Risk Acute Myeloid Leukemia Patients
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
![HEF1 (NEDD9) Mouse Monoclonal Antibody [Clone ID: 2G9] Product Data](https://docslib.b-cdn.net/cover/6906/hef1-nedd9-mouse-monoclonal-antibody-clone-id-2g9-product-data-66906.webp)
HEF1 (NEDD9) Mouse Monoclonal Antibody [Clone ID: 2G9] Product Data
OriGene Technologies, Inc. 9620 Medical Center Drive, Ste 200 Rockville, MD 20850, US Phone: +1-888-267-4436 [email protected] EU: [email protected] CN: [email protected] Product datasheet for TA319568 HEF1 (NEDD9) Mouse Monoclonal Antibody [Clone ID: 2G9] Product data: Product Type: Primary Antibodies Clone Name: 2G9 Applications: IF, WB Recommend Dilution: ELISA: 1:5,000 - 1:20,000, WB: 1:5,000, IF: 1:500, IP: 1:1,000 Reactivity: Human Host: Mouse Clonality: Monoclonal Immunogen: Anti-HEF1 monoclonal antibody was produced by repeated immunizations with a synthetic peptide corresponding to amino acid residues 82-398 of human HEF1 protein (hHEF1, 843 aa, predicted MW 92.8 kDa). Formulation: 0.02 M Potassium Phosphate, 0.15 M Sodium Chloride, pH 7.2 Concentration: 1 mg/ml Gene Name: neural precursor cell expressed, developmentally down-regulated 9 Database Link: NP_001135865 Entrez Gene 4739 Human Synonyms: CAS-L; CAS2; CASL; CASS2; HEF1 This product is to be used for laboratory only. Not for diagnostic or therapeutic use. View online » ©2020 OriGene Technologies, Inc., 9620 Medical Center Drive, Ste 200, Rockville, MD 20850, US 1 / 3 HEF1 (NEDD9) Mouse Monoclonal Antibody [Clone ID: 2G9] – TA319568 Note: HEF1, also known as Enhancer of filamentation 1, CRK-associated substrate-related protein, CAS-L, CasL, p105 and Neural precursor cell expressed developmentally down-regulated 9 is the product of the NEDD9 (CASGL) gene. HEF1 functions as a docking protein that plays a central coordinating role for tyrosine-kinase-based signaling related to cell adhesion. HEF1 may also function in transmitting growth control signals between focal adhesions at the cell periphery and the mitotic spindle in response to adhesion or growth factor signals initiating cell proliferation. -
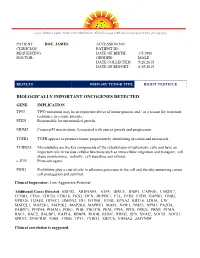
Sample Lab Report
3030 Venture Lane, Suite 108 ● Melbourne, Florida 32934 ● Phone 321-253-5197 ● Fax 321-253-5199 PATIENT: DOE, JAMES ACCESSION NO: CLINICIAN/ PATIENT ID: REQUESTING DATE OF BIRTH: 1/5/1986 DOCTOR: GENDER: MALE DATE COLLECTED: 5/26/2015 DATE OF REPORT: 6/15/2015 RESULTS PRIMARY TUMOR TYPE RIGHT TESTICLE BIOLOGICALLY IMPORTANT ONCOGENES DETECTED GENE IMPLICATION TP53 TP53 mutations may be an important driver of tumorigenesis and / or a reason for treatment resistance in a some patients. PTEN Responsible for uncontrolled growth. MDM2 Causes p53 inactivation. Associated with cancer growth and progression. TGFB1 TGFB appears to promote tumor progession by stimulating invasion and metastasis. TUBB2A Microtubules are the key components of the cytoskeleton of eukaryotic cells and have an important role in various cellular functions such as intracellular migration and transport, cell shape maintenance, polarity, cell signaling and mitosis. c-JUN Proto-oncogene PHB2 Prohibitins play a crucial role in adhesion processes in the cell and thereby sustaining cancer cell propagation and survival. Clinical Impression: Low Aggressive Potential Additional Genes Detected: ABCG2, ARHGAP5, ATF4, BIRC5, BNIP3, CAPNS1, CARD17, CCNB1, CD24, CDC20, CDK18, CKS2, DCN, DEPDC1, FTL, FZD5, FZD9, GAPDH, GNB2, GPR126, H2AFZ, HDAC1, HMGN2, ID1, IFITM1, JUNB, KPNA2, KRT18, LDHA, LTF, MAD2L1, MAP2K1, MAP2K2, MAP2K4, MAPRE1, MAS1, NME1, NME3, NPM1, PA2G4, PABPC1, PFDN4, PGAM1, PGK1, PHB, PIK3CB, PKM, PPIA, PPIH, PRKX, PRNP, PTMA, RAC1, RAC2, RALBP1, RAP1A, RBBP4, RHOB, RHOC, -

CRKL As a Lung Cancer Oncogene and Mediator Of
views in The spotliGhT CRKL as a Lung Cancer Oncogene and Mediator of Acquired Resistance to eGFR inhibitors: is it All That it is Cracked Up to Be? Marc Ladanyi summary: Cheung and colleagues demonstrate that amplified CRKL can function as a driver oncogene in lung adeno- carcinoma, activating both RAS and RAP1 to induce mitogen-activated protein kinase signaling. In addition, they show that CRKL amplification may be another mechanism for primary or acquired resistance to epidermal growth factor re- ceptor kinase inhibitors. Cancer Discovery; 1(7); 560–1. ©2011 AACR. Commentary on Cheung et al., p. 608 (1). In this issue of Cancer Discovery, Cheung and colleagues (1) mutual exclusivity. Cheung and colleagues (1) report that present extensive genomic and functional data supporting focal CRKL amplification is mutually exclusive with EGFR focal amplification of the CRKL gene at 22q11.21 as a driver mutation and EGFR amplification. However, of the 6 lung oncogene in lung adenocarcinoma. The report expands on cancer cell lines found in this study to have focal gains of data previously presented by Kim and colleagues (2). CRKL CRKL, 2 contain other major driver oncogenes (KRAS G13D is a signaling adaptor protein that contains SH2 and SH3 in HCC515, BRAF G469A in H1755; refs. 7, 8). Interestingly, domains that mediate protein–protein interactions linking both cell lines demonstrated clear dependence on CRKL in tyrosine-phosphorylated upstream signaling molecules (e.g., functional assays. Perhaps CRKL amplification is more akin BCAR1, paxillin, GAB1) to downstream effectors (e.g., C3G, to PIK3CA mutations, which often, but not always, are con- SOS) (3). -

Immunohistochemical Expression of NEDD9, E-Cadherin and Γ-Catenin and Their Prognostic Significance in Pancreatic Ductal Adenocarcinoma (PDAC)
BOSNIAN JOURNAL of Basic Medical Sciences RESEARCH ARTICLE WWW.BJBMS.ORG Immunohistochemical expression of NEDD9, E-cadherin and γ-catenin and their prognostic significance in pancreatic ductal adenocarcinoma (PDAC) Petra Radulović*, Božo Krušlin Department of Pathology and Cytology, Sestre Milosrdnice University Hospital, Zagreb, Croatia ABSTRACT Extensive research is being conducted to identify novel diagnostic, predictive and prognostic biomarkers for pancreatic ductal adenocarcinoma (PDAC), as only a few markers have been routinely used so far with limited success. Our aim was to assess the expression of neural precur- sor cell expressed developmentally down-regulated protein 9 (NEDD9), E-cadherin, and γ-catenin in PDAC in relation to clinicopathological parameters and patient survival. We also investigated if there is a correlation of NEDD9 expression with E-cadherin or γ-catenin. The protein expression was determined by immunohistochemistry in 61 PDAC and 61 samples of normal pancreatic tissue. The log rank test and Kaplan- Meier survival curve were used for survival analysis. E-cadherin and γ-catenin expressions were reduced in PDAC, and completely retained in normal pancreatic tissue. Expression of NEDD9 was significantly increased in PDAC (strong expression in 78.7% of cases and moderate in 21.3%) and reduced in normal pancreatic tissue (strong positivity in 45.9% of cases, moderate in 31.1%, and weak in 23%). There was a positive correlation between reduced E-cadherin and γ-catenin expression in PDAC (p = 0.015). The loss or reduced expression of E-cadherin had a negative impact on patient survival (p = 0.020). A negative correlation between E-cadherin expression and tumor grade was also observed (p = 0.011). -
Conditional Ablation of P130cas/BCAR1 Adaptor Protein
Camacho Leal et al. Cell Communication and Signaling (2018) 16:73 https://doi.org/10.1186/s12964-018-0289-z RESEARCH Open Access Conditional ablation of p130Cas/BCAR1 adaptor protein impairs epidermal homeostasis by altering cell adhesion and differentiation Maria del Pilar Camacho Leal†, Andrea Costamagna†, Beatrice Tassone, Stefania Saoncella, Matilde Simoni, Dora Natalini, Aurora Dadone, Marianna Sciortino, Emilia Turco, Paola Defilippi, Enzo Calautti‡ and Sara Cabodi*‡ Abstract Background: p130 Crk-associated substrate (p130CAS; also known as BCAR1) is a scaffold protein that modulates many essential cellular processes such as cell adhesion, proliferation, survival, cell migration, and intracellular signaling. p130Cas has been shown to be highly expressed in a variety of human cancers of epithelial origin. However, few data are available regarding the role of p130Cas during normal epithelial development and homeostasis. Methods: To this end, we have generated a genetically modified mouse in which p130Cas protein was specifically ablated in the epidermal tissue. Results: By using this murine model, we show that p130Cas loss results in increased cell proliferation and reduction of cell adhesion to extracellular matrix. In addition, epidermal deletion of p130Cas protein leads to premature expression of “late” epidermal differentiation markers, altered membrane E-cadherin/catenin proteins localization and aberrant tyrosine phosphorylation of E-cadherin/catenin complexes. Interestingly, these alterations in adhesive properties in absence -

Expression Profiling of KLF4
Expression Profiling of KLF4 AJCR0000006 Supplemental Data Figure S1. Snapshot of enriched gene sets identified by GSEA in Klf4-null MEFs. Figure S2. Snapshot of enriched gene sets identified by GSEA in wild type MEFs. 98 Am J Cancer Res 2011;1(1):85-97 Table S1: Functional Annotation Clustering of Genes Up-Regulated in Klf4 -Null MEFs ILLUMINA_ID Gene Symbol Gene Name (Description) P -value Fold-Change Cell Cycle 8.00E-03 ILMN_1217331 Mcm6 MINICHROMOSOME MAINTENANCE DEFICIENT 6 40.36 ILMN_2723931 E2f6 E2F TRANSCRIPTION FACTOR 6 26.8 ILMN_2724570 Mapk12 MITOGEN-ACTIVATED PROTEIN KINASE 12 22.19 ILMN_1218470 Cdk2 CYCLIN-DEPENDENT KINASE 2 9.32 ILMN_1234909 Tipin TIMELESS INTERACTING PROTEIN 5.3 ILMN_1212692 Mapk13 SAPK/ERK/KINASE 4 4.96 ILMN_2666690 Cul7 CULLIN 7 2.23 ILMN_2681776 Mapk6 MITOGEN ACTIVATED PROTEIN KINASE 4 2.11 ILMN_2652909 Ddit3 DNA-DAMAGE INDUCIBLE TRANSCRIPT 3 2.07 ILMN_2742152 Gadd45a GROWTH ARREST AND DNA-DAMAGE-INDUCIBLE 45 ALPHA 1.92 ILMN_1212787 Pttg1 PITUITARY TUMOR-TRANSFORMING 1 1.8 ILMN_1216721 Cdk5 CYCLIN-DEPENDENT KINASE 5 1.78 ILMN_1227009 Gas2l1 GROWTH ARREST-SPECIFIC 2 LIKE 1 1.74 ILMN_2663009 Rassf5 RAS ASSOCIATION (RALGDS/AF-6) DOMAIN FAMILY 5 1.64 ILMN_1220454 Anapc13 ANAPHASE PROMOTING COMPLEX SUBUNIT 13 1.61 ILMN_1216213 Incenp INNER CENTROMERE PROTEIN 1.56 ILMN_1256301 Rcc2 REGULATOR OF CHROMOSOME CONDENSATION 2 1.53 Extracellular Matrix 5.80E-06 ILMN_2735184 Col18a1 PROCOLLAGEN, TYPE XVIII, ALPHA 1 51.5 ILMN_1223997 Crtap CARTILAGE ASSOCIATED PROTEIN 32.74 ILMN_2753809 Mmp3 MATRIX METALLOPEPTIDASE -

Breast Cancer Antiestrogen Resistance-3 Expression Regulates Breast Cancer Cell Migration Through Promotion of P130cas Membrane Localization Andmembrane Ruffling
Research Article Breast Cancer Antiestrogen Resistance-3 Expression Regulates Breast Cancer Cell Migration through Promotion of p130Cas Membrane Localization andMembrane Ruffling Randy S. Schrecengost,1 Rebecca B. Riggins,2 Keena S. Thomas,1 Michael S. Guerrero,1 and Amy H. Bouton1 1Department of Microbiology, University of Virginia Health System, Charlottesville, Virginia and 2Department of Oncology, Lombardi Comprehensive Cancer Center, Georgetown University, Washington, District of Columbia Abstract antiestrogen resistance-1 (BCAR1; also known as p130Cas; refs. 2, 3). Antiestrogens such as tamoxifen are widely used in the clinic A second protein, BCAR3 (the human homologue of the murine to treat estrogen receptor–positive breast tumors. Resistance protein AND-34), was identified in a genetic screen along with to tamoxifen can occur either de novo or develop over time in BCAR1 as a gene product whose overexpression conferred tamoxifen resistance in vitro (4). BCAR3 is a member of the novel a large proportion of these tumors. Additionally, resistance is S p associated with enhanced motility and invasiveness in vitro. rc homology 2 (SH2)–containing rotein (NSP) family that One molecule that has been implicated in tamoxifen resis- includes two other members, Chat/SHEP1 and NSP1. These tance, breast cancer antiestrogen resistance-3 (BCAR3), has proteins share a common domain structure consisting of an also been shown to regulate migration of fibroblasts. In this amino-terminal SH2 domain and a carboxyl-terminal domain with study, we investigated the role of BCAR3 in breast cancer cell sequence homology to the Cdc25-family of guanine nucleotide exchange factors (GEF). Several studies have shown that BCAR3 migration and invasion. -

Dioxin) Receptor
TOXICOLOGICAL SCIENCES 124(1), 1–22 (2011) doi:10.1093/toxsci/kfr218 Advance Access publication September 9, 2011 Exactly the Same but Different: Promiscuity and Diversity in the Molecular Mechanisms of Action of the Aryl Hydrocarbon (Dioxin) Receptor Michael S. Denison,*,1 Anatoly A. Soshilov,* Guochun He,* Danica E. DeGroot,* and Bin Zhao† Downloaded from *Department of Environmental Toxicology, University of California, Davis, California 95616; and †Research Center for Eco-Environmental Sciences, Chinese Academy of Sciences, Beijing, China 1To whom correspondence should be addressed at Department of Environmental Toxicology, University of California, Meyer Hall, One Shields Avenue, Davis, CA 95616-8588. Fax: (530) 752-3394. E-mail: [email protected]. http://toxsci.oxfordjournals.org/ Received June 6, 2011; accepted August 12, 2011 toxic effects in a wide range of species and tissues (Beischlag The Ah receptor (AhR) is a ligand-dependent transcription et al., 2008; Furness and Whelan, 2009; Hankinson, 2005; factor that mediates a wide range of biological and toxicological Humblet et al., 2008; Marinkovic´ et al., 2010; Poland and effects that result from exposure to a structurally diverse variety Knutson, 1982; Safe, 1990; White and Birnbaum, 2009). The of synthetic and naturally occurring chemicals. Although the overall mechanism of action of the AhR has been extensively best-characterized high-affinity ligands for the AhR include at University of California, Davis - Library on May 4, 2012 studied and involves a classical nuclear receptor mechanism of a wide variety of ubiquitous hydrophobic environmental action (i.e., ligand-dependent nuclear localization, protein hetero- contaminants such as the halogenated aromatic hydrocarbons dimerization, binding of liganded receptor as a protein complex to (HAHs) and nonhalogenated polycyclic aromatic hydrocarbons its specific DNA recognition sequence and activation of gene (PAHs). -

This Research Was Originally Published in the Journal of Biological Chemistry
This research was originally published in The Journal of Biological Chemistry. By Bradbury P, Bach CT, Paul A, O’Neill GM, Titled: Src Kinase Determines the Dynamic Exchange of the Docking Protein NEDD9 (Neural Precursor Cell Expressed Developmentally Down-regulated Gene 9) at Focal Adhesions. 2014 ;289(36): 24792-24800. doi:10.1074/jbc.M113.544106. Final publication is available at http://www.jbc.org/content/289/36/24792.long © 2016 The American Society for Biochemistry and Molecular Biology. Src and molecular exchange at adhesions Src Kinase Determines the Dynamic Exchange of the Docking Protein NEDD9 at Focal Adhesions* Peta Bradbury,1, 2 Cuc T Bach,1 Andre Paul,1 and Geraldine M O’Neill1, 2 1From the Children’s Cancer Research Unit, Kids Research Institute at The Children’s Hospital at Westmead, NSW, 2145 2Discipline of Paediatrics and Child Health, University of Sydney, NSW, 2006 * Running title: Src and molecular exchange at adhesions To whom correspondence should be addressed: Geraldine M. O’Neill, Children’s Cancer Research Unit, The Children’s Hospital at Westmead, Locked Bag 4001, Westmead, 2145, Australia Tel.: 61 2 98451206; Fax: 61 2 98453078; Email: [email protected] Key Words: NEDD9; focal adhesion; FRAP; Src kinase; FAK; migration Background: Dynamic exchange provides a focal adhesions is key in modulating rates of mechanism for rapidly reorganizing migration and invasion. Our study suggests that macromolecular structures. Src kinase activity determines NEDD9 Results: Exchange of the focal adhesion targeted exchange at focal adhesions and may similarly protein NEDD9 between the cytoplasm and focal modulate other focal adhesion-targeted Src adhesions is faster in the absence of Src kinase substrates to regulate cell migration. -

Genomic and Functional Analysis Identifies CRKL As an Oncogene
Oncogene (2010) 29, 1421–1430 & 2010 Macmillan Publishers Limited All rights reserved 0950-9232/10 $32.00 www.nature.com/onc ORIGINAL ARTICLE Genomic and functional analysis identifies CRKL as an oncogene amplified in lung cancer YH Kim1,7, KA Kwei1,7, L Girard2, K Salari1,3, J Kao1, M Pacyna-Gengelbach4, P Wang5, T Hernandez-Boussard3, AF Gazdar2, I Petersen6, JD Minna2 and JR Pollack1 1Department of Pathology, Stanford University, Stanford, CA, USA; 2Hamon Center for Therapeutic Oncology Research, University of Texas Southwestern Medical Center, Dallas, TX, USA; 3Department of Genetics, Stanford University, Stanford, CA, USA; 4Institute of Pathology, University Hospital Charite´, Berlin, Germany; 5Division of Public Health Sciences, Fred Hutchinson Cancer Research Center, Seattle, WA, USA and 6Institute of Pathology, Universita¨tsklinikum Jena, Jena, Germany DNA amplifications, leading to the overexpression of related mortality (Jemal et al., 2008). Nearly 80% oncogenes, are a cardinal feature of lung cancer and of lung cancers diagnosed are non-small-cell lung directly contribute to its pathogenesis. To uncover such cancers (NSCLCs), which are classified into three main novel alterations, we performed an array-based compara- histological subtypes: adenocarcinoma, squamous cell tive genomic hybridization survey of 128 non-small-cell carcinoma and large cell carcinoma. Despite the lung cancer cell lines and tumors. Prominent among our advancement of surgical, cytotoxic and radiological findings, we identified recurrent high-level amplification at treatment options over the years, lung cancer therapy cytoband 22q11.21 in 3% of lung cancer specimens, with remains largely ineffective from a clinical standpoint, another 11% of specimens exhibiting low-level gain spanning as evidenced by a low 5-year survival rate (o15%), that locus. -

NEDD9 Depletion Destabilizes Aurora a Kinase and Heightens the Efficacy of Aurora a Inhibitors: Implications for Treatment of Metastatic Solid Tumors
Published OnlineFirst March 28, 2013; DOI: 10.1158/0008-5472.CAN-12-4008 Cancer Tumor and Stem Cell Biology Research NEDD9 Depletion Destabilizes Aurora A Kinase and Heightens the Efficacy of Aurora A Inhibitors: Implications for Treatment of Metastatic Solid Tumors Ryan J. Ice4, Sarah L. McLaughlin4, Ryan H. Livengood3, Mark V. Culp2, Erik R. Eddy2, Alexey V. Ivanov1,4, and Elena N. Pugacheva1,4 Abstract Aurora A kinase (AURKA) is overexpressed in 96% of human cancers and is considered an independent marker of poor prognosis. While the majority of tumors have elevated levels of AURKA protein, few have AURKA gene amplification, implying that posttranscriptional mechanisms regulating AURKA protein levels are significant. Here, we show that NEDD9, a known activator of AURKA, is directly involved in AURKA stability. Analysis of a comprehensive breast cancer tissue microarray revealed a tight correlation between the expression of both proteins, significantly corresponding with increased prognostic value. A decrease in AURKA, concomitant with increased ubiquitination and proteasome-dependent degradation, occurs due to depletion or knockout of NEDD9. Reexpression of wild-type NEDD9 was sufficient to rescue the observed phenomenon. Binding of NEDD9 to AURKA is critical for AURKA stabilization, as mutation of S296E was sufficient to disrupt binding and led to reduced AURKA protein levels. NEDD9 confers AURKA stability by limiting the binding of the cdh1–substrate recognition subunit of APC/C ubiquitin ligase to AURKA. Depletion of NEDD9 in tumor cells increases sensitivity to AURKA inhibitors. Combination therapy with NEDD9 short hairpin RNAs and AURKA inhibitors impairs tumor growth and distant metastasis in mice harboring xenografts of breast tumors. -

Expression of NEDD9 in Hepatocellular Carcinoma and Its Clinical Significance
ONCOLOGY REPORTS 33: 2375-2383, 2015 Expression of NEDD9 in hepatocellular carcinoma and its clinical significance PENG LU1,2*, ZHI-PENG WANG3*, ZHENG DANG4*, ZHI-GANG ZHENG1*, XIAO LI1, LIANG ZHOU5, RUI DING1, SHU-QIANG YUE1 and KE-FENG DOU1 1Department of Hepatobiliary and Pancreaticosplenic Surgery, Xijing Hospital, The Fourth Military Medical University; 2Department of General Surgery, The 518 Central Hospital of PLA; 3Department of Pharmacology, School of Pharmacy, The Fourth Military Medical University, Xi'an, Shanxi; 4Department of Hepatobiliary Surgery, Lanzhou General Hospital of PLA, Lanzhou, Gansu; 5Department of General Surgery, The 155 Central Hospital of PLA, Kaifeng, He'nan, P.R. China Received December 1, 2014; Accepted January 22, 2015 DOI: 10.3892/or.2015.3863 Abstract. Neural precursor cell expressed, developmentally metastasis, intrahepatic venous invasion and high UICC TNM downregulated 9 (NEDD9) plays an integral role in natural and stages in HCC patients. Patients with high NEDD9 expression pathological cell biology. Overexpression of NEDD9 protein levels exhibited poorer recurrence-free and overall survival has been correlated with poor prognosis in various types of than those with a low NEDD9 expression. Additionally, cancer. However, few available data address the precise func- NEDD9 expression status was an independent prognostic tion of the NEDD9 gene in hepatocellular carcinoma (HCC). factor for survival. This correlation remained significant in In the present study, we investigated NEDD9 expression patients with early-stage HCC or with normal serum AFP in 40 primary human HCC tissues compared with matched levels. The results of this study suggest that NEDD9 may be a adjacent non-tumor hepatic tissues using RT-qPCR and valuable prognostic biomarker for HCC, including early-stage western blot analysis.