Imatinib-Dependent Tyrosine Phosphorylation Profiling of Bcr-Abl
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Proximal Signaling Network of the BCR-ABL1 Oncogene Shows a Modular Organization
Oncogene (2010) 29, 5895–5910 & 2010 Macmillan Publishers Limited All rights reserved 0950-9232/10 www.nature.com/onc ORIGINAL ARTICLE The proximal signaling network of the BCR-ABL1 oncogene shows a modular organization B Titz, T Low, E Komisopoulou, SS Chen, L Rubbi and TG Graeber Crump Institute for Molecular Imaging, Institute for Molecular Medicine, Jonsson Comprehensive Cancer Center, California NanoSystems Institute, Department of Molecular and Medical Pharmacology, University of California, Los Angeles, CA, USA BCR-ABL1 is a fusion tyrosine kinase, which causes signaling effects of BCR-ABL1 toward leukemic multiple types of leukemia. We used an integrated transformation. proteomic approach that includes label-free quantitative Oncogene (2010) 29, 5895–5910; doi:10.1038/onc.2010.331; protein complex and phosphorylation profiling by mass published online 9 August 2010 spectrometry to systematically characterize the proximal signaling network of this oncogenic kinase. The proximal Keywords: adaptor protein; BCR-ABL1; phospho- BCR-ABL1 signaling network shows a modular and complex; quantitative mass spectrometry; signaling layered organization with an inner core of three leukemia network; systems biology transformation-relevant adaptor protein complexes (Grb2/Gab2/Shc1 complex, CrkI complex and Dok1/ Dok2 complex). We introduced an ‘interaction direction- ality’ analysis, which annotates static protein networks Introduction with information on the directionality of phosphorylation- dependent interactions. In this analysis, the observed BCR-ABL1 is a constitutively active oncogenic fusion network structure was consistent with a step-wise kinase that arises through a chromosomal translocation phosphorylation-dependent assembly of the Grb2/Gab2/ and causes multiple types of leukemia. It is found in Shc1 and the Dok1/Dok2 complexes on the BCR-ABL1 many cases (B25%) of adult acute lymphoblastic core. -
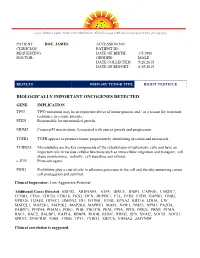
Sample Lab Report
3030 Venture Lane, Suite 108 ● Melbourne, Florida 32934 ● Phone 321-253-5197 ● Fax 321-253-5199 PATIENT: DOE, JAMES ACCESSION NO: CLINICIAN/ PATIENT ID: REQUESTING DATE OF BIRTH: 1/5/1986 DOCTOR: GENDER: MALE DATE COLLECTED: 5/26/2015 DATE OF REPORT: 6/15/2015 RESULTS PRIMARY TUMOR TYPE RIGHT TESTICLE BIOLOGICALLY IMPORTANT ONCOGENES DETECTED GENE IMPLICATION TP53 TP53 mutations may be an important driver of tumorigenesis and / or a reason for treatment resistance in a some patients. PTEN Responsible for uncontrolled growth. MDM2 Causes p53 inactivation. Associated with cancer growth and progression. TGFB1 TGFB appears to promote tumor progession by stimulating invasion and metastasis. TUBB2A Microtubules are the key components of the cytoskeleton of eukaryotic cells and have an important role in various cellular functions such as intracellular migration and transport, cell shape maintenance, polarity, cell signaling and mitosis. c-JUN Proto-oncogene PHB2 Prohibitins play a crucial role in adhesion processes in the cell and thereby sustaining cancer cell propagation and survival. Clinical Impression: Low Aggressive Potential Additional Genes Detected: ABCG2, ARHGAP5, ATF4, BIRC5, BNIP3, CAPNS1, CARD17, CCNB1, CD24, CDC20, CDK18, CKS2, DCN, DEPDC1, FTL, FZD5, FZD9, GAPDH, GNB2, GPR126, H2AFZ, HDAC1, HMGN2, ID1, IFITM1, JUNB, KPNA2, KRT18, LDHA, LTF, MAD2L1, MAP2K1, MAP2K2, MAP2K4, MAPRE1, MAS1, NME1, NME3, NPM1, PA2G4, PABPC1, PFDN4, PGAM1, PGK1, PHB, PIK3CB, PKM, PPIA, PPIH, PRKX, PRNP, PTMA, RAC1, RAC2, RALBP1, RAP1A, RBBP4, RHOB, RHOC, -

Host-Pathogen Systems Biology: Logical Modelling of Hepatocyte
BMC Systems Biology BioMed Central Research article Open Access Host-pathogen systems biology: logical modelling of hepatocyte growth factor and Helicobacter pylori induced c-Met signal transduction Raimo Franke†1, Melanie Müller†1, Nicole Wundrack1, Ernst-Dieter Gilles2, Steffen Klamt2, Thilo Kähne1 and Michael Naumann*1 Address: 1Institute of Experimental Internal Medicine, Otto von Guericke University, Leipziger Str. 44, 39120 Magdeburg, Germany and 2Max Planck Institute for Dynamics of Complex Technical Systems, Sandtorstrasse 1, 39106 Magdeburg, Germany Email: Raimo Franke - [email protected]; Melanie Müller - [email protected]; Nicole Wundrack - [email protected]; Ernst-Dieter Gilles - [email protected]; Steffen Klamt - Klamt@mpi- magdeburg.mpg.de; Thilo Kähne - [email protected]; Michael Naumann* - [email protected] * Corresponding author †Equal contributors Published: 14 January 2008 Received: 3 October 2007 Accepted: 14 January 2008 BMC Systems Biology 2008, 2:4 doi:10.1186/1752-0509-2-4 This article is available from: http://www.biomedcentral.com/1752-0509/2/4 © 2008 Franke et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Abstract Background: The hepatocyte growth factor (HGF) stimulates mitogenesis, motogenesis, and morphogenesis in a wide range of tissues, including epithelial cells, on binding to the receptor tyrosine kinase c-Met. Abnormal c-Met signalling contributes to tumour genesis, in particular to the development of invasive and metastatic phenotypes. -
Conditional Ablation of P130cas/BCAR1 Adaptor Protein
Camacho Leal et al. Cell Communication and Signaling (2018) 16:73 https://doi.org/10.1186/s12964-018-0289-z RESEARCH Open Access Conditional ablation of p130Cas/BCAR1 adaptor protein impairs epidermal homeostasis by altering cell adhesion and differentiation Maria del Pilar Camacho Leal†, Andrea Costamagna†, Beatrice Tassone, Stefania Saoncella, Matilde Simoni, Dora Natalini, Aurora Dadone, Marianna Sciortino, Emilia Turco, Paola Defilippi, Enzo Calautti‡ and Sara Cabodi*‡ Abstract Background: p130 Crk-associated substrate (p130CAS; also known as BCAR1) is a scaffold protein that modulates many essential cellular processes such as cell adhesion, proliferation, survival, cell migration, and intracellular signaling. p130Cas has been shown to be highly expressed in a variety of human cancers of epithelial origin. However, few data are available regarding the role of p130Cas during normal epithelial development and homeostasis. Methods: To this end, we have generated a genetically modified mouse in which p130Cas protein was specifically ablated in the epidermal tissue. Results: By using this murine model, we show that p130Cas loss results in increased cell proliferation and reduction of cell adhesion to extracellular matrix. In addition, epidermal deletion of p130Cas protein leads to premature expression of “late” epidermal differentiation markers, altered membrane E-cadherin/catenin proteins localization and aberrant tyrosine phosphorylation of E-cadherin/catenin complexes. Interestingly, these alterations in adhesive properties in absence -

Expression Profiling of KLF4
Expression Profiling of KLF4 AJCR0000006 Supplemental Data Figure S1. Snapshot of enriched gene sets identified by GSEA in Klf4-null MEFs. Figure S2. Snapshot of enriched gene sets identified by GSEA in wild type MEFs. 98 Am J Cancer Res 2011;1(1):85-97 Table S1: Functional Annotation Clustering of Genes Up-Regulated in Klf4 -Null MEFs ILLUMINA_ID Gene Symbol Gene Name (Description) P -value Fold-Change Cell Cycle 8.00E-03 ILMN_1217331 Mcm6 MINICHROMOSOME MAINTENANCE DEFICIENT 6 40.36 ILMN_2723931 E2f6 E2F TRANSCRIPTION FACTOR 6 26.8 ILMN_2724570 Mapk12 MITOGEN-ACTIVATED PROTEIN KINASE 12 22.19 ILMN_1218470 Cdk2 CYCLIN-DEPENDENT KINASE 2 9.32 ILMN_1234909 Tipin TIMELESS INTERACTING PROTEIN 5.3 ILMN_1212692 Mapk13 SAPK/ERK/KINASE 4 4.96 ILMN_2666690 Cul7 CULLIN 7 2.23 ILMN_2681776 Mapk6 MITOGEN ACTIVATED PROTEIN KINASE 4 2.11 ILMN_2652909 Ddit3 DNA-DAMAGE INDUCIBLE TRANSCRIPT 3 2.07 ILMN_2742152 Gadd45a GROWTH ARREST AND DNA-DAMAGE-INDUCIBLE 45 ALPHA 1.92 ILMN_1212787 Pttg1 PITUITARY TUMOR-TRANSFORMING 1 1.8 ILMN_1216721 Cdk5 CYCLIN-DEPENDENT KINASE 5 1.78 ILMN_1227009 Gas2l1 GROWTH ARREST-SPECIFIC 2 LIKE 1 1.74 ILMN_2663009 Rassf5 RAS ASSOCIATION (RALGDS/AF-6) DOMAIN FAMILY 5 1.64 ILMN_1220454 Anapc13 ANAPHASE PROMOTING COMPLEX SUBUNIT 13 1.61 ILMN_1216213 Incenp INNER CENTROMERE PROTEIN 1.56 ILMN_1256301 Rcc2 REGULATOR OF CHROMOSOME CONDENSATION 2 1.53 Extracellular Matrix 5.80E-06 ILMN_2735184 Col18a1 PROCOLLAGEN, TYPE XVIII, ALPHA 1 51.5 ILMN_1223997 Crtap CARTILAGE ASSOCIATED PROTEIN 32.74 ILMN_2753809 Mmp3 MATRIX METALLOPEPTIDASE -

Breast Cancer Antiestrogen Resistance-3 Expression Regulates Breast Cancer Cell Migration Through Promotion of P130cas Membrane Localization Andmembrane Ruffling
Research Article Breast Cancer Antiestrogen Resistance-3 Expression Regulates Breast Cancer Cell Migration through Promotion of p130Cas Membrane Localization andMembrane Ruffling Randy S. Schrecengost,1 Rebecca B. Riggins,2 Keena S. Thomas,1 Michael S. Guerrero,1 and Amy H. Bouton1 1Department of Microbiology, University of Virginia Health System, Charlottesville, Virginia and 2Department of Oncology, Lombardi Comprehensive Cancer Center, Georgetown University, Washington, District of Columbia Abstract antiestrogen resistance-1 (BCAR1; also known as p130Cas; refs. 2, 3). Antiestrogens such as tamoxifen are widely used in the clinic A second protein, BCAR3 (the human homologue of the murine to treat estrogen receptor–positive breast tumors. Resistance protein AND-34), was identified in a genetic screen along with to tamoxifen can occur either de novo or develop over time in BCAR1 as a gene product whose overexpression conferred tamoxifen resistance in vitro (4). BCAR3 is a member of the novel a large proportion of these tumors. Additionally, resistance is S p associated with enhanced motility and invasiveness in vitro. rc homology 2 (SH2)–containing rotein (NSP) family that One molecule that has been implicated in tamoxifen resis- includes two other members, Chat/SHEP1 and NSP1. These tance, breast cancer antiestrogen resistance-3 (BCAR3), has proteins share a common domain structure consisting of an also been shown to regulate migration of fibroblasts. In this amino-terminal SH2 domain and a carboxyl-terminal domain with study, we investigated the role of BCAR3 in breast cancer cell sequence homology to the Cdc25-family of guanine nucleotide exchange factors (GEF). Several studies have shown that BCAR3 migration and invasion. -

RET Gene Fusions in Malignancies of the Thyroid and Other Tissues
G C A T T A C G G C A T genes Review RET Gene Fusions in Malignancies of the Thyroid and Other Tissues Massimo Santoro 1,*, Marialuisa Moccia 1, Giorgia Federico 1 and Francesca Carlomagno 1,2 1 Department of Molecular Medicine and Medical Biotechnology, University of Naples “Federico II”, 80131 Naples, Italy; [email protected] (M.M.); [email protected] (G.F.); [email protected] (F.C.) 2 Institute of Endocrinology and Experimental Oncology of the CNR, 80131 Naples, Italy * Correspondence: [email protected] Received: 10 March 2020; Accepted: 12 April 2020; Published: 15 April 2020 Abstract: Following the identification of the BCR-ABL1 (Breakpoint Cluster Region-ABelson murine Leukemia) fusion in chronic myelogenous leukemia, gene fusions generating chimeric oncoproteins have been recognized as common genomic structural variations in human malignancies. This is, in particular, a frequent mechanism in the oncogenic conversion of protein kinases. Gene fusion was the first mechanism identified for the oncogenic activation of the receptor tyrosine kinase RET (REarranged during Transfection), initially discovered in papillary thyroid carcinoma (PTC). More recently, the advent of highly sensitive massive parallel (next generation sequencing, NGS) sequencing of tumor DNA or cell-free (cfDNA) circulating tumor DNA, allowed for the detection of RET fusions in many other solid and hematopoietic malignancies. This review summarizes the role of RET fusions in the pathogenesis of human cancer. Keywords: kinase; tyrosine kinase inhibitor; targeted therapy; thyroid cancer 1. The RET Receptor RET (REarranged during Transfection) was initially isolated as a rearranged oncoprotein upon the transfection of a human lymphoma DNA [1]. -

Imatinib Dependent Tyrosine Phosphorylation Profiling of Bcr-Abl
Provided by the author(s) and University College Dublin Library in accordance with publisher policies. Please cite the published version when available. Title Imatinib-dependent tyrosine phosphorylation profiling of Bcr-Abl-positive chronic myeloid leukemia cells Authors(s) Preisinger, C.; Schwarz, J. P.; Bleijerveld, O. B.; et al. Publication date 2012-08-27 Publication information Leukemia, 27 (3): 743-746 Publisher Nature Publishing Group Item record/more information http://hdl.handle.net/10197/5078 Publisher's version (DOI) 10.1038/leu.2012.243 Downloaded 2021-09-25T14:43:28Z The UCD community has made this article openly available. Please share how this access benefits you. Your story matters! (@ucd_oa) © Some rights reserved. For more information, please see the item record link above. 1 Imatinib dependent tyrosine phosphorylation profiling of Bcr-Abl 2 positive chronic myeloid leukemia cells 3 Bcr-Abl is the major cause and pathogenetic principle of chronic myeloid leukemia (CML). 4 Bcr-Abl results from a chromosomal translocation that fuses the bcr and the abl genes, 5 thereby generating a constitutively active tyrosine kinase, which stimulates several signaling 6 networks required for proliferation and survival. Bcr-Abl’s oncogenic properties comprise 7 both functions as a kinase and as a scaffold protein 1. A number of Bcr-Abl interaction 8 partners and downstream effectors have been described, improving our understanding of the 9 signaling networks deranged in CML. Brehme et al. recently defined the “core-interactome of 10 Bcr-Abl”, identifying seven major interaction partners of Bcr-Abl (GRB2, Shc1, Crk, c-Cbl, 11 p85, Sts-1, and SHIP-2) 2. -

Detection of a Rare BCR–ABL Tyrosine Kinase Fusion Protein in H929 Multiple Myeloma Cells Using Immunoprecipitation (IP)-Tandem Mass Spectrometry (MS/MS)
Detection of a rare BCR–ABL tyrosine kinase fusion protein in H929 multiple myeloma cells using immunoprecipitation (IP)-tandem mass spectrometry (MS/MS) Susanne B. Breitkopfa,b, Min Yuana, German A. Pihanc, and John M. Asaraa,b,1 aDivision of Signal Transduction, Beth Israel Deaconess Medical Center, Boston, MA 02115; bDepartment of Medicine, Harvard Medical School, Boston, MA 02115; and cDepartment of Hematopathology, Beth Israel Deaconess Medical Center, Boston, MA 02115 Edited by Peter K. Vogt, The Scripps Research Institute, La Jolla, CA, and approved August 23, 2012 (received for review July 26, 2012) Hypothesis directed proteomics offers higher throughput over Here, we focused on a hypothesis-directed approach to identify global analyses. We show that immunoprecipitation (IP)–tandem the active signaling pathways that drive cancers. To this end, we mass spectrometry (LC-MS/MS) in H929 multiple myeloma (MM) immunoprecipitated proteins that have clinical significance in cell cancer cells led to the discovery of a rare and unexpected BCR– proliferation such as the central nodes in the AKT and ERK sig- ABL fusion, informing a therapeutic intervention using imatinib naling pathways. The p85 regulatory subunit of phosphoinositide- (Gleevec). BCR–ABL is the driving mutation in chronic myeloid leu- 3-kinase (PI3K) binds pYXXM motif-containing proteins to the kemia (CML) and is uncommon to other cancers. Three different IP– SRC homology 2 (SH2) domains of p85, thus recruiting the p110 MS experiments central to cell signaling pathways were sufficient to catalytic subunit to the plasma membrane for activation (5, 17). Activated p110 phosphorylates its lipid substrate phosphatidyli- discover a BCR–ABL fusion in H929 cells: phosphotyrosine (pY) pep- nositol-4,5-bisphosphate (PIP2) to phosphatidylinositol-3,4,5-tri- tide IP, p85 regulatory subunit of phosphoinositide-3-kinase (PI3K) phosphate (PIP3) and binds to the pleckstrin homology (PH) IP, and the GRB2 adaptor IP. -

High BCAR1 Expression Is Associated with Early PSA Recurrence in ERG Negative Prostate Cancer Asmus Heumann1†, Nina Heinemann1†, Claudia Hube-Magg1, Dagmar S
Heumann et al. BMC Cancer (2018) 18:37 DOI 10.1186/s12885-017-3956-3 RESEARCHARTICLE Open Access High BCAR1 expression is associated with early PSA recurrence in ERG negative prostate cancer Asmus Heumann1†, Nina Heinemann1†, Claudia Hube-Magg1, Dagmar S. Lang1, Katharina Grupp2, Martina Kluth1, Sarah Minner1, Christina Möller-Koop1,MarkusGraefen3, Hans Heinzer3, Maria Christina Tsourlakis1, Waldemar Wilczak1, Corinna Wittmer1,FrankJacobsen1,HartwigHuland3, Ronald Simon1* ,ThorstenSchlomm3,4, Guido Sauter1, Stefan Steurer1,PatrickLebok1 and Andrea Hinsch1 Abstract Background: Breast cancer anti-estrogen resistance 1 (BCAR1/p130cas) is a hub for diverse oncogenic signaling cascades and promotes tumor development and progression. Methods: To understand the effect of BCAR1 in prostate cancer, we analyzed its expression on more than 11,000 prostate cancer samples. BCAR1 expression levels were compared with clinical characteristics, PSA recurrence, molecular subtype defined by ERG status and 3p, 5q, 6q and PTEN deletion. Results: BCAR1 staining was barely detectable in normal prostate glands but seen in 77.6% of 9472 interpretable cancers, including strong expression in 38.5%, moderate in 23.2% and weak in 15.9% of cases. BCAR1 up regulation was associated with positive ERG status (p < 0.0001), high Gleason score (p < 0.0001), advanced pathological tumor stage (p = 0.0082), lower preoperative PSA level (p < 0.0001), increased cell proliferation (p < 0.0001), early PSA recurrence (p = 0.0008), and predicted prognosis independently from clinico-pathological parameters available at the time of the initial biopsy. However, subset analyses revealed that the prognostic impact of BCAR1 expression was limited to ERG-negative cancer. That BCAR1 up regulation was linked to almost all analyzed deletions (p < 0.0001 each for PTEN, 5q, 6q deletion) may suggest a functional link to genomic instability. -

Ephrin-B1 Forward Signaling Regulates Craniofacial Morphogenesis by Controlling Cell Proliferation Across Eph–Ephrin Boundaries
Downloaded from genesdev.cshlp.org on September 28, 2021 - Published by Cold Spring Harbor Laboratory Press Ephrin-B1 forward signaling regulates craniofacial morphogenesis by controlling cell proliferation across Eph–ephrin boundaries Jeffrey O. Bush1 and Philippe Soriano1,2 Program in Developmental Biology and Division of Basic Sciences, Fred Hutchinson Cancer Research Center, Seattle, Washington 98109, USA; and Department of Developmental and Regenerative Biology, Mt. Sinai School of Medicine, New York, New York 10029, USA Mutations in the X-linked human EPHRIN-B1 gene result in cleft palate and other craniofacial anomalies as part of craniofrontonasal syndrome (CFNS), but the molecular and developmental mechanisms by which ephrin-B1 controls the underlying developmental processes are not clear. Here we demonstrate that ephrin-B1 plays an intrinsic role in palatal shelf outgrowth in the mouse by regulating cell proliferation in the anterior palatal shelf mesenchyme. In ephrin-B1 heterozygous mutants, X inactivation generates ephrin-B1-expressing and -nonex- pressing cells that sort out, resulting in mosaic ephrin-B1 expression. We now show that this process leads to mosaic disruption of cell proliferation and post-transcriptional up-regulation of EphB receptor expression through relief of endocytosis and degradation. The alteration in proliferation rates resulting from ectopic Eph–ephrin expression boundaries correlates with the more severe dysmorphogenesis of ephrin-B1+/À heterozygotes that is a hallmark of CFNS. Finally, by integrating phosphoproteomic and transcriptomic approaches, we show that ephrin-B1 controls proliferation in the palate by regulating the extracellular signal-regulated kinase/mitogen- activated protein kinase (ERK/MAPK) signal transduction pathway. [Keywords: Ephrin; cell proliferation; ERK/MAPK; endocytosis; boundaries; craniofrontonasal syndrome; palate] Supplemental material is available at http://www.genesdev.org. -

Has Programmed Cell Death Ligand-1 MET an Accomplice in Non-Small Cell Lung Cancer?—A Narrative Review
2682 Review Article Has programmed cell death ligand-1 MET an accomplice in non-small cell lung cancer?—a narrative review Wolfram C. M. Dempke1, Klaus Fenchel2 1Department of Haematology and Oncology, University of Munich, Munich, Germany; 2Medical Oncology Clinic, Saalfeld, Germany Contributions: (I) Conception and design: Both authors; (II) Administrative support: None; (III) Provision of study materials or patients: None; (IV) Collection and assembly of data: Both authors; (V) Data analysis and interpretation: Both authors; (VI) Manuscript writing: Both authors; (VII) Final approval of manuscript: Both authors. Correspondence to: Wolfram C. M. Dempke, MD, PhD, MBA. Department of Haematology and Oncology, Medical Clinic III (Campus Grosshadern), Marchinoninistr. 15, D-81377 Munich, Germany. Email: [email protected]. Abstract: Recently approved and highly specific small-molecule inhibitors of c-MET exon 14 skipping mutations (e.g., capmatinib, tepotinib) are a new and important therapeutic option for the treatment of non- small cell lung cancer (NSCLC) patients harbouring c-MET alterations. Several experimental studies have provided compelling evidence that c-MET is involved in the regulation of the immune response by up- regulating inhibitory molecules (e.g., PD-L1) and down-regulating of immune stimulators (e.g., CD137, CD252, CD70, etc.). In addition, c-MET was found to be implicated in the regulation of the inflamed tumour microenvironment (TME) and thereby contributing to an increased immune escape of tumour cells from T cell killing. Moreover, it is a major resistance mechanism following treatment of epidermal growth factor receptor mutations (EGFRmut) with tyrosine kinase receptor inhibitors (TKIs). In line with these findings c-MET alterations have also been shown to be associated with a worse clinical outcome and a poorer prognosis in NSCLC patients.