An Overview of the Current Genetic and Phenotypical Selection Strategies to Reduce the Prevalence of Feline Hypertrophic Cardiomyopathy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Abyssinian Cat Club Type: Breed
Abyssinian Cat Association Abyssinian Cat Club Asian Cat Association Type: Breed - Abyssinian Type: Breed – Abyssinian Type: Breed – Asian LH, Asian SH www.abycatassociation.co.uk www.abyssiniancatclub.com http://acacats.co.uk/ Asian Group Cat Society Australian Mist Cat Association Australian Mist Cat Society Type: Breed – Asian LH, Type: Breed – Australian Mist Type: Breed – Australian Mist Asian SH www.australianmistcatassociation.co.uk www.australianmistcats.co.uk www.asiangroupcatsociety.co.uk Aztec & Ocicat Society Balinese & Siamese Cat Club Balinese Cat Society Type: Breed – Aztec, Ocicat Type: Breed – Balinese, Siamese Type: Breed – Balinese www.ocicat-classics.club www.balinesecatsociety.co.uk Bedford & District Cat Club Bengal Cat Association Bengal Cat Club Type: Area Type: PROVISIONAL Breed – Type: Breed – Bengal Bengal www.thebengalcatclub.com www.bedfordanddistrictcatclub.com www.bengalcatassociation.co.uk Birman Cat Club Black & White Cat Club Blue Persian Cat Society Type: Breed – Birman Type: Breed – British SH, Manx, Persian Type: Breed – Persian www.birmancatclub.co.uk www.theblackandwhitecatclub.org www.bluepersiancatsociety.co.uk Blue Pointed Siamese Cat Club Bombay & Asian Cats Breed Club Bristol & District Cat Club Type: Breed – Siamese Type: Breed – Asian LH, Type: Area www.bpscc.org.uk Asian SH www.bristol-catclub.co.uk www.bombayandasiancatsbreedclub.org British Shorthair Cat Club Bucks, Oxon & Berks Cat Burmese Cat Association Type: Breed – British SH, Society Type: Breed – Burmese Manx Type: Area www.burmesecatassociation.org -

TICA Sphynx Breed Introduction
TICA Sphynx Breed Introduction www.tica.org General Description: The intriguing Sphynx cat never fails to draw a reaction from people - some people love the bald, wrinkled look, some are fascinated by the cat, while others are less than enthusiastic. But for those that take the time to get to know the cat, a great treat is in store. They have very soft skin that feels like the softest chamois leather and are so very warm to the touch that you just want to cuddle up with them-especially in cold weather. Their toes are like fingers and they use them that way as they investigate and play with everything that takes their curiosity. They wrinkled faces remind you of the wisdom we all gather with age while their big ears and lemon-shaped eyes give them a unique look. Their rounded Buddha-like bodies bring a smile to the face. The Sphynx is definitely an enigmatic breed for the connoisseur. History: First attempts at breeding Sphynx began in 1966, when a black and white cat gave birth to a hairless kitten in Ontario, Canada. The owner named the hairless kitten Prune, due to the wrinkled hairless skin. Prune was bred to other cats in an attempt to create more hairless kittens. Because hairlessness is a recessive gene, some of the kittens resulting from this union had hair, while others did not. These kittens were called Canadian Hairless Cats, which some people referred to as Sphynx cats, due to their physical similarities with an ancient Egyptian cat sculpture called the Sphinx. -

SE Region April 2011 Newsletter
SE Region April 2011 Newsletter Meet Your Neighbors Name Ed Manning Location Raleigh, NC Cattery Wizardgate www.wizardgate.org 1. What breed do you work with..??.. I have worked with several breeds over the years. When I first started in the cat fancy in 1987 I worked with the entire Persian breed group. the Himalayan, Persian, and the Exotic Shorthair until I received my first sphynx alter in 1998. I showed him for 2 years and decided I wanted to work with the sphynx breed. I started actively working with my breeding program in April of 2000. I enjoy the sphynx breed by far . I find them to be not like any other breed of cat. Their personality will win you over by far. Over the years I have shared my home with several other breeds of cats, Tonk's, Bombay, Burmese, Siamese, American Bobtail, Manx, Dsh, Birman, Mainecoon, American Shorthair and a Bengal. How long..??.. I started in 1987 to present 2. If you could, what other breed of cat would you like to work with..??.. I find the Japanese Bobtail to be very interesting but have cut back on my breeding program at the moment and working with a very limited number of kitties. 3. What is your most memorable win..??.. My most memorable win was my IW win with IW, SGC Wizardgate's Daddy's Girl. She got an IW as a kitten, RW as an Adult in the same year and then received an IW as an adult the following year. and she truly is Daddy's Girl. -
Sept Oct 2010 Color Version
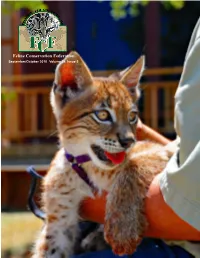
Feline Conservation Federation September/October 2010 Volume 54, Issue 5 TABLE OF Features 8 2010 Convention Review: contents Tim Stoffel SEPTEMBER/OCTOBER 2010 | VOLUME 54, ISSUE 5 It’s official, Tim declares this year’s the “best ever!” 12 Election Time for the FCF Board of Directors Candidate platforms for voter consid- eration. 28 Reminiscences of Dutchie: A Leop- ard Cat Laura Reeder remembers teenage years with an Asian leopard cat. 30 Managing your own People Mindy Stinner concentrates on those insidious insiders. 32 2010 FCF Convention review: Jim and Nora Battista Hot, Hot, Hot, and plenty of pussy cats, too! 33 2010 FCF Convention review: Robert and Sandra Lee Hohn FCF members make the memories. 34 Enrichment at the 2010 Convention Debi Willoughby helps us improve our cats’ quality of life. 35 Cats Went Head over Heels for Their New Toys! Brandon Null reports enrichments were a big hit at Tiger Safari. 45 Minutes and Summary: 2010 Annu- al Convention General Membership Meeting Questions and Answers and the pre- miere of An In(CAT)venient Truth. Cover Photo: 8 Siberian lynx cub, Salty. Photo by Tony Richards. Read more on page 52. 28 21 Photo by Thierry Plaud Photo by harryandanimals 41 Photo by Alain Compost Feline Conservation Federation Volume 54, Issue 5 • September/October 2010 TO SUBSCRIBE TO THE FCF JOURNAL AND JOIN FCF IN ITS CONSERVATION EFFORTS A membership to FCF entitles you to six issues of the Journal, the back-issue DVD, an invitation to FCF husbandry and wildlife education courses and annual convention, and participation in our online discussion group. -

READING LEVEL O: Where's Your Hair?
Where’s Your Hair? LEVELED BOOK • O A Reading A–Z Level O Leveled Book Word Count: 682 Where’s Your Hair? Written by Charles C. Hofer Visit www.readinga-z.com www.readinga-z.com for thousands of books and materials. Photo Credits: Hairless All Around Us Glossary Front cover, pages 9, 15: © Jean-Michel Labat/ardea.com; back cover: © Eddie Boldizsar/REX USA; title page, page 8: © GlobalP/iStock/Thinkstock; page 3: © Jacqueline Hunkele/iStock/Thinkstock; page 4: © GROSSEMY VANESSA/ Hairless animals are everywhere. They adapted (v.) changed to fit a new or specific Where’s Alamy; page 5: © Juniors Bildarchiv GmbH/Alamy; page 6: © Tierfotoagentur/ Alamy; page 10: © Phil Yeomans/REX USA; page 11 (top): © krechet/iStock/ situation or environment (p. 12) Thinkstock; page 11 (bottom): © allesalltag/Alamy; page 12: © Wade Payne/AP can be wild animals or cuddly pets. Images; page 13: © Frans Lanting Studio/Alamy; page 14 (top): © Peter Zigich/ Some hairless animal breeds are Hemera/Thinkstock; page 14 (bottom): © Andrey Nekrasov/imagebroker/Corbis breeds (n.) groups of animals or plants Your Hair? Back Cover: A Chinese crested dog enjoys (?) a bath. thousands of years old, while others are that are alike as a result of Front Cover: The fantastic (and hairless) four: a Mexican xolo dog, sphynx cat, brand new. Who knows what kind of controlled reproduction (p. 4) guinea pig, and rat hairless animal will pop up next? Title Page: A Chinese crested puppy shows us its good side. bred (v.) cared for an animal or plant Page 3: A sphynx cat nuzzles her kitten. -

A Super Show Cat Do You Want a Feline That You Can Enter in Cat Shows? Sphynx Cats Are Natural Show-Offs
THIS PAGE INTENTIONALLY LEFT BLANK Elaine Landau a lerner Publications comPany • minneaPolis Copyright © 2011 by Lerner Publishing Group, Inc. All rights reserved. International copyright secured. No part of this book may be reproduced, stored in a retrieval system, or transmitted in any form or by any means—electronic, mechanical, photocopying, recording, or otherwise— without the prior written permission of Lerner Publishing Group, Inc., except for the inclusion of brief quotations in an acknowledged review. Lerner Publications Company A division of Lerner Publishing Group, Inc. 241 First Avenue North Minneapolis, MN 55401 U.S.A. Website address: www.lernerbooks.com Library of Congress Cataloging-in-Publication Data Landau, Elaine. Sphynx are the best! / by Elaine Landau. p. cm. — (The best cats ever) Includes index. ISBN 978-0-7613-6429-0 (lib. bdg. : alk. paper) 1. Sphynx cat—Juvenile literature. I. Title. SF449.S68L36 2011 636.8—dc22 2010028472 Manufactured in the United States of America 1 — C G — 1 2 / 3 1 / 1 0 CHAPTER ONE CHAPTER TWO where’s the story the hair? behind the 4 sphynx 10 CHAPTER THREE the Sphynx CHAPTER FOUR and you welcome 16 your sphynx 22 Glossary . 30 For more information . 31 index . 32 I’m thinking of a special cat. This curious kitty is not like most felines. Some cats have long, fluffy coats. Other cats have hair that’s nice and short. But the sphynx is almost hairless. At first, you might not think it looks like a cat at all. Sphynx cats stand out in a crowd. These cats have only a thin layer of hair, usually on their noses, tails, and feet. -

Werewolf, There Wolf: Variants in Hairless Associated with Hypotrichia and Roaning in the Lykoi Cat Breed
G C A T T A C G G C A T genes Article Werewolf, There Wolf: Variants in Hairless Associated with Hypotrichia and Roaning in the Lykoi Cat Breed 1, 1, 1 1 Reuben M. Buckley y, Barbara Gandolfi y, Erica K. Creighton , Connor A. Pyne , Delia M. Bouhan 1, Michelle L. LeRoy 1,2, David A. Senter 1,2, Johnny R. Gobble 3, 4,5 1, Marie Abitbol , Leslie A. Lyons * and 99 Lives Consortium z 1 Department of Veterinary Medicine and Surgery, College of Veterinary Medicine, University of Missouri, Columbia, MO 65211, USA; [email protected] (R.M.B.); Barbara-Gandolfi@idexx.com (B.G.); [email protected] (E.K.C.); [email protected] (C.A.P.); [email protected] (D.M.B.); [email protected] (M.L.L.); [email protected] (D.A.S.) 2 Veterinary Allergy and Dermatology Clinic, LLC., Overland Park, KS 66210, USA 3 Tellico Bay Animal Hospital, Vonore, TN 37885, USA; [email protected] 4 NeuroMyoGène Institute, CNRS UMR 5310, INSERM U1217, Faculty of Medicine, Rockefeller, Claude Bernard Lyon I University, 69008 Lyon, France; [email protected] 5 VetAgro Sup, University of Lyon, Marcy-l’Etoile, 69280 Lyon, France * Correspondence: [email protected]; Tel.: +1-573-884-2287 These authors contributed equally to this work. y Membership of the 99 Lives Consortium is provided in the Acknowledgments. z Received: 12 May 2020; Accepted: 12 June 2020; Published: 22 June 2020 Abstract: A variety of cat breeds have been developed via novelty selection on aesthetic, dermatological traits, such as coat colors and fur types. -

Clinical and Histologic Description of Lykoi Cat Hair Coat and Skin
獣医臨床皮膚科 22 (3): 179–191, 2016 Original Clinical and Histologic Description of Lykoi Cat Hair Coat and Skin リコイ猫の被毛と皮膚に関する臨床的および組織学的記述 Michelle L. LeRoy1, 2)*, David A. Senter1, 2), Dae Young Kim3), Barbara Gandolfi2), John R. Middleton2), Karen E. Trainor4), Delia M. Bouhan2), Leslie A. Lyons2) 1)Veterinary Allergy and Dermatology Clinic, LLC, 2)Department of Veterinary Medicine and Surgery, University of Missouri, College of Veterinary Medicine, 3)Department of Veterinary Pathobiology, University of Missouri, College of Veterinary Medicine, 4)Innovative Vet Path, LLC Received April 9, 2016 and accepted June 7, 2016 Abstract: Hair and skin abnormalities of domesticated animals are readily identified and are biomedical models for ectodermal dysplasias. The hair coat of the Lykoi cat, a new cat breed, is a dramatic phenotype and has not been clinically or histologically described. Dermatoscopic examination was performed and skin biopsies were collected from seven Lykoi cats and seven dermatologically normal domestic shorthair (DSH) cats. All skin structures were examined on longitudinal and transverse sections. Immunohistochemistry for CD3 and Cytokeratin 8/18 was performed for comparison with DSH cats. Dermatoscopic images were compared. Lykoi had a significant reduction in average numbers of follicles per hair follicle group as compared to DSH cats, 14.7 ± 2.9 and 23.4 ± 5.4, respectively. Median (range) numbers of hairs per hair follicle group were 1.3 (0.4–5.7) and 18.8 (10.6–26.6), respectively. Mean (± SD) hair follicle depth was 0.95 mm ± 0.15 and 1.14 mm ± 0.21 for Lykoi and DSH cats, respectively. Mean (± SD) primary hair shaft diameters were 39 µm ± 0.029 and 47 µm ± 0.011 for Lykoi and DSH cats, respectively. -

Truth About Cats and Dogs
Everybody wants to be a cat Bengal Cat Siberian Cat Savanah Cat Siamese Cat Sphinx Cat Russian Blue Memories Big Ear Cat . One of the most popular breeds of cat in the USA, this short-haired breed has the old name for the country where it was thought to have originated. Which fine-boned, slender, medium-sized breed of cat is this? Abyssinian Abyssinian • Although this breed was developed in Great Britain, it was given the old name for what is now Ethiopia/Abyssinia. • It was thought the breed developed from kittens brought home by returning soldiers coming from that part of the world. • There is an element of truth in the story but, it now seems that the soldiers almost certainly bought their kittens from Egyptian traders, rather than Ethiopian ones. Indeed, recent research suggests that the breed may have developed from a single cat, named Zula, bought by a soldier in Alexandria in 1868. • This breed is sometimes called a "Purebred Long-haired Siamese", since is developed as a mutation from the standard Siamese. Noted for its sapphas a light-coloured body with darker extremities. Considered the most intelligent of all long- haired breeds, which cat is this? Bengal Bengal cat • This is a rare breed of domestic cat from France. Large and muscular(called cobby) with relatively short, fine-boned limbs, and very fast reflexes. They are known for their blue (grey) water-resistant short hair double coats and orange or copper-colored eyes. They are also known for their “smile”. These cats are exceptional hunters and are highly prized by farmers. -

Echocardiographic Parameters in Healthy Young Adult Sphynx Cats
Schweiz. Arch. Tierheilk. E.Mottet, C.Amberger, M.G. Doherr, C. Lombard, Band 154, Heft 2, Februar 2012, xxx – xxx © 2012 by Verlag Hans Huber, Hogrefe AG, Bern DOI 10.1024/0036-7281/a00000x Echocardiographic parameters in Sphynx cats 1 Echocardiographic parameters in healthy young adult Sphynx cats E.Mottet 1, C.Amberger 1, M.G. Doherr 2, C. Lombard 2 1 Cabinet Vétérinaire Amberger-Philip, Genève, 2 Clinic of Small Animals, University of Bern Summary Echokardiographische Parameter bei jungen, gesunden, erwachsenen Sphynxkatzen The objective of this retrospective study is to deter- mine normal reference values for 2-Dimension (2D) Das Ziel dieser retrospektiven Studie ist die Festle- and Motion-mode (M-mode) echocardiographic pa- gung von Normalwerten für 2D- und Motion-Mode rameters in nonsedated healthy young adult Sphynx (M-Mode) echokardiographische Parameter bei nicht cats and to compare them to those of the domestic sedierten, gesunden, jungen, erwachsenen Sphynxkat- shorthair (DSH). 131 Sphynx cats underwent cardiac zen und diese Werte mit denjenigen der Europäischen screening prior to breeding. The control group con- Kurzhaarkatze zu vergleichen. 131 Sphynx Katzen sisted of 30 healthy adult domestic cats. A complete wurden vor dem ersten Zuchteinsatz kardiologisch cardiac ultrasound was performed on all cats using untersucht. Die Kontrollgruppe bestand aus 30 gesun- right parasternal long and short axis views. There den, erwachsenen Hauskatzen. Eine komplette Herz- were few echocardiographic parameters in the Sphynx prüfung wurde unter Berücksichtigung der rechten that differed from those of the healthy DSH. Only the parasternalen, langen und kurzen Achsen durchge- left atrial (LA) dimension in 2D and M-mode, the left führt. -
Understanding the Elderly Cat Safeguard Your Pets Against Ticks
... Expert information on medicine, behaviorandhealth from a world leader in veterinary medicine INSIDE Understanding the Elderly Cat Short Takes 2 Dietary help for constipation; protein Happily, our pets are living longer, But that means we and kidney function; facial dermatitis and feline herpesvirus. need to be prepared for some behavioral changes, too. Cats and Separation Anxiety 3 Felines can experience stress when hanks to ad tooth loss may alter there's achange in the household. Tvances in all its eating habits; and fields of veterinary progressive hearing Is Your Cat's Hearing Failing? 4 medicine, it is not problems may make lhe cause {ould be arampant over uncommon these a cat decreasingly growth of yeast in the ear {anals. days for a cat to live responsive to its en to the very ripe old vironment. Movies to Entertain Our Cats 5 age of20 roughly In some cases, lhey can be agreat daytime babysitter the physiologic however, an elderly for the bored feline in your home. equivalent of age 93 eat's behavioral pe Ask Elizabeth: 8 in a human. That's culiarities will Can aromatherapy be potentially the good news. - despite thorough harmful to our cats? The bad news is veterinaryexamina that cats, like humans, become increasingly tion and laboratory testing remain unat IN THE NEWS '" susceptible to age-related disease conditions tributable to any underlying disease condi as they grow old, and most of these disorders tion. In such a case, the animal is apt to be Grants to Study FIP are bound to have an effect on an animal's diagnosed as "senile," a vague term used to and Other Diseases behavior. -

VIJ March 2019.Indd 154 01/03/2019 16:44 CONTINUING EDUCATION I SMALL ANIMAL
SMALL ANIMAL I CONTINUING EDUCATION Cat breeds: the hidden problem of inherited diseases Pedigree cats are far less widely kept compared to pure-bred dogs, but there are signs that this may be beginning to change, writes Pete Wedderburn BVM&S CertVR MRCVS, Brayvet, Co. Wicklow who details the inherited disorders that are common in these breeds While around 90 per cent of pet cats are still classified attributes, creating a new breed within decades. The as cross-bred (either domestic short-haired or domestic Munchkin breed is a good example: this was developed after long-haired) pedigree cats are increasingly popular. As an unowned, short-legged, black cat was found living under with pedigree dogs, they have an element of predictability, a trailer in Louisiana in 1983. This cat was pregnant when with strong personalities and distinctive appearances. And she was taken in, and it turned out that half of her kittens as with any situation where there is an increase in interest were born with abnormally short legs. One of the kittens was and numbers of a particular type of cat, there is likely to be then used for breeding, becoming the founder of a breeding an increase in problems. Just like pedigree dogs, pedigree programme that went on to establish the new cat breed in cats can carry inherited problems that can mean illness and North America. suªering for aªlicted individuals, a challenge for the vets The challenge in this type of situation is that development of recruited to treat them, and expensive veterinary bills for their a new breed like this requires rapid, high-turnover, selective owners.