Cd34+ Stromal Cells/Telocytes in Normal and Pathological Skin
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Telocytes - Stem Cells
INTERNATIONAL JOURNAL OF BIOLOGY AND BIOMEDICAL ENGINEERING The Tandem: Telocytes - Stem Cells Lawrence M. Popescu Abstract - We have recently described a novel type of inter- II. TeloCyTeS and/oR fIbRoblaSTS ? stitial (stromal) cells – Telocytes (TC) – in several cavitary The interstitium (stroma) is in most of the cases seen as a and non-cavitary organs from humans and other mammalians. connecting “device” for the specific structures of an organ. TC have a small cell body, but specific (unique) prolongations Usually, people are perceiving interstitial cells as being that we named Telopodes (Tp). Therefore, the simplest defi- mainly (or even, only) fibroblasts. However, fibroblasts have nition for TC is: cells with Tp. Tp are characterized by: a) the function of generating connective tissue matrix, specifi- number (1-5/cell, frequently 2 or 3); b) length (tens up to hun- cally, collagen. The distinction between TC and fibroblasts dreds of mm); c) moniliform aspect – an alternation of thin is obvious since they have different ultrastructure and phe- segments, podomeres (with caliber under 200 nm, below the notype. Therefore, their functions should be mostly different: resolving power of light microscopy) and dilated segments, TC - intercellular signalling (connections), but fibroblasts - podoms, which accommodate mitochondria, (rough) endo- collagen synthesis. In other words, TC are “more” function- 2+ plasmic-reticulum and caveolae, the so-called “Ca uptake/ ally oriented, and fibroblasts are “more” structuraly oriented, release units”; d) dichotomous branching pattern forming a responsible for fibrosis. 3D network, a labyrinthine system with complex homo- and There are some clear ultrastructural features that differ- heterocellular junctions, revealed only by electron tomogra- entiate TC from fibroblasts. -
Network Scan Data
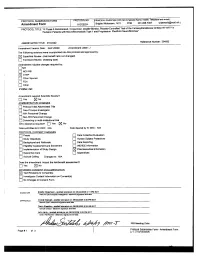
CTEP Protocol No: T-99-0090 CC Protocol No: 01-C-0222 Amendment: J Revised: 4/21/09 IRB Approval Date: A Phase II Randomized, Cross-Over, Double-Blinded, Placebo-Controlled Trial of the Farnesyltransferase Inhibitor R115777 in Pediatric Patients with Neurofibromatosis Type 1 and Progressive Plexiform Neurofibromas Coordinating Center: Pediatric Oncology Branch, NCI Principal Investigator: Brigitte Widemann, M.D.* (POB, NCI) NIH Associate Investigators: Frank M. Balis, M.D. (POB, NCI) Beth Fox, M.D. (POB, NCI) Kathy Warren, M.D. (NOB, NCI) Andy Gillespie, R.N. (ND, CC) Eva Dombi, MD (POB, NCI)** Nalini Jayaprakash, (POB, NCI) Diane Cole, (POB, NCI) Seth Steinberg, Ph.D. (BDMB, DCS, NCI) Nicholas Patronas, M.D. (DR, CC)** Maria Tsokos, M.D., (Laboratory of Pathology, NCI)** Pamela Wolters, Ph.D. (HAMB, NCI) Staci Martin, Ph.D. (HAMB, NCI) Jeffrey Solomon, (NIH and Sensor Systems, Inc.) Non-NIH Associate Investigators: Wanda Salzer, M.D. ** Keesler Air Force Base, Biloxi, Mississippi) 81st MDOS/SGOC 301 Fisher Street, Room 1A132 Keesler AFB, MS 39534-2519 Phone: 228-377-6524 E-mail: [email protected] Bruce R. Korf, M.D., Ph.D. ** Chair, Department of Genetics Univeristy of Alabama at Birmingham 1530 3rd Ave. S. Birmingham, AL 35294 Phone: (205)-934-9411, Fax: (205)-934-9488 E-mail: [email protected] David H. Gutmann, M.D., Ph.D. ** Department of Neurology Washington University School of Medicine St. Louis Children’s Hospital Box 8111, 660 S. Euclid Avenue St. Louis, MO 63110 Phone: (314)-632-7149, Fax: (314)-362-9462 E-mail: [email protected] 1 4/21/2009 T-99-0090, 01-C-0222 Arie Perry, M.D. -

Ultrastructural Identification of Telocytes in the Muscularis of Chicken Ileum
EXPERIMENTAL AND THERAPEUTIC MEDICINE 10: 2325-2330, 2015 Ultrastructural identification of telocytes in the muscularis of chicken ileum PING YANG, YA'AN LIU, NISAR AHMED, SHAKEEB ULLAH, YI LIU and QIUSHENG CHEN Key Laboratory of Animal Physiology and Biochemistry, Ministry of Agriculture, College of Veterinary Medicine, Nanjing Agricultural University, Nanjing, Jiangsu 210095, P.R. China Received November 13, 2014; Accepted September 24, 2015 DOI: 10.3892/etm.2015.2841 Abstract. Telocytes (TCs) are a specialized type of intersti- waves, a basal electrical rhythm leading to contraction of the tial cells, characterized by a small cell body and long, thin smooth muscle (1‑3). In the last decade, ICCs were investigated processes, that have recently been identified in various cavitary from a number of aspects, including ultrastructure, immuno- and non‑cavitary organs of humans and laboratory mammals. reactivity, electrophysiology and pathology (4‑6). In a 2008 Chickens present significant economical and scientific nota- study (7), the intestinal wall cell population was re‑examined; bility; however, ultrastructural identification of TCs remains consequently, a novel cell type was observed by transmission unclear in birds. The aim of the present study was to describe electron microscopy (TEM) and immunohistochemistry. This electron microscopic evidence for the presence of TCs in novel type of interstitial cell, previously known as interstitial the chicken gut. The ileum of healthy adult broiler chickens Cajal-like cells (ICLCs), are now established to be telocytes (n=10) was studied by transmission electron microscopy. TCs (TCs) (8). Characteristics of TCs include long, projected are characterized by several, long (tens to hundreds of µm) prolongations termed telopodes (Tps) measuring tens to prolongations called telopodes (Tps). -

Depo-Provera
PRODUCT MONOGRAPH INCLUDING PATIENT MEDICATION INFORMATION PR ® DEPO-PROVERA medroxyprogesterone acetate injectable suspension, USP Sterile Aqueous Suspension 50 mg/mL and 150 mg/mL Progestogen Pfizer Canada Inc. Date of Revision: 17,300 Trans-Canada Highway February 13, 2018 Kirkland, Quebec H9J 2M5 Submission Control No: 210121 ® Pharmacia & Upjohn Company LLC Pfizer Canada Inc., Licensee © Pfizer Canada Inc., 2018 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION......................................................... 3 SUMMARY PRODUCT INFORMATION ........................................................................ 3 INDICATIONS AND CLINICAL USE .............................................................................. 3 CONTRAINDICATIONS ................................................................................................... 4 WARNINGS AND PRECAUTIONS: ................................................................................ 5 ADVERSE REACTIONS ................................................................................................. 18 DRUG INTERACTIONS .................................................................................................. 27 DOSAGE AND ADMINISTRATION .............................................................................. 28 OVERDOSAGE ................................................................................................................ 30 ACTION AND CLINICAL PHARMACOLOGY ............................................................ 30 STORAGE AND -

Identification and Characterization of Telocytes in the Uterus of the Oviduct
J. Cell. Mol. Med. Vol 18, No 12, 2014 pp. 2385-2392 Identification and characterization of telocytes in the uterus of the oviduct in the Chinese soft-shelled turtle, Pelodiscus sinensis: TEM evidence Shakeeb Ullah #, Ping Yang #, Linli Zhang, Qian Zhang, Yi Liu, Wei Chen, Yasir Waqas, Yuan Le, Bing Chen, Qiusheng Chen * Key Laboratory of Animal Physiology and Biochemistry, Ministry of Agriculture, College of Veterinary Medicine, Nanjing Agricultural University, Nanjing, China Received: April 12, 2014; Accepted: July 16, 2014 Abstract Telocytes (Tcs) are cells with telopodes (Tps), which are very long cellular extensions with alternating thin segments (podomers) and dilated bead-like thick regions known as podoms. Tcs are a distinct category of interstitial cells and have been identified in many mammalian organs including heart, lung and kidney. The present study investigates the existence, ultrastructure, distribution and contacts of Tcs with surrounding cells in the uterus (shell gland) of the oviduct of the Chinese soft-shelled turtle, Pelodiscus sinensis. Samples from the uterine segment of the oviduct were examined by transmission electron microscopy. Tcs were mainly located in the lamina propria beneath the simple columnar epithelium of the uterus and were situated close to nerve endings, capillaries, collagen fibres and secretory glands. The complete morphology of Tcs and Tps was clearly observed and our data confirmed the existence of Tcs in the uterus of the Chinese soft-shelled turtle Pelodiscus sinensis. Our results suggest these cells contribute to the function of the secretory glands and contraction of the uterus. Keywords: telocytes uterus Chinese soft-shelled turtle (Pelodiscus sinensis) ultrastructure Introduction Telocytes (TCs) are a novel type of interstitial (stromal) cell that have blast-like cells [3]. -

Interstitial Cells of Cajal and Telocytes in the Gut: Twins, Related Or Simply Neighbor Cells?
BioMol Concepts 2016; 7(2): 93–102 Review Maria Giuliana Vannucchi* and Chiara Traini Interstitial cells of Cajal and telocytes in the gut: twins, related or simply neighbor cells? DOI 10.1515/bmc-2015-0034 Received December 9, 2015; accepted January 22, 2016 Introduction Abstract: In the interstitium of the connective tissue The term telocyte (TC) was introduced for the first time in several types of cells occur. The fibroblasts, responsible the scientific literature in 2010 (1). Since these cells were for matrix formation, the mast cells, involved in local described, an increasing number of papers have been response to inflammatory stimuli, resident macrophages, published on this issue and cells with TC features have plasma cells, lymphocytes, granulocytes and monocytes, been found in almost all mammalian organs (2–7). These all engaged in immunity responses. Recently, another type cells reside in the interstitium of the connective tissue of interstitial cell, found in all organs so far examined, has and are characterized by peculiar features seen using been added to the previous ones, the telocytes (TC). In the transmission electron microscopes (TEM). gut, in addition to the cells listed above, there are also More than a century ago, Santiago Ramon y Cajal the interstitial cells of Cajal (ICC), a peculiar type of cell described a particular cell type in the gastrointestinal exclusively detected in the alimentary tract with multiple tract (GI) that appeared to function as an ‘endostruc- functions including pace-maker activity. The possibility ture’ of the intrinsic nervous system; he named these that TC and ICC could correspond to a unique cell type, cells ‘interstitial neurons’ because they were identifiable where the former would represent an ICC variant outside through staining techniques which specifically labeled the gut, was initially considered, however, further stud- neurons (e.g. -

Cutaneous Neurofibromas: Clinical Definitions Current Treatment Is Limited to Surgical Removal Or Physical Or Descriptors Destruction
ARTICLE OPEN ACCESS Cutaneous neurofibromas Current clinical and pathologic issues Nicolas Ortonne, MD, PhD,* Pierre Wolkenstein, MD, PhD,* Jaishri O. Blakeley, MD, Bruce Korf, MD, PhD, Correspondence Scott R. Plotkin, MD, PhD, Vincent M. Riccardi, MD, MBA, Douglas C. Miller, MD, PhD, Susan Huson, MD, Dr. Wolkenstein Juha Peltonen, MD, PhD, Andrew Rosenberg, MD, Steven L. Carroll, MD, PhD, Sharad K. Verma, PhD, [email protected] Victor Mautner, MD, Meena Upadhyaya, PhD, and Anat Stemmer-Rachamimov, MD Neurology® 2018;91 (Suppl 1):S5-S13. doi:10.1212/WNL.0000000000005792 Abstract RELATED ARTICLES Objective Creating a comprehensive To present the current terminology and natural history of neurofibromatosis 1 (NF1) cuta- research strategy for neous neurofibromas (cNF). cutaneous neurofibromas Page S1 Methods NF1 experts from various research and clinical backgrounds reviewed the terms currently in use The biology of cutaneous fi for cNF as well as the clinical, histologic, and radiographic features of these tumors using neuro bromas: Consensus published and unpublished data. recommendations for setting research priorities Results Page S14 Neurofibromas develop within nerves, soft tissue, and skin. The primary distinction between fi fi Considerations for cNF and other neuro bromas is that cNF are limited to the skin whereas other neuro bromas development of therapies may involve the skin, but are not limited to the skin. There are important cellular, molecular, for cutaneous histologic, and clinical features of cNF. Each of these factors is discussed in consideration of neurofibroma a clinicopathologic framework for cNF. Page S21 Conclusion Clinical trial design for The development of effective therapies for cNF requires formulation of diagnostic criteria that cutaneous neurofibromas encompass the clinical and histologic features of these tumors. -

9Th Clinical Dermatology Congress Psoriasis, Psoriatic Arthritis & Skin
conferenceseries.com Joint Conference Mi Hye Lee et al., J Clin Exp Dermatol Res 2017, 8:6 (Suppl) DOI: 10.4172/2155-9554-C1-066 9th Clinical Dermatology Congress & 2nd International Conference on Psoriasis, Psoriatic arthritis & Skin infections October 16-18, 2017 New York, USA Nonsurgical treatment using micro-insulated needle on neurofibroma Mi Hye Lee, Hak Tae Kim, Woo Jin Lee, Chong Hyun Won, Sung Eun Chang, Mi Woo Lee and Jee Ho Choi University of Ulsan, Korea any studies have investigated the application of micro-insulated needles with radiofrequency (RF) for acne treatment or skin Mrejuvenation. However, there is no study investigating the effects of using micro-insulated needles with RF to treat multiple neurofibroma (NF) lesions. Many patients with multiple neurofibromas usually hesitate to remove all the lesions surgically due to cosmetic concerns. The aim of this study was to evaluate the clinicopathologic outcome, including efficacy and side effects after treatment, using newly developed micro-insulated needles with RF treatment. In this study, two human volunteers received multiple sessions of the micro-insulated needle RF treatment to multiple lesions. Seven to 40 shots were performed on each lesion. The treatment settings were as follows: microneedle penetrating depth of 5.0 mm; insulated 1.0 mm; power 16~46 (level 12~25); and a RF exposure time of 180~400 milliseconds. Skin biopsies were performed before and after the treatment. Outcome assessments included standardized photography, objective measurements of lesion size, histopathologic comparison between before and after the treatment, a physician’s global assessment, and patient satisfaction scores. RF energy could be delivered to the lesions without epidermal damage because the micro-insulation on the needle protects the epidermis from skin burns. -

Clinical Guideline Treatment and Removal of Benign Skin Lesions
Clinical Guideline Guideline Number: CG015, Ver. 5 Treatment and Removal of Benign Skin Lesions Disclaimer Clinical guidelines are developed and adopted to establish evidence-based clinical criteria for utilization management decisions. Oscar may delegate utilization management decisions of certain services to third-party delegates, who may develop and adopt their own clinical criteria. Clinical guidelines are applicable to certain plans. Clinical guidelines are applicable to members enrolled in Medicare Advantage plans only if there are no criteria established for the specified service in a Centers for Medicare & Medicaid Services (CMS) national coverage determination (NCD) or local coverage determination (LCD) on the date of a prior authorization request. Services are subject to the terms, conditions, limitations of a member’s policy and applicable state and federal law. Please reference the member’s policy documents (e.g., Certificate/Evidence of Coverage, Schedule of Benefits) or contact Oscar at 855-672-2755 to confirm coverage and benefit conditions. Summary The integumentary system is comprised of the skin, hair, and nails. The skin is divided into two layers: the dermis and epidermis; diseases of these protective outer layers are among the most common conditions worldwide. Lesions of the skin can be either benign (non-malignant), pre-malignant (potential for evolving into malignancy), or malignant (cancerous). Such lesions arise from congenital malformations or are acquired, often due to extensive UV exposure or underlying illness. Diagnosis is primarily through history, clinical exam, and the appearance of the lesion(s). While the vast majority of benign lesions require no intervention, some cases may necessitate intervention due to bothersome symptoms, for definitive diagnosis, or for exclusion of malignant features. -

Supermicar Data Entry Instructions, 2007 363 Pp. Pdf Icon[PDF
SUPERMICAR TABLE OF CONTENTS Chapter I - Introduction to SuperMICAR ........................................... 1 A. History and Background .............................................. 1 Chapter II – The Death Certificate ..................................................... 3 Exercise 1 – Reading Death Certificate ........................... 7 Chapter III Basic Data Entry Instructions ....................................... 12 A. Creating a SuperMICAR File ....................................... 14 B. Entering and Saving Certificate Data........................... 18 C. Adding Certificates using SuperMICAR....................... 19 1. Opening a file........................................................ 19 2. Certificate.............................................................. 19 3. Sex........................................................................ 20 4. Date of Death........................................................ 20 5. Age: Number of Units ........................................... 20 6. Age: Unit............................................................... 20 7. Part I, Cause of Death .......................................... 21 8. Duration ................................................................ 22 9. Part II, Cause of Death ......................................... 22 10. Was Autopsy Performed....................................... 23 11. Were Autopsy Findings Available ......................... 23 12. Tobacco................................................................ 24 13. Pregnancy............................................................ -

A Review of Telocytes in Cardiovascular Tissue and Their Role in Angiogenesis
REVIEW Anatomy Journal of Africa. 2020. Vol 9 (2): 1807 - 1815. A REVIEW OF TELOCYTES IN CARDIOVASCULAR TISSUE AND THEIR ROLE IN ANGIOGENESIS Ibsen Ongidi, Fadhila Abdulsalaam, Harry Otieno, Noel Odero, Anne Pulei, Moses Obimbo, Kevin Ongeti Correspondence to Ibsen H. Ongidi; Department of Human Anatomy, University of Nairobi. Email: [email protected] ABSTRACT Telocytes are interstitial cells characterized by small cell bodies with very long and slender processes extending from them. They are present in most tissues and are most commonly found in close association with nerves, smooth muscle and microvascular networks in tissue interstitial space. Telocytes maintain tissue homeostasis in various ways including modulation of electrical activity, regulation of stem cell proliferation and angiogenesis. The role of telocytes in blood vessels stems from a structural and functional coupling to vascular endothelial and smooth muscle cells. This review explores the distribution of telocytes in cardiovascular tissues, their mechanisms in angiogenesis and application of this property in tissue regeneration. The literature search was conducted on PubMedTM, Science directTM and African Journals Online databases as well as Google ScholarTM search engines. The keywords used in the literature search included ‘telocytes’, ‘cardiovascular telocytes’, ‘blood vessel’, ‘cardiac tissue’, ‘(neo- )angiogenesis’ and ‘tissue regeneration’. Articles which contained the keywords and relevant citations from their reference lists were included in the study. In conclusion, telocytes display close structural relationship with cardiovascular tissues. They play an angiogenesis inducing role which may be explored as a therapeutic target in tissue repair and regeneration. KEYWORDS : cardiovascular telocytes, interstitial Cajal-like cell, regeneration, angiogenesis INTRODUCTION Telocytes are a specialized type of duodenum (Cantarero et al., 2011). -

The Primary Cilium of Telocytes in the Vasculature: Electron Microscope Imaging
J. Cell. Mol. Med. Vol 15, No 12, 2011 pp. 2594-2600 The primary cilium of telocytes in the vasculature: electron microscope imaging I. Cantarero a, b, *, M. J. Luesma a, b, C. Junquera a, b a Department of Human Anatomy and Histology, Faculty of Medicine, University of Zaragoza, Zaragoza, Spain b Aragon Health Sciences Institute (IϩCS), Zaragoza, Spain Received: February 24, 2011; Accepted: March 17, 2011 Abstract Blood vessels are highly organized and complex structure, which are far more than simple tubes conducting the blood to almost any tissue of the body. The fine structure of the wall of blood vessels has been studied previously using the electron microscope, but the presence the telocytes associated with vasculature, a specific new cellular entity, has not been studied in depth. Interestingly, telocytes have been recently found in the epicardium, myocardium, endocardium, human term placenta, duodenal lamina propria and pleura. We show the presence of telocytes located on the extracellular matrix of blood vessels (arterioles, venules and capillaries) by immunohis- tochemistry and transmission electron microscopy. Also, we demonstrated the first evidence of a primary cilium in telocytes. Several functions have been proposed for these cells. Here, the telocyte-blood vessels cell proximity, the relationship between telocytes, exo- somes and nervous trunks may have a special significance. Keywords: telocytes • primary cilium • vasculature • transmission electron microscopy Introduction Blood vessels are highly organized and complex structure, which found in the epicardium [4], myocardium [5–7], endocardium are far more than simple tubes conducting the blood to almost [8], human term placenta [9], duodenal lamina propria [10] and any tissue of the body.