Comparison with Its Mediastinal Component and Myeloid Sarcoma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Network Scan Data
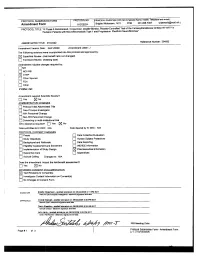
CTEP Protocol No: T-99-0090 CC Protocol No: 01-C-0222 Amendment: J Revised: 4/21/09 IRB Approval Date: A Phase II Randomized, Cross-Over, Double-Blinded, Placebo-Controlled Trial of the Farnesyltransferase Inhibitor R115777 in Pediatric Patients with Neurofibromatosis Type 1 and Progressive Plexiform Neurofibromas Coordinating Center: Pediatric Oncology Branch, NCI Principal Investigator: Brigitte Widemann, M.D.* (POB, NCI) NIH Associate Investigators: Frank M. Balis, M.D. (POB, NCI) Beth Fox, M.D. (POB, NCI) Kathy Warren, M.D. (NOB, NCI) Andy Gillespie, R.N. (ND, CC) Eva Dombi, MD (POB, NCI)** Nalini Jayaprakash, (POB, NCI) Diane Cole, (POB, NCI) Seth Steinberg, Ph.D. (BDMB, DCS, NCI) Nicholas Patronas, M.D. (DR, CC)** Maria Tsokos, M.D., (Laboratory of Pathology, NCI)** Pamela Wolters, Ph.D. (HAMB, NCI) Staci Martin, Ph.D. (HAMB, NCI) Jeffrey Solomon, (NIH and Sensor Systems, Inc.) Non-NIH Associate Investigators: Wanda Salzer, M.D. ** Keesler Air Force Base, Biloxi, Mississippi) 81st MDOS/SGOC 301 Fisher Street, Room 1A132 Keesler AFB, MS 39534-2519 Phone: 228-377-6524 E-mail: [email protected] Bruce R. Korf, M.D., Ph.D. ** Chair, Department of Genetics Univeristy of Alabama at Birmingham 1530 3rd Ave. S. Birmingham, AL 35294 Phone: (205)-934-9411, Fax: (205)-934-9488 E-mail: [email protected] David H. Gutmann, M.D., Ph.D. ** Department of Neurology Washington University School of Medicine St. Louis Children’s Hospital Box 8111, 660 S. Euclid Avenue St. Louis, MO 63110 Phone: (314)-632-7149, Fax: (314)-362-9462 E-mail: [email protected] 1 4/21/2009 T-99-0090, 01-C-0222 Arie Perry, M.D. -

Photodermatoses Update Knowledge and Treatment of Photodermatoses Discuss Vitamin D Levels in Photodermatoses
Ashley Feneran, DO Jenifer Lloyd, DO University Hospitals Regional Hospitals AMERICAN OSTEOPATHIC COLLEGE OF DERMATOLOGY Objectives Review key points of several photodermatoses Update knowledge and treatment of photodermatoses Discuss vitamin D levels in photodermatoses Types of photodermatoses Immunologically mediated disorders Defective DNA repair disorders Photoaggravated dermatoses Chemical- and drug-induced photosensitivity Types of photodermatoses Immunologically mediated disorders Polymorphous light eruption Actinic prurigo Hydroa vacciniforme Chronic actinic dermatitis Solar urticaria Polymorphous light eruption (PMLE) Most common form of idiopathic photodermatitis Possibly due to delayed-type hypersensitivity reaction to an endogenous cutaneous photo- induced antigen Presents within minutes to hours of UV exposure and lasts several days Pathology Superficial and deep lymphocytic infiltrate Marked papillary dermal edema PMLE Treatment Topical or oral corticosteroids High SPF Restriction of UV exposure Hardening – natural, NBUVB, PUVA Antimalarial PMLE updates Study suggests topical vitamin D analogue used prophylactically may provide therapeutic benefit in PMLE Gruber-Wackernagel A, Bambach FJ, Legat A, et al. Br J Dermatol, 2011. PMLE updates Study seeks to further elucidate the pathogenesis of PMLE Found a decrease in Langerhans cells and an increase in mast cell density in lesional skin Wolf P, Gruber-Wackernagel A, Bambach I, et al. Exp Dermatol, 2014. Actinic prurigo Similar to PMLE Common in native -

Depo-Provera
PRODUCT MONOGRAPH INCLUDING PATIENT MEDICATION INFORMATION PR ® DEPO-PROVERA medroxyprogesterone acetate injectable suspension, USP Sterile Aqueous Suspension 50 mg/mL and 150 mg/mL Progestogen Pfizer Canada Inc. Date of Revision: 17,300 Trans-Canada Highway February 13, 2018 Kirkland, Quebec H9J 2M5 Submission Control No: 210121 ® Pharmacia & Upjohn Company LLC Pfizer Canada Inc., Licensee © Pfizer Canada Inc., 2018 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION......................................................... 3 SUMMARY PRODUCT INFORMATION ........................................................................ 3 INDICATIONS AND CLINICAL USE .............................................................................. 3 CONTRAINDICATIONS ................................................................................................... 4 WARNINGS AND PRECAUTIONS: ................................................................................ 5 ADVERSE REACTIONS ................................................................................................. 18 DRUG INTERACTIONS .................................................................................................. 27 DOSAGE AND ADMINISTRATION .............................................................................. 28 OVERDOSAGE ................................................................................................................ 30 ACTION AND CLINICAL PHARMACOLOGY ............................................................ 30 STORAGE AND -

Various Clinical and Histopathological Patterns of Idiopathic Photodermatosis: an Observational Study
Review Article Clinician’s corner Images in Medicine Experimental Research Case Report Miscellaneous Letter to Editor DOI: 10.7860/JCDR/2018/28950.12274 Original Article Postgraduate Education Various Clinical and Histopathological Case Series Patterns of Idiopathic Photodermatosis: Dermatology Section An Observational Study Short Communication DIMPLE CHOPRA1, RAVINDER SINGH2, RK BAHL3, RAMESH KUMAR KUNDAL4, SHIVALI AGGARWAL5, AASTHA SHARMA6, AANCHAL SINGLA7 ABSTRACT presented in the age group of 56-70 years. Total 95% cases Introduction: The idiopathic photodermatosis have different had lesions on photoexposed parts of upper limbs followed by histopathological patterns, spongiotic pattern being the most neck involvement in 51% cases. The most common presenting common. symptom was itching, seen in 98% patients. Polymorphic Light Eruption (PMLE) was the clinical diagnosis in 97% cases. Aim: To study the histopathological patterns of photodermatosis The most common histopathological pattern observed was and to correlate between the clinical and histopathological Spongiotic pattern which was seen in 46% cases. findings. Conclusion: While young females in the age group 26-40 year Materials and Methods: Hundered consecutive patients with were more commonly affected, lesions were more common lesions of idiopathic photodermatosis were included in this in men who were in the age group 56-70 year. Population in cross-sectional observational study. The clinical diagnosis was North India may be at greater risk because their skin is suddenly made and confirmed after thorough history, clinical examination exposed to sun in spring and summer after the end of winter and relevant investigations, including biopsy. season. The PMLE was the most common subtype. Spongiotic Results: In this study 49 participants were male and 51 were pattern was the most common histopathological pattern found, female. -

Case Reports Article – Rapidly Growing Mass in the Ear Canal: A
Arepen et al. (2020): Rapidly growing mass in the ear canal May 2020 Vol. 23 Issue 8 Case reports article – Rapidly growing mass in the ear canal: A rare case of isolated superficial angiomyxoma Siti Asmat Md Arepen1,2, Nor Eyzawiah Hassan1,2, Azlina Abd Rani1, Shahrul Hitam2 Mohd Khairi Md Daud3 1Faculty of Medicine & Health Sciences,Universiti Sains Islam Malaysia, Selangor, Malaysia. 2Department of Otorhinolaryngology Head & Neck Surgery, Hospital Ampang, Selangor, Malaysia. 3Department of Otorhinolaryngology Head & Neck Surgery, Faculty of Medicine & Health Sciences, Universiti Sains Malaysia, Kelantan, Malaysia. Corresponding author: Nor Eyzawiah Hassan ([email protected]) Abstract: Superficial angiomyxoma is a rare benign skin tumour and usually present as an asymptomatic lesion. It is known to be highly recurrent and complete wide excision is the best treatment. This cace reported of 56 yr old gentleman presented with fleshy, pink coloured right external auditory mass. The mass arisen from the posterior wall of the canal at the bony–cartilaginous junction. Clinical diagnosis of an anaural polyp was made and the mass was excised. However, it rapidly recurred bigger than its actual size within a week. The histopathological examination was reported as superficial angiomyxoma. A differential diagnosis of isolated superficial angiomyxoma should be considered in the case of external auditory canal mass and Carney complex needs to be considered. Complete excision and regular follow up is recommended. Keywords: Benign tumour, external auditory canal, myxoma How to cite this article: How to cite this article: Arepen et al. (2020): Case reports article – Rapidly growing mass in the ear canal: A rare case of isolated superficial angiomyxoma, Ann Trop & Public Health, 23 (S8): 1279–1282. -

Cutaneous Neurofibromas: Clinical Definitions Current Treatment Is Limited to Surgical Removal Or Physical Or Descriptors Destruction
ARTICLE OPEN ACCESS Cutaneous neurofibromas Current clinical and pathologic issues Nicolas Ortonne, MD, PhD,* Pierre Wolkenstein, MD, PhD,* Jaishri O. Blakeley, MD, Bruce Korf, MD, PhD, Correspondence Scott R. Plotkin, MD, PhD, Vincent M. Riccardi, MD, MBA, Douglas C. Miller, MD, PhD, Susan Huson, MD, Dr. Wolkenstein Juha Peltonen, MD, PhD, Andrew Rosenberg, MD, Steven L. Carroll, MD, PhD, Sharad K. Verma, PhD, [email protected] Victor Mautner, MD, Meena Upadhyaya, PhD, and Anat Stemmer-Rachamimov, MD Neurology® 2018;91 (Suppl 1):S5-S13. doi:10.1212/WNL.0000000000005792 Abstract RELATED ARTICLES Objective Creating a comprehensive To present the current terminology and natural history of neurofibromatosis 1 (NF1) cuta- research strategy for neous neurofibromas (cNF). cutaneous neurofibromas Page S1 Methods NF1 experts from various research and clinical backgrounds reviewed the terms currently in use The biology of cutaneous fi for cNF as well as the clinical, histologic, and radiographic features of these tumors using neuro bromas: Consensus published and unpublished data. recommendations for setting research priorities Results Page S14 Neurofibromas develop within nerves, soft tissue, and skin. The primary distinction between fi fi Considerations for cNF and other neuro bromas is that cNF are limited to the skin whereas other neuro bromas development of therapies may involve the skin, but are not limited to the skin. There are important cellular, molecular, for cutaneous histologic, and clinical features of cNF. Each of these factors is discussed in consideration of neurofibroma a clinicopathologic framework for cNF. Page S21 Conclusion Clinical trial design for The development of effective therapies for cNF requires formulation of diagnostic criteria that cutaneous neurofibromas encompass the clinical and histologic features of these tumors. -

Dermatopathology
Dermatopathology Clay Cockerell • Martin C. Mihm Jr. • Brian J. Hall Cary Chisholm • Chad Jessup • Margaret Merola With contributions from: Jerad M. Gardner • Talley Whang Dermatopathology Clinicopathological Correlations Clay Cockerell Cary Chisholm Department of Dermatology Department of Pathology and Dermatopathology University of Texas Southwestern Medical Center Central Texas Pathology Laboratory Dallas , TX Waco , TX USA USA Martin C. Mihm Jr. Chad Jessup Department of Dermatology Department of Dermatology Brigham and Women’s Hospital Tufts Medical Center Boston , MA Boston , MA USA USA Brian J. Hall Margaret Merola Department of Dermatology Department of Pathology University of Texas Southwestern Medical Center Brigham and Women’s Hospital Dallas , TX Boston , MA USA USA With contributions from: Jerad M. Gardner Talley Whang Department of Pathology and Dermatology Harvard Vanguard Medical Associates University of Arkansas for Medical Sciences Boston, MA Little Rock, AR USA USA ISBN 978-1-4471-5447-1 ISBN 978-1-4471-5448-8 (eBook) DOI 10.1007/978-1-4471-5448-8 Springer London Heidelberg New York Dordrecht Library of Congress Control Number: 2013956345 © Springer-Verlag London 2014 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifi cally the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfi lms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. Exempted from this legal reservation are brief excerpts in connection with reviews or scholarly analysis or material supplied specifi cally for the purpose of being entered and executed on a computer system, for exclusive use by the purchaser of the work. -

2016 Essentials of Dermatopathology Slide Library Handout Book
2016 Essentials of Dermatopathology Slide Library Handout Book April 8-10, 2016 JW Marriott Houston Downtown Houston, TX USA CASE #01 -- SLIDE #01 Diagnosis: Nodular fasciitis Case Summary: 12 year old male with a rapidly growing temple mass. Present for 4 weeks. Nodular fasciitis is a self-limited pseudosarcomatous proliferation that may cause clinical alarm due to its rapid growth. It is most common in young adults but occurs across a wide age range. This lesion is typically 3-5 cm and composed of bland fibroblasts and myofibroblasts without significant cytologic atypia arranged in a loose storiform pattern with areas of extravasated red blood cells. Mitoses may be numerous, but atypical mitotic figures are absent. Nodular fasciitis is a benign process, and recurrence is very rare (1%). Recent work has shown that the MYH9-USP6 gene fusion is present in approximately 90% of cases, and molecular techniques to show USP6 gene rearrangement may be a helpful ancillary tool in difficult cases or on small biopsy samples. Weiss SW, Goldblum JR. Enzinger and Weiss’s Soft Tissue Tumors, 5th edition. Mosby Elsevier. 2008. Erickson-Johnson MR, Chou MM, Evers BR, Roth CW, Seys AR, Jin L, Ye Y, Lau AW, Wang X, Oliveira AM. Nodular fasciitis: a novel model of transient neoplasia induced by MYH9-USP6 gene fusion. Lab Invest. 2011 Oct;91(10):1427-33. Amary MF, Ye H, Berisha F, Tirabosco R, Presneau N, Flanagan AM. Detection of USP6 gene rearrangement in nodular fasciitis: an important diagnostic tool. Virchows Arch. 2013 Jul;463(1):97-8. CONTRIBUTED BY KAREN FRITCHIE, MD 1 CASE #02 -- SLIDE #02 Diagnosis: Cellular fibrous histiocytoma Case Summary: 12 year old female with wrist mass. -

9Th Clinical Dermatology Congress Psoriasis, Psoriatic Arthritis & Skin
conferenceseries.com Joint Conference Mi Hye Lee et al., J Clin Exp Dermatol Res 2017, 8:6 (Suppl) DOI: 10.4172/2155-9554-C1-066 9th Clinical Dermatology Congress & 2nd International Conference on Psoriasis, Psoriatic arthritis & Skin infections October 16-18, 2017 New York, USA Nonsurgical treatment using micro-insulated needle on neurofibroma Mi Hye Lee, Hak Tae Kim, Woo Jin Lee, Chong Hyun Won, Sung Eun Chang, Mi Woo Lee and Jee Ho Choi University of Ulsan, Korea any studies have investigated the application of micro-insulated needles with radiofrequency (RF) for acne treatment or skin Mrejuvenation. However, there is no study investigating the effects of using micro-insulated needles with RF to treat multiple neurofibroma (NF) lesions. Many patients with multiple neurofibromas usually hesitate to remove all the lesions surgically due to cosmetic concerns. The aim of this study was to evaluate the clinicopathologic outcome, including efficacy and side effects after treatment, using newly developed micro-insulated needles with RF treatment. In this study, two human volunteers received multiple sessions of the micro-insulated needle RF treatment to multiple lesions. Seven to 40 shots were performed on each lesion. The treatment settings were as follows: microneedle penetrating depth of 5.0 mm; insulated 1.0 mm; power 16~46 (level 12~25); and a RF exposure time of 180~400 milliseconds. Skin biopsies were performed before and after the treatment. Outcome assessments included standardized photography, objective measurements of lesion size, histopathologic comparison between before and after the treatment, a physician’s global assessment, and patient satisfaction scores. RF energy could be delivered to the lesions without epidermal damage because the micro-insulation on the needle protects the epidermis from skin burns. -

Clinical Guideline Treatment and Removal of Benign Skin Lesions
Clinical Guideline Guideline Number: CG015, Ver. 5 Treatment and Removal of Benign Skin Lesions Disclaimer Clinical guidelines are developed and adopted to establish evidence-based clinical criteria for utilization management decisions. Oscar may delegate utilization management decisions of certain services to third-party delegates, who may develop and adopt their own clinical criteria. Clinical guidelines are applicable to certain plans. Clinical guidelines are applicable to members enrolled in Medicare Advantage plans only if there are no criteria established for the specified service in a Centers for Medicare & Medicaid Services (CMS) national coverage determination (NCD) or local coverage determination (LCD) on the date of a prior authorization request. Services are subject to the terms, conditions, limitations of a member’s policy and applicable state and federal law. Please reference the member’s policy documents (e.g., Certificate/Evidence of Coverage, Schedule of Benefits) or contact Oscar at 855-672-2755 to confirm coverage and benefit conditions. Summary The integumentary system is comprised of the skin, hair, and nails. The skin is divided into two layers: the dermis and epidermis; diseases of these protective outer layers are among the most common conditions worldwide. Lesions of the skin can be either benign (non-malignant), pre-malignant (potential for evolving into malignancy), or malignant (cancerous). Such lesions arise from congenital malformations or are acquired, often due to extensive UV exposure or underlying illness. Diagnosis is primarily through history, clinical exam, and the appearance of the lesion(s). While the vast majority of benign lesions require no intervention, some cases may necessitate intervention due to bothersome symptoms, for definitive diagnosis, or for exclusion of malignant features. -

Supermicar Data Entry Instructions, 2007 363 Pp. Pdf Icon[PDF
SUPERMICAR TABLE OF CONTENTS Chapter I - Introduction to SuperMICAR ........................................... 1 A. History and Background .............................................. 1 Chapter II – The Death Certificate ..................................................... 3 Exercise 1 – Reading Death Certificate ........................... 7 Chapter III Basic Data Entry Instructions ....................................... 12 A. Creating a SuperMICAR File ....................................... 14 B. Entering and Saving Certificate Data........................... 18 C. Adding Certificates using SuperMICAR....................... 19 1. Opening a file........................................................ 19 2. Certificate.............................................................. 19 3. Sex........................................................................ 20 4. Date of Death........................................................ 20 5. Age: Number of Units ........................................... 20 6. Age: Unit............................................................... 20 7. Part I, Cause of Death .......................................... 21 8. Duration ................................................................ 22 9. Part II, Cause of Death ......................................... 22 10. Was Autopsy Performed....................................... 23 11. Were Autopsy Findings Available ......................... 23 12. Tobacco................................................................ 24 13. Pregnancy............................................................ -

Cd34positive Superficial Myxofibrosarcoma
J Cutan Pathol 2013: 40: 639–645 © 2013 John Wiley & Sons A/S. doi: 10.1111/cup.12158 Published by John Wiley & Sons Ltd John Wiley & Sons. Printed in Singapore Journal of Cutaneous Pathology CD34-positive superficial myxofibrosarcoma: a potential diagnostic pitfall§ Background: Myxofibrosarcoma (MFS) arises most commonly in the Steven C. Smith1,†,AnnA. proximal extremities of the elderly, where it may involve subcutaneous Poznanski1,†,§, Douglas R. and dermal tissues and masquerade as benign entities in limited biopsy Fullen1,2, Linglei Ma3, samples. We encountered such a case, in which positivity for CD34 and Jonathan B. McHugh1,DavidR. morphologic features were initially wrongly interpreted as a Lucas1 and Rajiv M. Patel1,2 ‘low-fat/fat-free’ spindle cell/pleomorphic lipoma. Case series have not 1 assessed prevalence of CD34 reactivity among cutaneous examples of Department of Pathology, University of Michigan, Ann Arbor, MI, USA, MFS. 2Department of Dermatology, University of Methods: We performed a systematic review of our institution’s Michigan, Ann Arbor, MI, USA, and experience, selecting from among unequivocal MFS resection 3Miraca Life Sciences, Glen Burnie, MD, USA specimens those superficial cases in which a limited biopsy sample §This project was presented orally as a proffered might prove difficult to interpret. These cases were immunostained for paper at the United States and Canadian Academy CD34 and tabulated for clinicopathologic characteristics. of Pathology Annual Meeting in Baltimore, MD, = March 2013. Results: After review of all MFS diagnoses over 5 years (n 56), we †Both the authors contributed equally to this work. identified a study group of superficial MFS for comparison to the index ‡Present address: Department of Biomedical case (total n = 8).