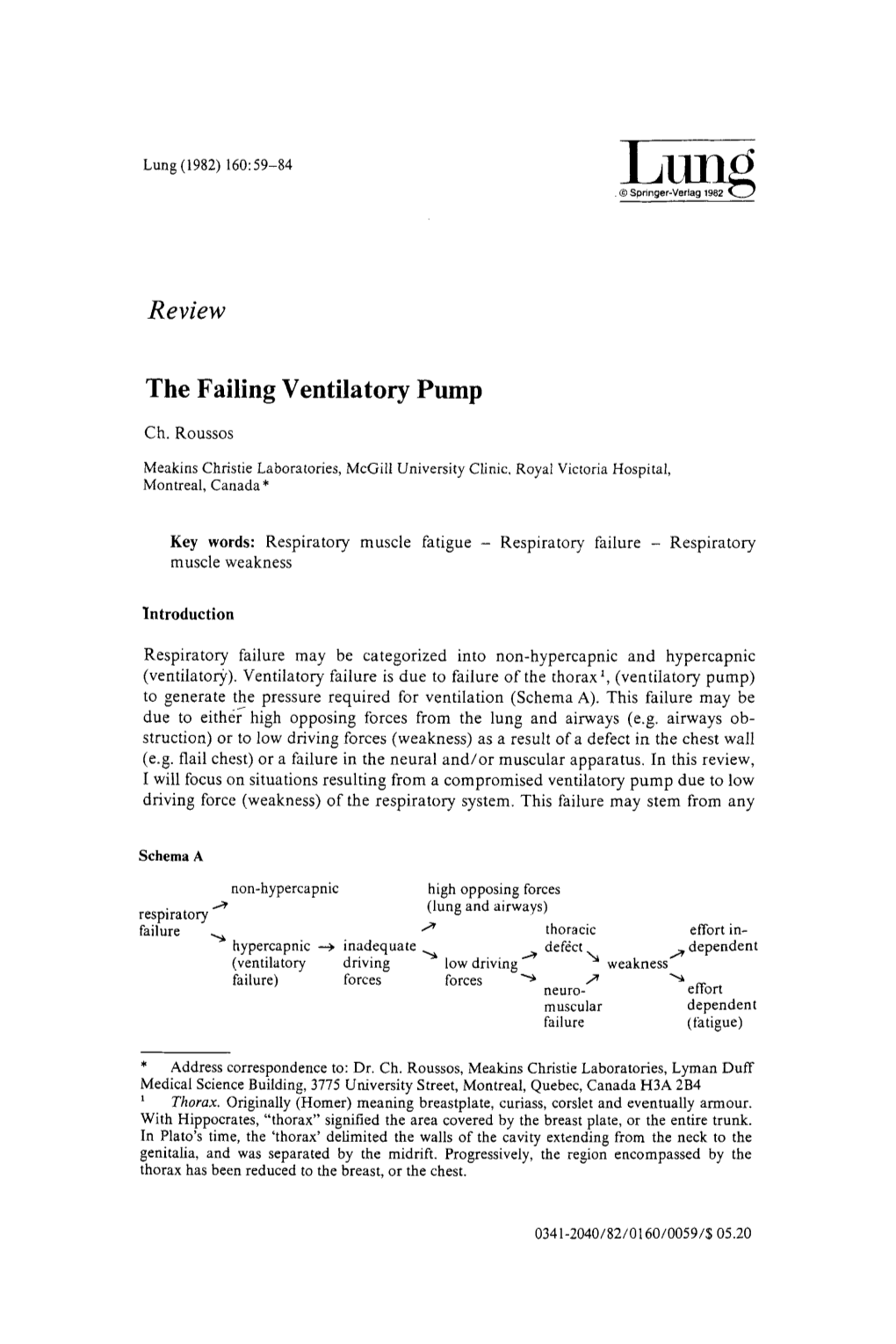
The Failing Ventilatory Pump
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Traumatic Diaphragmatic Hernia: 28-Years Analysis at a Brazilian University Hospital
Traumatic diaphragmatic hernia: 28-years analysis at a Brazilian university hospital Vitor Kruger ( [email protected] ) State University of Campinas Thiago Calderan State University of Campinas Rodrigo Carvalho State University of Campinas Elcio Hirano State University of Campinas Gustavo Fraga State University of Campinas Research Article Keywords: Traumatic diaphragmatic hernia, diaphragm, hernia, diaphragmatic injury Posted Date: December 17th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-121284/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/16 Abstract Background The objective of the study is evaluate the approach to patients with acute traumatic diaphragmatic hernia at a Brazilian university hospital during a 28-year period. Traumatic diaphragmatic hernia is an uncommon injury, however its real incidence may be higher than expected. Sometimes is missed in trauma patients, and is usually associated with signicant morbidity and mortality, this analysis may improve outcomes for the trauma patient care. Methods Retrospective study of time series using and analisys database records of trauma patients at HC- Unicamp was performed to investigate the incidence, trauma mechanism, diagnosis, herniated organs, associated injuries, trauma score, morbidity, and mortality of this injury. Results Fifty-ve cases were analyzed. Blunt trauma was two-fold frequent than penetrating trauma, are associated with high grade injury and motor vehicle collision was the most common mechanism. Left side hernia was four-fold frequent than right side. Diagnose was mostly performed by chest radiography (31 cases; 56%). Associated intra-abdominal injuries were found in 37 patients (67.3%) and extra- abdominal injuries in 35 cases (63.6%). -

Laparoscopic Repair of Chronic Traumatic Diaphragmatic Hernia Using Biologic Mesh with Cholecystectomy for Intrathoracic Gallbladder
CASE REPORT Laparoscopic Repair of Chronic Traumatic Diaphragmatic Hernia using Biologic Mesh with Cholecystectomy for Intrathoracic Gallbladder Jonathan Pulido, MD, Steven Reitz, MD, Suzanne Gozdanovic, MD, Phillip Price, MD ABSTRACT INTRODUCTION Background and Objectives: Diaphragmatic rupture is a Traumatic diaphragmatic hernias have been well de- serious complication of both blunt and penetrating ab- scribed after blunt trauma. Diaphragmatic ruptures can dominal trauma. In the acute setting, delay in diagnosis occur in up to 0.8% to 7% of blunt abdominal trauma, with can lead to severe cardiovascular and respiratory compro- large left-sided defects being the most common.1-4 If the mise. Chronic cases can present years later with a plethora injury is not recognized, progressive herniation of abdom- of clinical symptoms. Laparoscopic techniques are being inal contents may ensue. It is estimated that approximately increasingly utilized in the diagnosis and treatment of 40% to 62% of ruptured diaphragms are missed during the traumatic diaphragmatic hernias. acute hospital stay.1 The time delay to presentation has been reported to be from several weeks to 50 years.3 Method: We describe a case of a 70-year-old female who presented with signs and symptoms of a small bowel Although minimally invasive techniques have been uti- obstruction. She was ultimately found to have an obstruc- lized in the surgical repair of both acute diaphragmatic tion secondary to a chronic traumatic diaphragmatic her- lacerations and chronic traumatic diaphragmatic hernias, nia with an intrathoracic gallbladder and incarcerated its use has not been well defined or universally accepted. small intestine. A cholecystectomy and diaphragmatic her- nia repair were both performed laparoscopically. -

Left Flank Pain As the Sole Manifestation of Acute Pancreatitis
452 CASE REPORTS Emerg Med J: first published as 10.1136/emj.2003.013847 on 23 May 2005. Downloaded from Left flank pain as the sole manifestation of acute pancreatitis: a report of a case with an initial misdiagnosis J-H Chen, C-H Chern, J-D Chen, C-K How, L-M Wang, C-H Lee ............................................................................................................................... Emerg Med J 2005;22:452–453 On further review of the patient’s case 2 hours after the Acute pancreatitis is not an uncommon disease in an ultrasound examination, a decision was made to obtain a emergency department (ED). It manifests as upper abdominal computed tomography (CT) scan due to concern over the pain, sometimes with radiation of pain to the back and flank limitation of ultrasound studies in some clinical conditions. region. Isolated left flank pain being the sole manifestation of The CT showed abnormal fluid collection over the peri-renal acute pancreatitis is very rare and not previously identified in space and pancreatic tail as well as necrotic changes and the literature. In this report, we present a case of acute swelling of the pancreatic tail (fig 1). Serum pancreatic pancreatitis presenting solely with left flank pain. Having enzymes revealed a normal amylase (90 u/L) and a slightly negative findings on an ultrasound initially, she was elevated lipase level (336 u/L). The patient was diagnosed to misdiagnosed as having possible ‘‘acute pyelonephritis or have acute pancreatitis and admitted for supportive treat- other renal diseases’’. A second radiographic evaluation ment and monitoring. During her admission she was also with computed tomography showed pancreatitis in the tail noted to have hyperlipidemia (triglyceride 980 mg/dL and with abnormal fluid collected extending to the left peri-renal cholesterol 319 mg/dL). -

Traumatic Diaphragmatic Hernia
Journal of Surgery Jain SA. J Surg: JSUR-1102. Case Report DOI: 10.29011/2575-9760. 001102 Traumatic Diaphragmatic Hernia Sumita A. Jain* Department of Surgery and Oncology, S.M.S Medical College, Rajasthan, India *Corresponding author: Sumita A. Jain, Department of Surgery and Oncology, S.M.S. Medical College and Attached Hospital, J.L.N. Marg, Jaipur-302004, Rajasthan, India. Tel: +919828118380; Email: [email protected] Citation: Jain SA (2018) Traumatic Diaphragmatic Hernia. J Surg: JSUR-1102. DOI: 10.29011/2575-9760. 001102 Received Date: 25 January 2018; Accepted Date: 27 March, 2018; Published Date: 03 April, 2018 Introduction Diaphragmatic injuries occur in 0.8–1.6%1 of the patients suffering from thoraco-abdominal trauma. Diaphragmatic rupture leads to a traumatic diaphragmatic hernia [1]. Traumatic diaphragmatic hernia occurs in less than 50% of the patients with diaphragmatic injuries.2 Diagnosis of diaphragmatic injuries is difficult and often delayed leading to increased morbidity and mortality. Traumatic diaphragmatic hernia is a rare and often under recognized complication of penetrating and blunt trauma. These injuries are often missed or there is a delay in diagnosis, which can lead to enlargement of the defect and the development of abdominal or respiratory symptoms. Case Report The 35-year-old male presented with complaints of dyspnoea on exertion, with mild pain in the left upper abdomen with history of Road Traffic Accident and blunt trauma chest and abdomen 10 year back. Clinical examination revealed decreased breath sounds on left hemi thorax and presence of gurgling sounds over the left Figure 1: Chest X-ray showed stomach and bowel loops shadows hemi thorax. -

Delayed Presentation of Diaphragmatic Rupture: an Unusual Case of Dyspnea
Delayed Presentation of Diaphragmatic Rupture: An Unusual Case of Dyspnea Fotini C Ampatzidou MD, Charilaos-Panagiotis C Koutsogiannidis MD, Athanasios A Madesis MD PhD, Maria N Sileli MD, and George E Drossos MD PhD Introduction tibia were fractured. Diaphragmatic injury was not de- tected then. Diaphragmatic injuries are relatively rare, and they are The patient was afebrile but distressed due to tachycar- the result of penetrating or blunt trauma. Blunt diaphrag- dia and dyspnea. She was hemodynamically stable, with a matic rupture occurs mainly from high-speed motor vehi- heart rate of 110–120 beats/min and a breathing frequency cle crashes. Sudden increase in intra-abdominal pressure of 20–25 breaths/min. Her P was 70–75 mm Hg on aO2 may cause a diaphragmatic tear and visceral herniation. 4 L/min oxygen delivered via a nasal cannula. On exam- The magnitude of the pressure load on the inflexible cen- ination, she was tender in the left upper quadrant. A stetho- tral tendon by rapid deceleration may cause such cata- scope determined that there were no lung sounds in the left strophic injury. The predicted outcome for these patients is side. Chest x-ray showed a left-sided cavity with air-fluid associated with the severity of the disruption. However, level, multiple old fractured ribs in the left side, and an diaphragmatic rupture may go unnoticed, and in many indistinct costophrenic angle (Fig. 1). cases, diagnosis is delayed. In the delayed phase, symp- Typically, thoracocentesis to obtain a sample of pleural toms are nonspecific and suggestive of other disorders, fluid for diagnostic purposes would be the next step. -

Phrenic Paralysis After Chest Trauma: About 3 Cases
Open Access Journal of Emergency Medical Care CASE REPORT ISSN: 2641-8061 Phrenic Paralysis after Chest Trauma: About 3 Cases Lakranbi M1,2, Harmouchi H1*, Belliraj L1, Ammor FZ1, Issoufou I1, Ouadnouni Y1,2 and Smahi M1, 2 1Department of Thoracic Surgery, CHU Hassan II of Fez-Morocco, Morocco 2Faculty of Medicine and Pharmacy, Sidi Mohamed Ben Abdallah University, Fez-Morocco *Corresponding author: Harmouchi H, Thoracic surgery department, CHU Hassan II of Fez-Morocco, BP: 30000, Tel: 00212664153156, E-mail: [email protected] Citation: Lakranbi M, Harmouchi H, Belliraj L, Ammor FZ, Issoufou I, et al. (2018) Phrenic Paralysis after Chest Trauma: About 3 Cases. J Emerg Med Care 1: 105 Article history: Received: 15 October 2018, Accepted: 05 December 2018, Published: 07 December 2018 Abstract Introduction: Post-traumatic phrenic paralysis remains rare and most often related to cervical trauma, whereas attacks following closed or open chest trauma are very rarely reported. Through three cases of post traumatic diaphragmatic paralysis, we will focus on the mechanism of these paralysis as well as on the diagnostic problems encountered and the therapeutic modalities available. Observation 1: Patient aged 20 years, admitted for multiple thoraco-abdominal wounds, one sitting in parasternal left, another left basithoracic and a third in the right hypochondrium and for whom the chest X-ray shows an elevation of the left diaphragmatic dome. thoracic CT revealed a stomach in the intrathoracic position with liver fracture. The patient underwent laparotomy exploration demonstrating an intact diaphragm with wound of the common bile duct repaired. The chest X-ray of control showed a return of the diaphragm to its normal position. -

Traumatic Diaphragma Rupture: an Experience of 13 Cases
A. I. Filiz et al / Traumatic lesions of the diaphragm Eastern Journal of Medicine 13 (2008) 25 - 29 Original Article Traumatic diaphragma rupture: an experience of 13 cases Ali Ilker Filiza, Yavuz Kurta, Ilker Sucullua*, Ergun Yucela, M.Levhi Akına aGulhane Military Medical Academy, Haydarpasa Training Hospital, Department of General Surgery, Istanbul, Turkey Abstract. Diaphragmatic injury is a rare condition, but late diagnosis may be associated with increased mortality and morbidity. The aim of this study was to present our experience with the management of this injury. Between 2004 to 2007, 13 patients with traumatic diaphragmatic rupture or diaphragmatic hernia were treated. We described the findings in patients, who had operated urgent or had complaints due to intestinal obstruction months to years after an injury. All patients were male and mean age was 23.1 years. Diaphragmatic rupture was left-sided in all patients. Six of these patients had blunt and the remaining 7 had penetrating trauma. Diagnosis of diaphragmatic rupture was established in less than 24 hours in 4 patients. In the remaining 9 patients, who developed intra- throracic herniation of abdominal organs, diagnostic delay ranged from 12 to 48 months. The most frequent herniated organ was transverse colon. Non-absorbable sutures were used for closure of the defect. Complication rate was 30% and no death was observed. After blunt or penetrating trauma in upper abdomen and distal chest, a high index of suspicion is important to diagnose diaphragmatic rupture. Late presentations are associated with increased morbidity. Key words: Blunt/penetrating trauma, diaphragmatic rupture, diaphragmatic hernia, complication reported that missed diaphragmatic injuries in 1. -

Diaphragm Injury- Laparoscopy
Diaphragm Injury- Laparoscopy Steve Eubanks, MD Chair of Academic Surgery Executive Director of the Institute for Surgical Advancement AdventHealth Orlando Professor of Surgery- University of Central Florida SAGES Past President Disclosures EB Surgical C-Clear Founder/Partner CORI Diaphragm Injury Is there a role for minimally invasive surgery in the management of traumatic injury of the diaphragm? Diaphragmatic Rupture Blunt or Penetrating Acute or delayed diagnosis Occurs in 5% of blunt trauma to the torso Occurs in 8% of patients with blunt trauma to the chest Diaphragmatic Rupture Diaphragmatic tears from blunt trauma are most frequently caused by MVAs and falls. Mortality rates range from 15-40% in patients with blunt rupture Associated injuries occur in 80-100% of patients Associated injuries commonly involve head trauma, liver, spleen, aorta, pelvis, lung, long bones Lung injuries are the most common cause of death associated with rupture of the diaphragm Diaphragmatic Rupture A blow to the side is 3 times more likely to cause rupture of the diaphragm than a blow to the front 50-80% of ruptures occur on the left Rupture on the right is usually associated with significant liver injury. Mortality is higher with right-side diaphragmatic rupture Diaphragmatic Rupture Bilateral rupture of the diaphragm occurs in 1-2% of cases of injury to the diaphragm. Mortality is much higher with bilateral rupture. Diaphragmatic Rupture Penetrating trauma accounts for 12-20% of diaphragmatic ruptures. GSWs or stab wounds to the lower chest or upper abdomen raise the index of suspicion for diaphragm injury. Mortality rates are reported to be 10-30% with penetrating injuries to the diaphragm with almost 100% of deaths due to associated injuries. -

TRAUMATIC DIAPHRAGMATIC HERNIA Arcot Rekha A, Ananthakrishnan Vikrama ABSTRACT Asymptomatic State
Case Reports TRAUMATIC DIAPHRAGMATIC HERNIA Arcot Rekha a, Ananthakrishnan Vikrama ABSTRACT asymptomatic state. Patients are often seen initially by the Traumatic diaphragmatic hernias are uncommon, yet physician for respiratory symptoms. associated with high mortality. The colon very rarely Key words : trauma, diaphragm, hernia herniates through the diaphragmatic defect. This case is submitted as the diagnosis was delayed due to an initial SRJM 2010;3:23-25 INTRODUCTION Diaphragmatic rupture occurs due to blunt or penetrating injury, either as an acute presentation or delayed as respiratory distress or obstruction[1], can be managed through a laparotomy or a thoracotomy[2] and in the present day with minimal access surgery. Given the number of variables a review of this condition is interesting and thought provoking. HISTORICAL VIGNETTE Traumatic diaphragmatic hernia apparently was Fig 1 : Chest X-ray & CT showing the diaphragm hernia described by Sennertus, who in 1541 reported an instance A plain X Ray taken in the ER showed bowel loop of delayed herniation of viscera through an injured shadows in the chest (Fig 1 left inset).She was stabilised in [3] diaphragm . Ambroise Paré, in 1579, described the first ER and then shifted for a CT thorax and abdomen which case of diaphragmatic rupture diagnosed at autopsy. The showed herniation of the bowel loops through the left patient was a French artillery captain who initially survived hemi diaphragm. There was mediastinal shift to the right a gunshot wound of the abdomen, but died 8 months later and there was little lung field visualized on the left chest of a strangulated gangrenous colon, herniating through a (Fig 1-right inset). -

Acute and Chronic Traumatic Diaphragmatic Hernia: 10 Years’ Experience
RESEARCH ARTICLE Acute and chronic traumatic diaphragmatic hernia: 10 years' experience 1☯ 1☯ 2 1 Pengcheng Gu , Yang Lu , Xigong LiID *, Xiangjin Lin 1 Trauma centre, First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, China, 2 Department of Orthopedics, First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, China ☯ These authors contributed equally to this work. * [email protected] a1111111111 a1111111111 a1111111111 a1111111111 Abstract a1111111111 Controversy persists regarding many aspects of traumatic diaphragmatic hernia (TDH). We aimed to understand why some traumatic diaphragmatic injuries present with chronic hernia and to evaluate diagnosis and treatment options. Fifty acute and 19 chronic TDH patients were diagnosed and treated at our institution over a 10-year period. Clinical data from these OPEN ACCESS two groups were analyzed statistically and compared. Chronic TDH patients had a signifi- Citation: Gu P, Lu Y, Li X, Lin X (2019) Acute and cantly lower Injury Severity Score than acute TDH patients (10.26 ± 2.68 vs. 26.92 ± 4.79, chronic traumatic diaphragmatic hernia: 10 years' P < 0.001). The most common surgical approach for acute and chronic TDH was thoracot- experience. PLoS ONE 14(12): e0226364. https:// doi.org/10.1371/journal.pone.0226364 omy and laparotomy, respectively. The length of the diaphragmatic rupture was significantly shorter in chronic TDH patients than acute TDH patients (6.00 ± 1.94 cm vs. 10.71 ± 3.30 Editor: Linda L. Maerz, Yale University, UNITED STATES cm, P < 0.001). The mean length of hospital stay was significantly longer for acute TDH patients than chronic TDH patients (41.18 ± 31.02 days vs. -

Treatment of Post-Traumatic Rhabdomyolysis with a Combined Purification Strategy: a Case Report
Treatment of post-traumatic rhabdomyolysis with a combined purification strategy: a case report. ROMITO FM, ARMENTO M, CANIGLIA F, CASCIONE R, CIAMPO G, GAUDIO L, NICOLETTI R, SCHIEVENIN MG, ZUCCARO F, DIMONA F Terapia Intensiva Ospedale Madonna delle Grazie, MATERA – ASMBASILICATA Background Crush syndrome or traumatic rhabdomyolysis, a medical condition characterized by major shock and renal failure after a crushing injury to skeletal muscle is a challenge for intensivist. Methods We present a case regarding a young man (19 years old) victim of a motorbike accident in urban environment. He was conducted by emergency equipe (i.e. 911) in local emergency department. At admission he was awake and collaborative, with retrosternal/epigastric pain, and exposed fracture of the left knee with important lesion of the popliteal artery, low arterial pressure. Total body TC was performed: rupture of the diaphragm with herniation of the stomach, lung contusion, hemoperitoneum, right acetabulum and whole iliac wing fracture, confirmed left knee fracture with vascular lesion (ISS66). Urgent surgery was immediatly performed under general anaesthesia: reparation of the diaphragmatic rupture with stomach repositioning, correction of intraperitoneal hemorrage (from mesenteric artery), urgent vascular graft of the poplitea artery. The patient was conducted in ICU. He was sedated and curarized, under mechanical ventilation. Routine emergency Laboratory test was performed, and we notice low Hb level and an increasing value of myoglobin (up to 60000 mg%), with a rapid and progressive worsening of renal function, suggestive for AKI. So we started Continuous Renal Replacement Therapy in CVVHD CiCa using an highly adsorbent cartridge in order to remove Citokines and myoglobin (Citosorb®) and a secondary high-cut off dyalisis filter (Emic2®). -

Phrenic Nerve Injury Following Blunt Trauma
J Accid Emerg Med 2000;17:419–428 419 J Accid Emerg Med: first published as 10.1136/emj.17.6.426 on 1 November 2000. Downloaded from CASE REPORTS Phrenic nerve injury following blunt trauma David Bell, Ajith Siriwardena Abstract Phrenic nerve trauma in the absence of direct injury is unusual and may present diagnostic diYculty. Diaphragmatic pa- ralysis resulting from phrenic nerve injury may closely mimic diaphragmatic rupture. This case highlights the value of magnetic resonance imaging in establishing dia- phragmatic integrity and of ultrasono- graphic assessment during respiratory excursion in confirming diaphragmatic paralysis. In cases of non-contact injury involving torsional injury to the neck, an index of clinical awareness may help to establish the diagnosis of phrenic nerve trauma. Figure 1 Posteroanterior chest radiograph taken after (J Accid Emerg Med 2000;17:419–420) injury showing elevated right hemi-diaphragm. Keywords: phrenic nerve injury; blunt trauma diaphragmatic rupture was made. Computed tomography demonstrated mild rotation of the axis of the liver (anti-clockwise rotation Case report through the plane of the middle hepatic vein) A 36 year old man was admitted to the compatible with diaphragmatic rupture. How- accident and emergency department two hours ever, a magnetic resonance scan confirmed Y after a road tra c accident. The patient was that the diaphragm was intact but elevated. driving a car that had been struck on the near- Ultrasound scan with respiratory excursion http://emj.bmj.com/ side by another vehicle. The patient’s vehicle demonstrated paralysis of the right hemi- had been stationary at the time of impact.