGT and the Birth and Rise
CLASSIFICATION ARTICLE published: 05 February 2014 doi: 10.3389/fimmu.2014.00022 Immunoglobulin and T cell receptor genes: IMGT® and the birth and rise of immunoinformatics Marie-Paule Lefranc* The International ImMunoGenetics Information System® (IMGT®), Laboratoire d’ImmunoGénétique Moléculaire (LIGM), Institut de Génétique Humaine, UPR CNRS, Université Montpellier 2, Montpellier, France Edited by: IMGT®, the international ImMunoGeneTics information system®1, (CNRS and Université Kendall A. Smith, Weill Cornell Montpellier 2) is the global reference in immunogenetics and immunoinformatics. By its Medical College of Cornell University, ® USA creation in 1989, IMGT marked the advent of immunoinformatics, which emerged at ® Reviewed by: the interface between immunogenetics and bioinformatics. IMGT is specialized in the Edward J. Collins, University of North immunoglobulins (IG) or antibodies, T cell receptors (TR), major histocompatibility (MH), Carolina at Chapel Hill, USA and proteins of the IgSF and MhSF superfamilies. IMGT® has been built on the IMGT- David K. Cole, Cardiff University, UK ONTOLOGY axioms and concepts, which bridged the gap between genes, sequences, and *Correspondence: three-dimensional (3D) structures.The concepts include the IMGT® standardized keywords Marie-Paule Lefranc, The International ® ® ImMunoGenetics Information (concepts of identification), IMGT standardized labels (concepts of description), IMGT System® (IMGT®), Laboratoire standardized nomenclature (concepts of classification), IMGT unique numbering, and -

Genomic Analysis Offers Insights Into the Evolution of the Bovine TRA/TRD Locus', BMC Genomics, Vol
Edinburgh Research Explorer Genomic analysis offers insights into the evolution of the bovine TRA/TRD locus Citation for published version: Connelley, TK, Degnan, K, Longhi, CW & Morrison, WI 2014, 'Genomic analysis offers insights into the evolution of the bovine TRA/TRD locus', BMC Genomics, vol. 15, no. 1, 994. https://doi.org/10.1186/1471- 2164-15-994 Digital Object Identifier (DOI): 10.1186/1471-2164-15-994 Link: Link to publication record in Edinburgh Research Explorer Document Version: Publisher's PDF, also known as Version of record Published In: BMC Genomics Publisher Rights Statement: © 2014 Connelley et al.; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated. General rights Copyright for the publications made accessible via the Edinburgh Research Explorer is retained by the author(s) and / or other copyright owners and it is a condition of accessing these publications that users recognise and abide by the legal requirements associated with these rights. Take down policy The University of Edinburgh has made every reasonable effort to ensure that Edinburgh Research Explorer content complies with UK legislation. If you believe that the public display of this file breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. -

Next Generation Sequencing Reveals Changes of the Γδ T Cell Receptor
www.nature.com/scientificreports Correction: Author Correction OPEN Next generation sequencing reveals changes of the γδ T cell receptor repertoires in patients Received: 24 November 2017 Accepted: 14 February 2018 with pulmonary tuberculosis Published online: 02 March 2018 Chaofei Cheng1, Bei Wang1,2, Lei Gao1, Jianmin Liu4, Xinchun Chen5, He Huang1,2 & Zhendong Zhao1,2,3 Tuberculosis (TB) is a severe global threat to human health. The immune protection initiated by γδ T cells play an important role in mycobacterial infection. Vaccines for Mycobacterium tuberculosis (Mtb) based on γδ T cells provide a novel approach for TB control. In our previous studies, we found a preponderant complementarity-determining region 3 (CDR3) sequence of the γδ T cell receptor (TCR) in TB patients, and successfully identifed a tuberculosis antigen that can efectively activate γδ T cells with a reverse genetic strategy. However, due to the throughput limitation of the method we used, the information we obtained about the γδ TCR repertoire and preponderant CDR3 sequences was limited. In this study, we introduced next generation sequencing (NGS) to study the γδ TCR CDR3 repertoires in TB patients. We found that the CDR3δ tended to be more polyclonal and CDR3γ tended to be longer in TB patients; the γδ T cells expressing CDR3 sequences using a Vγ9-JγP rearrangement expanded signifcantly during Mtb infection. We also identifed new preponderant CDR3 sequences during Mtb infection. This study comprehensively characterized the γδ T cell receptor repertoire changes, and provides useful information for the development of new vaccines and adjuvants against TB. Tuberculosis (TB) caused by Mycobacterium tuberculosis (Mtb), the top infectious disease killer worldwide, remains a severe global threat to human health. -

Download Slides
PEARLS OF LABORATORY MEDICINE Pearl Title: Immunoglobulin and T Cell Receptor Genetics Name of Presenter: Bing Melody Zhang Affiliation: Stanford University School of Medicine DOI: 10.15428/CCTC.2020.318055 © Clinical Chemistry Outline • Structure of Immunoglobulin (Ig) and TCR (T cell receptor) • TCR/Ig genetics • T/B cell development and TCR/Ig gene rearrangement • Molecular testing of TCR/Ig rearrangement • Clinical utility of molecular TCR/Ig rearrangement analysis in lymphoid malignancies 2 Immunoglobulin (Ig) and T Cell Receptor (TCR) 3 TCR/Ig Genetics • Each receptor chain is encoded in the germline genome as different gene segments (V, D, J). • During T/B lymphocyte development, the gene segments undergo random somatic DNA recombination (VDJ or VJ) to form a complete variable region sequence, known as gene rearrangement. • Non-templated insertion and deletion of random nucleotides at the junctional regions. • Somatic hypermutation: high rate of point mutations in V region of Ig genes (mature B cells). 4 IGH Gene Rearrangement V genes D genes J genes Constant region Germline V-N-D-N-J 5 B cell development and BCR/Ig gene rearrangement Large pre- Small pre- Immature B Mature B Stem cells Early pro-B Late pro-B cell cell B cell B cell cell cell IgH: germline D-J joining V-DJ joining VDJ rearranged VDJ rearranged VDJ rearranged VDJ rearranged IgK/L: germline germline germline germline V-J joining VJ rearranged VJ rearranged Order of gene rearrangements: IGH → IGK If IGK rearrangement fails → IGL gene rearrangement The Immune System, -

Cracking the Carbohydrate Code for Selectin Recognition
CAROLYN R BERTOZZI CROSSTALK Cracking the carbohydrate code for selectin recognition Selectins are central in the inflammatory response; the discovery that they bind to carbohydrate ligands has galvanized carbohydrate chemists to search for inhibitors of the process. Recent progress in identifying and analyzing physiological selectin counter-receptors suggests new approaches to the design of ligands that bind to specific selectins. Chemistry & Biology November 1995, 2:703-708 White blood cells (leukocytes) circulate throughout the by designing specific antagonists, which may also serve as blood vasculature, patrolling the body for sites of tissue leads for therapeutics. damage or microbial infection. When such a site is encountered, the leukocytes must exit the blood stream Carbohydrate specificity of the selectins and migrate into the surrounding tissue to perform their The selectin family of adhesion molecules has three protective f&ctions. The sequence of events leading to members, E-, l’- and L-selectin (for a recent review see leukocyte recruitment, referred to as the inflammatory [a]). These share a common domain structure, which cascade, begins with the interaction of circulating leuko- includes an amino-terminal calcium-dependent (C-type) cytcs with endothelial cells lining the blood vessel (Fig. lectin domain, the sequence of which is highly conserved 1) [II. First, the leukocytes tether to and roll along the between family members, an epidermal growth factor endothelial layer, propelled by the force of the blood (EGF)-like domain, and a series of short consensus repeat flow.The leukocytes then firmly adhere to the endothe- sequences that are homologous to complement regulatory lial layer, and migrate between endothelial cells to com- proteins. -

Committed to Innovation and Growth
Committed to innovation and growth Alan Hippe, CFO Roche Group New York , February 2013 Roche strategy: Focused on medically differentiated therapies Regulators: Pharma Dia Optimised benefit / risk ratio Payors: Focus Optimised benefit / cost ratio MedTech Premium for innovation OTC Generics Differentiation 2 Roche: Operating profit and margin continuously increased Group core operating profit and margin 37.7% 34.9% 35.6% % of sales 33.0% 33.2% +11%1 17.16 16.27 16.59 15.07 15.15 CHF bn 2008 2009 2010 2011 2012 3 1 At CER=Constant Exchange Rates Roche: Cash flow and margin continuously increased Group operating free cash flow and margin % of sales 33.8% 32.1% 32.3% 29.8% 27.1% +10%1 15.7 15.4 14.1 13.7 12.4 CHF bn 2008 2009 2010 2011 2012 4 1 At CER=Constant Exchange Rates R&D productivity differs substantially among players Average annual 1 NME peak sales (2001-10) $ 710 m Peak Sales 4 x US$ bn (per $1 bn R&D) Roche $ 165 m Peak Sales (per $1 bn R&D) Average annual R&D investment (1997-2006)1 US$ bn 1 Peak sales and R&D calculated pro forma to account for major M&A 5 Source: EvaluatePharma; BCG analysis; Roche analysis Roche: R&D well balanced from a risk & disease point of view 2012 Roche budget Oncology Metabolism Inflammation CNS Virology 0% 5% 10% 15% 20% 25% 30% Industry average probability of success – Phase 0 to Registration 6 Source: Bernstein Equity Research, Tufts University and Roche analysis Changing the standard of care in HER2 Securing future growth by improving the standard of care Biosimilars launch (EU) 2nd line Xeloda -

Role of the Actin Cytoskeleton in Acinar Cell Protein Secretion
Role of the Actin Aytoskeleton in Acinar Cell Protein Secretion Robert C. De Lisle Anatomy and Cell Biology, University of Kansas School of Medicine, Kansas City, KS 66160 USA e-mail: [email protected] Version 2.0, November 9th, 2020 [DOI: 10.3998/panc.2020.07] Abstract different functions, as mutations in the two genes have very different effects (2). In the mouse acinar All eukaryotic cells, including the pancreatic acinar cell, Actb mRNA is expressed more than 2-fold cell, tightly control organization of their cytoplasm greater than Actg1 (Table 1); presumably their which in large part relies on the cytoskeleton. The protein levels match this expression although this cytoskeleton is comprised of three filament types: has not been measured in the pancreas. In gastric microtubules (tubulin), intermediate filaments parietal cells, β-actin is more localized to the apical (keratins), and microfilaments (actin). In addition to cortical cytoskeleton whereas γ-actin is more characteristics common to all cells, the pancreatic localized along the basolateral plasma membrane acinar cell is a polarized epithelial cell with a (BLPM) (47). If the same is true in the acinar cell, vectorial arrangement of the secretory machinery then β-actin is more likely to be important in protein and apically-directed protein secretion, with secretion which is also localized to the apical important roles of the cytoskeleton in this polarity. surface of the cell. In the acinar cell, γ-actin may be The most investigated of the cytoskeleton involved in the BLPM blebs that form under elements in the acinar cell are actin-based supraphysiologic stimulation. -

SUPPLEMENTAL FIGURE LEGEND Supplemental Figure 1. Representative HGA Histology of (A) Greater Than Median, and (B) Less Than
SUPPLEMENTAL FIGURE LEGEND Supplemental figure 1. Representative HGA histology of (A) greater than median, and (B) less than median tumor infiltration of helper T-cells (CD4; brown), (C) greater than median, and (D) less than median tumor infiltration of cytotoxic T-cells (CD8; red), (E) greater than 75th percentile, and (F) less than 75% percentile tumor infiltration of microglia/macrophages (AIF1; brown). Immunohistochemistry was performed using FFPE tumor sections and with hematoxylin counterstaining (400x magnification). Supplemental table IA. High grade astrocytoma long-term survivor patient details. Sample Survival Dead Age Karnofsky/ Dx detail location of Extent of Therapy received Used in ID (yrs) at Lansky tumor surgery microarray Dx performance study (yrs) score HGA1 17.0 N 34 100 AA pons biopsy radiation and BCNU HGA2 16.5 N 8 80 AA cerebrum GTR carboplatin, etoposide, CCNU, vincristine and radiation HGA3 16.0 N 47 90 GBM 1o cerebrum STR radiation and temozolmide HGA4 11.0 N 45 60 GBM, giant cell cerebrum GTR none HGA5 10.5 N 27 100 GBM 1o, cerebrum GTR radiation, CCNU, irinotecan, and temozolmide epithelioid HGA6 8.5 Y 21 100 RIG cerebellum STR radiation and temozolmide HGA7 8.5 N 2 80 GBM 1o thalamus/ STR cisplatin, vincristine, cytoxan, etoposide, carboplatin, cerebrum thiotepa HGA8 8.5 N 42 100 GBM 2o cerebrum GTR radiation, CCNU, irinotecan and temozolmide HGA9 8.5 N 46 80 GBM 1o cerebrum GTR radiation, CCNU, erlotinib and temozolmide yes HGA10 7.0 N 10 80 GBM 1o thalamus biopsy radiation and temozolmide HGA11 7.0 Y 24 -

Final Rule Is at 410–786–4142 Or Mitali Dayal Via Effective on January 1, 2020
61142 Federal Register / Vol. 84, No. 218 / Tuesday, November 12, 2019 / Rules and Regulations DEPARTMENT OF HEALTH AND DATES: via email [email protected] or HUMAN SERVICES Effective date: This final rule is at 410–786–4142 or Mitali Dayal via effective on January 1, 2020. email [email protected] or at Centers for Medicare & Medicaid Comment period: To be assured 410–786–4329. Services consideration, comments on the Ambulatory Surgical Center Quality payment classifications assigned to the Reporting (ASCQR) Program 42 CFR Parts 405, 410, 412, 414, 416, interim APC assignments and/or status Administration, Validation, and 419, and 486 indicators of new or replacement Level Reconsideration Issues, contact Anita II HCPCS codes in this final rule with [CMS–1717–FC] Bhatia via email Anita.Bhatia@ comment period must be received at one cms.hhs.gov or at 410–786–7236. RIN 0938–AT74 of the addresses provided in the Ambulatory Surgical Center Quality ADDRESSES section no later than 5 p.m. Reporting (ASCQR) Program Measures, Medicare Program: Changes to EST on December 2, 2019. contact Nicole Hewitt via email Hospital Outpatient Prospective ADDRESSES: In commenting, please refer [email protected] or at 410– Payment and Ambulatory Surgical to file code CMS–1717–FC when 786–7778. Center Payment Systems and Quality commenting on the issues in this final Blood and Blood Products, contact Reporting Programs; Revisions of rule with comment period. Because of Josh McFeeters via email Organ Procurement Organizations staff and resource limitations, we cannot [email protected] or at Conditions of Coverage; Prior accept comments by facsimile (FAX) 410–786–9732. -

Genomic and Expression Analyses of Tursiops Truncatus T Cell Receptor
Linguiti et al. BMC Genomics (2016) 17:634 DOI 10.1186/s12864-016-2841-9 RESEARCH ARTICLE Open Access Genomic and expression analyses of Tursiops truncatus T cell receptor gamma (TRG) and alpha/delta (TRA/TRD) loci reveal a similar basic public γδ repertoire in dolphin and human Giovanna Linguiti1†, Rachele Antonacci1†, Gianluca Tasco2, Francesco Grande3, Rita Casadio2, Serafina Massari4, Vito Castelli1, Arianna Consiglio5, Marie-Paule Lefranc6 and Salvatrice Ciccarese1* Abstract Background: The bottlenose dolphin (Tursiops truncatus) is a mammal that belongs to the Cetartiodactyla and have lived in marine ecosystems for nearly 60 millions years. Despite its popularity, our knowledge about its adaptive immunity and evolution is very limited. Furthermore, nothing is known about the genomics and evolution of dolphin antigen receptor immunity. Results: Here we report a evolutionary and expression study of Tursiops truncatus T cell receptor gamma (TRG) and alpha/delta (TRA/TRD) genes. We have identified in silico the TRG and TRA/TRD genes and analyzed the relevant mature transcripts in blood and in skin from four subjects. The dolphin TRG locus is the smallest and simplest of all mammalian loci as yet studied. It shows a genomic organization comprising two variable (V1 and V2), three joining (J1, J2 and J3) and a single constant (C), genes. Despite the fragmented nature of the genome assemblies, we deduced the TRA/TRD locus organization, with the recent TRDV1 subgroup genes duplications, as it is expected in artiodactyls. Expression analysis from blood of a subject allowed us to assign unambiguously eight TRAV genes to those annotated in the genomic sequence and to twelve new genes, belonging to five different subgroups.