Hematology/ Oncology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Budgetpresentation.Univeresity of Pittsburgh 2021.Pdf
One of the most innovative universities in the world — Reuters The top public university in the Northeast — The Wall Street Journal/ Times Higher Education Among the top 20 public schools in the nation — U.S. News & World Report $4.2 Billion in economic impact in Pennsylvania — EI Report Data Budget Presentation to the General Assembly of the Commonwealth of Pennsylvania 2021–22 CONTENTS CHANCELLOR’S STATEMENT ...................................................................................1 OUR IMPACT .....................................................................................................................2 The Student Experience ..................................................................................................3 Outstanding Faculty .........................................................................................................5 Research Strength ............................................................................................................5 Combating the Opioid Crisis in Pennsylvania ...........................................................6 Engaging with the Community for Impact .................................................................8 Pitt Partnering as an Economic Driver .....................................................................11 Innovation and Entrepreneurship ..............................................................................12 Pitt Ventures ....................................................................................................................13 -
Blood Products Advisory Committee March 21, 2019 Meeting Transcript- Topic 3
FOOD AND DRUG ADMINISTRATION (FDA) Center for Biologics Evaluation and Research (CBER) th 120 Meeting of the Blood Products Advisory Committee OPEN PUBLIC MEETING FDA White Oak Campus 10903 New Hampshire Avenue Silver Spring, MD 20993 March 21, 2019 This transcript appears as received from the commercial transcribing service after inclusion of minor corrections to typographical and factual errors as recommended by the DFO. PARTICIPANTS Richard M. Kaufman, M.D. Brigham and Women’s Hospital Prabhakara Atreya, PhD Food and Drug Administration (FDA) UCLA- Division of Pediatric Judith Baker, Dr.PH, MHSA Hematology/Oncology Sridhar V. Basavaraju, M.D. Centers for Disease Control and Prevention Evan Bloch, M.D., M.S. Johns Hopkins University School of Medicine Barbara Bryant, M.D. University of Texas Medical Branch Meera B. Chitlur, M.D. Wayne State University Bureau of Infectious Disease and Laboratory Alfred DeMaria, M.D. Science Walter Reed National Military Medical Michael DeVan, M.D. Center Roger Lewis, M.D., Ph.D. Harbor-UCLA Medical Center Thomas Ortel, M.D., Ph.D. Duke University Medical Center Martin Schreiber, M.D. Oregon Health & Sciences University Amy Shapiro, M.D. Indiana Hemophilia and Thrombosis Center Jack Stapleton, M.D. University of Iowa Susan L. Stramer, Ph.D. American Red Cross F. Blaine Hollinger, M.D. Baylor College of Medicine Christopher Templin Patient Representative Anne Eder, M.D., Ph.D. Office of Blood Research and Review, FDA Mindy Goldman, M.D. Canadian Blood Services John Brooks, M.D. Centers for Disease Control and Prevention 3 Office of Biostatistics and Epidemiology, Alan Williams, Ph.D. -

Ashi Accredited Laboratories 2021
ASHI ACCREDITED LABORATORIES 2021 1120 Route 73, Suite 200 Mount Laurel, NJ 08054 Phone: 856-638-0428 Fax: 856-439-0525 www.ashi-hla.org Updated: February 2021 Histocompatibility Laboratories Histocompatibility laboratories are organized alphabetically by state and institution, followed by those in countries outside the United States. Each laboratory has a current address, director, supervisor (if applicable), phone and fax numbers. Each has been characterized for tests and accreditation, as follows: Test Performed: Serologic Typing Class I (Serology: Class I) Serologic Typing Class II (Serology: Class II) DNA Typing Class I (DNA: Class I) DNA Typing Class II (DNA: Class II) Next Generation Sequencing (NGS) Flow Cytometry (Flow) MLC (MLC) Monitoring for Engraftment (Mont. For Engraft.) Antibody Screening (Antibody Screening) Antibody Identification (Antibody ID) Crossmatch (Crossmatch) ABO/RH Typing (ABO/RH) ASHI Accreditation Categories: HSC/BM Transplantation: Related Donor (HSC/BM: Related) HSC/BM Transplantation: Unrelated Donor (HSC/BM: Unrelated) Solid Organ Transplantation: Deceased Donor (Solid Organ: Deceased) Solid Organ Transplantation: Live Donor (Solid Organ: Live) Histocompatibility Testing for Other Clinical Purposes (Typing for Non-TX) Transfusion Support (Transfusion Support) 2 UNITED STATES (AL – AR) Alabama 11-6-AZ-03-1 Banner University Medical Center – Tucson 10-3-AL-02-2 HLA Laboratory UAB Comprehensive Transplant Institute Department of Pathology Histocompatibility and Immunogenetics Laboratory 1625 N. Campbell -

Philip J. Norris University of California San Francisco Prepared: 10/10/2018
Philip J. Norris University of California San Francisco Prepared: 10/10/2018 CURRICULUM VITAE Name: Philip John Norris Position: Adjunct Professor Department of Laboratory Medicine Clinical Professor Department of Medicine University of California, San Francisco Senior Investigator and Director of Laboratory Sciences, SF Vitalant Research Institute Vice President, Research and Scientific Programs Vitalant Address: Vitalant Research Institute 270 Masonic Avenue San Francisco, CA 94118 Voice: (415) 923-5769 FAX: (415) 567-5899 email: [email protected] WWW: https://research.vitalant.org/Investigators/Philip-Norris EDUCATION: 1985-1989 University of California, Berkeley B.A. Molecular Biology 1985-1989 University of California, Berkeley B.S. Bioengineering 1991-1995 College of Physicians & Surgeons, Columbia University M.D. 1995-1996 The Presbyterian Hospital in the City of New York Intern Internal Medicine 1996-1998 Duke University Medical Center Resident Internal Medicine 1998-2001 Massachusetts General Hospital and FelloW Infectious Diseases Brigham and Women’s Hospital, Harvard University LICENSES, CERTIFICATION: 1995 Diplomate of National Board of Medical Examiners 1996 Diplomate of American Board of Internal Medicine 1996-2010 Board Certified in Internal Medicine 2000-noW Board Certified in Infectious Diseases 2004 California medical license, number A87646 PRINICIPAL POSITIONS HELD: 2002-2003 Massachusetts General Hospital Instructor in Medicine 2004-2012 Vitalant Research Institute Associate Investigator 2012-noW Senior Investigator -
2020 Single Audit Report
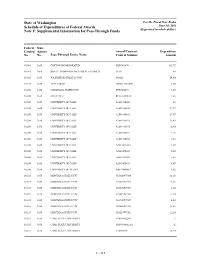
State of Washington For the Fiscal Year Ended Schedule of Expenditures of Federal Awards June 30, 2020 (Expressed in whole dollars) Note F: Supplemental Information for Pass-Through Funds Federal State Catalog Agency Award/Contract Expenditure No. No. Pass-Through Entity Name Control Number Amount 10.001 3650 COTTON INCORPORATED WSU003470 183,737 10.025 3600 BOYCE THOMPSON INST FOR PLANT RSCH 19-03 865 10.025 3650 WA STATE RECREAT & CON 182432 24,008 10.170 3650 VIVA FARMS ORSO131825001 4,680 10.200 3650 COLORADO STATE UNIV WSU004075 1,370 10.200 3650 MI ST UNIV RC110588WSU 7,252 10.200 3650 UNIVERSITY OF CALIF A180916S003 687 10.200 3650 UNIVERSITY OF CALIF A180916S004 17,711 10.200 3650 UNIVERSITY OF CALIF A180916S066 27,357 10.200 3650 UNIVERSITY OF CALIF A180916S074 75,070 10.200 3650 UNIVERSITY OF CALIF A180916S076 18,401 10.200 3650 UNIVERSITY OF CALIF A180916S077 3,353 10.200 3650 UNIVERSITY OF CALIF A180916S082 8,811 10.200 3650 UNIVERSITY OF CALIF A201347A010 1,197 10.200 3650 UNIVERSITY OF CALIF A201347S003 5,407 10.200 3650 UNIVERSITY OF CALIF A201347S005 5,255 10.200 3650 UNIVERSITY OF CALIF A201347S029 1,679 10.200 3650 UNIVERSITY OF IDAHO BJKP36SB003 1,122 10.215 3650 MONTANA STATE UNIV G13020W7504 11,131 10.215 3650 MONTANA STATE UNIV G13220W7504 14,214 10.215 3650 MONTANA STATE UNIV G13520W7507 1,266 10.215 3650 MONTANA STATE UNIV G16219W7506 15,536 10.215 3650 MONTANA STATE UNIV G16920W7507 4,328 10.215 3650 MONTANA STATE UNIV G23620W7504 11,811 10.215 3650 MONTANA STATE UNIV G26219W7502 12,286 10.215 3650 UTAH STATE UNIVERSITY 130676002240 -11 10.215 3650 UTAH STATE UNIVERSITY 15089300001266 -13 10.215 3650 UTAH STATE UNIVERSITY 150893169 14,505 F - 215 State of Washington For the Fiscal Year Ended Schedule of Expenditures of Federal Awards June 30, 2020 (Expressed in whole dollars) Note F: Supplemental Information for Pass-Through Funds Federal State Catalog Agency Award/Contract Expenditure No. -

Cornell University Single Audit Report
Cornell University Report on Federal Awards in Accordance with the Uniform Guidance June 30, 2020 EIN: 15-0532082 Cornell University Index June 30, 2020 Page(s) Report of Independent Auditors .............................................................................................................................. 1–3 Consolidated Financial Statements .......................................................................................................................... 4–6 Notes to Consolidated Financial Statements ......................................................................................................... 7–46 Financial Responsibility Supplemental Schedule ...................................................................................................... 47 Note to Financial Responsibility Supplemental Schedule ......................................................................................... 48 Schedule of Expenditures of Federal Awards ...................................................................................................... 49–73 Notes to Schedule of Expenditures of Federal Awards ............................................................................................. 74 Report of Independent Auditors on Internal Control Over Financial Reporting and on Compliance and Other Matters Based on an Audit of Financial Statements Performed in Accordance with Government Auditing Standards ................................. 75–76 Report of Independent Auditors on Compliance with Requirements That -

1 Use of US Blood Donors for National Serosurveillance of SARS-Cov-2 Antibodies
medRxiv preprint doi: https://doi.org/10.1101/2021.05.01.21255576; this version posted May 3, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-ND 4.0 International license . 1 Use of U.S. Blood Donors for National Serosurveillance of SARS-CoV-2 Antibodies: Basis for an 2 Expanded National Donor Serosurveillance Program. 3 4 Mars Stone1,2, Clara Di Germanio1, David J. Wright3, Hasan Sulaeman1, Honey Dave1, Rebecca V. 5 Fink3, Edward P. Notari4, Valerie Green5, Donna Strauss6, Debra Kessler6, Mark Destree7, Paula Saa4, 6 Phillip C. Williamson1,5, Graham Simmons1,2, Susan L. Stramer4, Jean Opsomer3, Jefferson M. Jones8, 7 Steven Kleinman9, Michael P. Busch1,2; for the NHLBI Recipient Epidemiology and Donor Evaluation 8 Study-IV-Pediatric (REDS-IV-P) 9 1. Vitalant Research Institute (VRI), San Francisco, CA 10 2. Department of Laboratory Medicine, University of California, San Francisco, CA 11 3. Westat, Rockville, MD 12 4. American Red Cross (ARC), Gaithersburg, MD 13 5. Creative Testing Solutions (CTS), Tempe, AZ 14 6. New York Blood Center (NYBC), New York, NY 15 7. BloodWorks Northwest, Seattle, WA 16 8. Centers for Disease Control and Prevention COVID-19 Response Team, Atlanta, Georgia 17 9. University of British Columbia, Victoria, BC, Canada 18 19 Corresponding author: Michael P. Busch MD, PhD. Address: Vitalant Research Institute, 270 20 Masonic Avenue, San Francisco, CA, United States 94118. Phone: 1-415-354-1389. -

FY 2019 Form 990 Emory University
Clark, Susan P From: [email protected] Sent: Wednesday, July 15, 2020 1:05 PM To: Clark, Susan P Cc: Clark, Susan P Subject: [External] Emory University 2018 Form 990 has been Accepted! Dear Susan: Congratulations! The 2018 Form 990 for Emory University has been accepted by the IRS. Regards, Crowe LLP (CTRAC Team) This email message is from Crowe LLP or one of its subsidiaries and may contain privileged or confidential information or other information exempt from disclosure under applicable law. If you are not the intended recipient, please notify the sender by reply email immediately and delete this message without reading further or forwarding to others. This email is not intended to be a contract or other legally binding obligation, and any tax advice expressed in this email should not be construed as a formal tax opinion unless expressly stated. Visit www.crowe.com/disclosure for more information about Crowe LLP and its subsidiaries. 1 Form 990 (2018) Page 2 Part III Statement of Program Service Accomplishments Check if Schedule O contains a response or note to any line in this Part III . ✔ 1 Briefly describe the organization’s mission: EMORY UNIVERSITY'S MISSION IS TO CREATE, PRESERVE, TEACH, AND APPLY KNOWLEDGE IN THE SERVICE OF HUMANITY. (SEE SCHEDULE O FOR CONTINUATION) 2 Did the organization undertake any significant program services during the year which were not listed on the prior Form 990 or 990-EZ? . Yes No If “Yes,” describe these new services on Schedule O. 3 Did the organization cease conducting, or make significant changes in how it conducts, any program services? . -

Thank You to Members of NIAID Peer Review Groups and Advisory Committees
Thank You to Members of NIAID Peer Review Groups and Advisory Committees NIH's ability to fund outstanding science hinges in large part on the generosity of scientists and lay people who serve on its hundreds of peer review and advisory committees, including our NIAID Council Members. Learn more about Serving on a Peer Review Committee and how to become a peer reviewer. Whether you traveled to the Washington, D.C., area or participated by teleconference, you donated valuable time and effort to make an enormous and irreplaceable contribution to biomedical science. In recognition, we'd like to take a moment to thank people who participated on NIAID peer review groups, listed below. We'd also like to thank the people who serve on the Center for Scientific Review Study Sections for NIAID applications, though we do not list you individually here. List of Fiscal Year 2020 NIAID Peer Review Group Members These data are sorted by name. To search for a name or organizational affiliation, use control-F (command-F for Mac). Send questions or corrections to [email protected]. Name Affiliation Abazeed, Mohamed E., M.D., Ph.D. Northwestern University Abbate, Antonio, M.D., Ph.D. Virginia Commonwealth University Abimiku, Alash'Le G., Ph.D. University of Maryland, Baltimore Abramovitch, Robert B., Ph.D. Michigan State University Aceves, Seema S., M.D., Ph.D. University of California, San Diego Acharya, Abhinav, Ph.D. Arizona State University Ackerman, Steven Jules, Ph.D. University of Illinois at Chicago Adachi, Roberto, M.D. University of Texas MD Anderson Cancer Center Adamko, Darryl, M.D.