Vulvar Conditions & Management
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ovarian Cancer and Cervical Cancer
What Every Woman Should Know About Gynecologic Cancer R. Kevin Reynolds, MD The George W. Morley Professor & Chief, Division of Gyn Oncology University of Michigan Ann Arbor, MI What is gynecologic cancer? Cancer is a disease where cells grow and spread without control. Gynecologic cancers begin in the female reproductive organs. The most common gynecologic cancers are endometrial cancer, ovarian cancer and cervical cancer. Less common gynecologic cancers involve vulva, Fallopian tube, uterine wall (sarcoma), vagina, and placenta (pregnancy tissue: molar pregnancy). Ovary Uterus Endometrium Cervix Vagina Vulva What causes endometrial cancer? Endometrial cancer is the most common gynecologic cancer: one out of every 40 women will develop endometrial cancer. It is caused by too much estrogen, a hormone normally present in women. The most common cause of the excess estrogen is being overweight: fat cells actually produce estrogen. Another cause of excess estrogen is medication such as tamoxifen (often prescribed for breast cancer treatment) or some forms of prescribed estrogen hormone therapy (unopposed estrogen). How is endometrial cancer detected? Almost all endometrial cancer is detected when a woman notices vaginal bleeding after her menopause or irregular bleeding before her menopause. If bleeding occurs, a woman should contact her doctor so that appropriate testing can be performed. This usually includes an endometrial biopsy, a brief, slightly crampy test, performed in the office. Fortunately, most endometrial cancers are detected before spread to other parts of the body occurs Is endometrial cancer treatable? Yes! Most women with endometrial cancer will undergo surgery including hysterectomy (removal of the uterus) in addition to removal of ovaries and lymph nodes. -

The Cyclist's Vulva
The Cyclist’s Vulva Dr. Chimsom T. Oleka, MD FACOG Board Certified OBGYN Fellowship Trained Pediatric and Adolescent Gynecologist National Medical Network –USOPC Houston, TX DEPARTMENT NAME DISCLOSURES None [email protected] DEPARTMENT NAME PRONOUNS The use of “female” and “woman” in this talk, as well as in the highlighted studies refer to cis gender females with vulvas DEPARTMENT NAME GOALS To highlight an issue To discuss why this issue matters To inspire future research and exploration To normalize the conversation DEPARTMENT NAME The consensus is that when you first start cycling on your good‐as‐new, unbruised foof, it is going to hurt. After a “breaking‐in” period, the pain‐to‐numbness ratio becomes favourable. As long as you protect against infection, wear padded shorts with a generous layer of chamois cream, no underwear and make regular offerings to the ingrown hair goddess, things are manageable. This is wrong. Hannah Dines British T2 trike rider who competed at the 2016 Summer Paralympics DEPARTMENT NAME MY INTRODUCTION TO CYCLING Childhood Adolescence Adult Life DEPARTMENT NAME THE CYCLIST’S VULVA The Issue Vulva Anatomy Vulva Trauma Prevention DEPARTMENT NAME CYCLING HAS POSITIVE BENEFITS Popular Means of Exercise Has gained popularity among Ideal nonimpact women in the past aerobic exercise decade Increases Lowers all cause cardiorespiratory mortality risks fitness DEPARTMENT NAME Hermans TJN, Wijn RPWF, Winkens B, et al. Urogenital and Sexual complaints in female club cyclists‐a cross‐sectional study. J Sex Med 2016 CYCLING ALSO PREDISPOSES TO VULVAR TRAUMA • Significant decreases in pudendal nerve sensory function in women cyclists • Similar to men, women cyclists suffer from compression injuries that compromise normal function of the main neurovascular bundle of the vulva • Buller et al. -

Pregnancy and Cesarean Delivery After Multimodal Therapy for Vulvar Carcinoma: a Case Report
MOLECULAR AND CLINICAL ONCOLOGY 5: 583-586, 2016 Pregnancy and cesarean delivery after multimodal therapy for vulvar carcinoma: A case report KUNIAKI TORIYABE1,2, HARUKI TANIGUCHI2, TOKIHIRO SENDA2,3, MASAKO NAKANO2, YOSHINARI KOBAYASHI2, MIHO IZAWA2, HIROHIKO TANAKA2, TETSUO ASAKURA2, TSUTOMU TABATA1 and TOMOAKI IKEDA1 1Department of Obstetrics and Gynecology, Mie University Graduate School of Medicine, Tsu, Mie 514-8507; 2Department of Obstetrics and Gynecology, Mie Prefectural General Medical Center, Yokkaichi, Mie 510-8561; 3Department of Obstetrics and Gynecology, Kinan Hospital, Mihama, Mie 519-5293, Japan Received November 4, 2015; Accepted September 12, 2016 DOI: 10.3892/mco.2016.1021 Abstract. Reports of pregnancy following treatment for vulvectomy, may have an increased incidence of caesarean vulvar carcinoma are extremely uncommon, as the main delivery (2). In the literature, vulvar scarring following radical problem of subsequent pregnancy is vulvar scarring following vulvectomy was the major reason for pregnant women under- radical surgery. We herein report the case of a patient who was going caesarean section (2-7). To date, no cases of pregnancy diagnosed with stage I squamous cell carcinoma of the vulva following vulvar carcinoma have been reported in patients at the age of 17 years and was treated with multimodal therapy, who had undergone surgery and radiotherapy. including neoadjuvant chemotherapy, wide local excision with We herein describe a case in which caesarean section was bilateral inguinal lymph node dissection and adjuvant radio- performed due to the presence of extensive vulvar scarring therapy. The patient became pregnant spontaneously 9 years following multimodal therapy for vulvar carcinoma, including after her initial diagnosis and the antenatal course was good, chemotherapy, surgery and radiotherapy. -
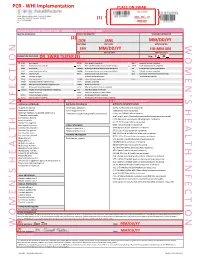
Womens Health Requisition Forms
PCR - WHI Implementation PLACE ON SWAB 10854 Midwest Industrial Blvd. St. Louis, MO 63132 MM DD YY Phone: (314) 200-3040 | Fax (314) 200-3042 (1) CLIA ID #26D0953866 JANE DOE v3 PCR MOLECULAR REQUISITION - WOMEN'S HEALTH INFECTION PRACTICE INFORMATION PATIENT INFORMATION *SPECIMEN INFORMATION (2) DOE JANE MM/DD/YY LAST NAME FIRST NAME DATE COLLECTED W O M E ' N S H E A L T H I F N E C T I O N SSN MM/DD/YY HH:MM AM SSN DATE OF BIRTH TIME COLLECTED REQUESTING PHYSICIAN: DR. SWAB TESTER (3) Sex: F X M (4) Diagnosis Codes X N76.0 Acute vaginitis B37.49 Other urogenital candidiasis A54.9 Gonococcal infection, unspecified N76.1 Subacute and chronic vaginitis N89.8 Other specified noninflammatory disorders of vagina A59.00 Urogenital trichomoniasis, unspecified N76.2 Acute vulvitis O99.820 Streptococcus B carrier state complicating pregnancy A64 Unspecified sexually transmitted disease N76.3 Subacute and chronic vulvitis O99.824 Streptococcus B carrier state complicating childbirth A74.9 Chlamydial infection, unspecified N76.4 Abscess of vulva B95.1 Streptococcus, group B, as the cause Z11.3 Screening for infections with a predmoninantly N76.5 Ulceration of vagina of diseases classified elsewhere sexual mode of trasmission N76.6 Ulceration of vulva Z22.330 Carrier of group B streptococcus Other: N76.81 Mucositis(ulcerative) of vagina and vulva N70.91 Salpingitis, unspecified N76.89 Other specified inflammation of vagina and vulva N70.92 Oophoritis, unspecified N95.2 Post menopausal atrophic vaginitis N71.9 Inflammatory disease of uterus, unspecified -

Female Perineum Doctors Notes Notes/Extra Explanation Please View Our Editing File Before Studying This Lecture to Check for Any Changes
Color Code Important Female Perineum Doctors Notes Notes/Extra explanation Please view our Editing File before studying this lecture to check for any changes. Objectives At the end of the lecture, the student should be able to describe the: ✓ Boundaries of the perineum. ✓ Division of perineum into two triangles. ✓ Boundaries & Contents of anal & urogenital triangles. ✓ Lower part of Anal canal. ✓ Boundaries & contents of Ischiorectal fossa. ✓ Innervation, Blood supply and lymphatic drainage of perineum. Lecture Outline ‰ Introduction: • The trunk is divided into 4 main cavities: thoracic, abdominal, pelvic, and perineal. (see image 1) • The pelvis has an inlet and an outlet. (see image 2) The lowest part of the pelvic outlet is the perineum. • The perineum is separated from the pelvic cavity superiorly by the pelvic floor. • The pelvic floor or pelvic diaphragm is composed of muscle fibers of the levator ani, the coccygeus muscle, and associated connective tissue. (see image 3) We will talk about them more in the next lecture. Image (1) Image (2) Image (3) Note: this image is seen from ABOVE Perineum (In this lecture the boundaries and relations are important) o Perineum is the region of the body below the pelvic diaphragm (The outlet of the pelvis) o It is a diamond shaped area between the thighs. Boundaries: (these are the external or surface boundaries) Anteriorly Laterally Posteriorly Medial surfaces of Intergluteal folds Mons pubis the thighs or cleft Contents: 1. Lower ends of urethra, vagina & anal canal 2. External genitalia 3. Perineal body & Anococcygeal body Extra (we will now talk about these in the next slides) Perineum Extra explanation: The perineal body is an irregular Perineal body fibromuscular mass. -

NVA Research Update E- Newsletter September – October – November 2016
NVA Research Update E- Newsletter September – October – November 2016 www.nva.org __________________________ Vulvodynia The Vulvar Pain Assessment Questionnaire inventory. Dargie E, Holden RR, Pukall CF. Pain. 2016 Aug 1. https://www.ncbi.nlm.nih.gov/pubmed/27780177 Millions suffer from chronic vulvar pain (ie, vulvodynia). Vulvodynia represents the intersection of 2 difficult subjects for health care professionals to tackle: sexuality and chronic pain. Those with chronic vulvar pain are often uncomfortable seeking help, and many who do so fail to receive proper diagnoses. The current research developed a multidimensional assessment questionnaire, the Vulvar Pain Assessment Questionnaire (VPAQ) inventory, to assist in the assessment and diagnosis of those with vulvar pain. A large pool of items was created to capture pain characteristics, emotional/cognitive functioning, physical functioning, coping skills, and partner factors. The item pool was subsequently administered online to 288 participants with chronic vulvar pain. Of those, 248 participants also completed previously established questionnaires that were used to evaluate the convergent and discriminant validity of the VPAQ. Exploratory factor analyses of the item pool established 6 primary scales: Pain Severity, Emotional Response, Cognitive Response, and Interference with Life, Sexual Function, and Self-Stimulation/Penetration. A brief screening version accompanies a more detailed version. In addition, 3 supplementary scales address pain quality characteristics, coping skills, and the impact on one's romantic relationship. When relationships among VPAQ scales and previously researched scales were examined, evidence of convergent and discriminant validity was observed. These patterns of findings are consistent with the literature on the multidimensional nature of vulvodynia. The VPAQ can be used for assessment, diagnosis, treatment formulation, and treatment monitoring. -

The Vulva Vaginal Diseases in Daily Practice Layout 1
Experimental & Clinical Article Gynecology; and Gynecologial Onncology The Vulva / Vaginal Diseases in Daily Practice Gamze S. ÇAĞLAR1, Elif D. ÖZDEMİR1, Sevim D. CENGİZ1, Handan DOĞAN2 Ankara, Turkey OBJECTIVE: To emphasize the neglected vulva/vaginal lesions and symptoms commonly encountered in daily practice. STUDY DESIGN: The data of 98 patients with vulva or vaginal biopsies were collected retrospectively. The histopathological diagnosis of 82(83.67%) vulvar and 16(16.32%) vaginal biopsy cases were eval- uated. RESULTS: The most common symptom was mass in 67% and 62% of cases in vulvar and vaginal re- gion, respectively. Among the vulvar lesions the most frequent histopathological diagnoses were condy- loma acuminatum (20.73%), hyperkeratotic papilloma (14.63%), non-spesific inflammatory changes (12.19%), fibroepithelial polyp (9.75%) and bartholin cyst (8.53%). On the other hand, the histopatolog- ical evaluation of the vaginal lesions revealed vaginal stromal polyp (25%) and gartner cyst (25%) as the most frequent lesions. CONCLUSIONS: The results of the study document lesions commonly not well known or disregarded by gynecologists. The literature is inconclusive about vulvavaginal diseases. Expanded data will help the clinicians in making correct diagnoses and patient managament. Key Words: Fibroepithelial polyp, Hyperkeratotic papilloma, Stromal polyp, Vaginal diseases, Vulvar diseases. Gynecol Obstet Reprod Med 2011;17:155-159 Introduction The clinicians should be aware of these physiological changes that will help in guiding the vulvar/vaginal symptoms Vulva is once called forgetten pelvic organ and related and disorders in daily clinical practice. There is limited data symptoms are usually considered as unimportant.1 The most about the most common reported histopathological diagnoses common compliants in women admitting to gynecology clin- and management in vulvavaginal diseases. -
Table of Contents
Society for Sex Therapy and Research SSTAR 2008: 33rd Annual Meeting Continuing Medical Education Credit is provided through joint sponsorship with The American College of Obstetricians and Gynecologists (ACOG). Intercontinental Hotel Chicago, Illinois USA March 13-15, 2008 TABLE OF CONTENTS President‘s Welcome ..........................................................................................................1 SSTAR 2009: 34th Annual Meeting – Arlington, Virginia, USA ........................................2 SSTAR 2008 Fall Clinical Meeting – New York, New York USA ....................................2 SSTAR Executive Council and Administrative Staff ..........................................................3 Continuing Education Accreditations & Approvals ............................................................5 Acknowledgements ..............................................................................................................6 Program Schedule ................................................................................................................7 2008 Award Recipients ....................................................................................................14 SSTAR Health Professional Book Award .............................................................14 Sex, Therapy, and Kids Recipient: Sharon Lamb, EdD SSTAR Service Award ..........................................................................................14 Recipient: Bill Maurice, MD SSTAR Student Research Award Abstract ............................................................15 -

Co™™I™™Ee Opinion
The American College of Obstetricians and Gynecologists WOMEN’S HEALTH CARE PHYSICIANS COMMITTEE OPINION Number 673 • September 2016 (Replaces Committee Opinion No. 345, October 2006) Committee on Gynecologic Practice This Committee Opinion was developed by the American College of Obstetricians and Gynecologists’ Committee on Gynecologic Practice and the American Society for Colposcopy and Cervical Pathology (ASCCP) in collaboration with committee member Ngozi Wexler, MD, MPH, and ASCCP members and experts Hope K. Haefner, MD, Herschel W. Lawson, MD, and Colleen K. Stockdale, MD, MS. This document reflects emerging clinical and scientific advances as of the date issued and is subject to change. The information should not be construed as dictating an exclusive course of treatment or procedure to be followed. Persistent Vulvar Pain ABSTRACT: Persistent vulvar pain is a complex disorder that frequently is frustrating to the patient and the clinician. It can be difficult to treat and rapid resolution is unusual, even with appropriate therapy. Vulvar pain can be caused by a specific disorder or it can be idiopathic. Idiopathic vulvar pain is classified as vulvodynia. Although optimal treatment remains unclear, consider an individualized, multidisciplinary approach to address all physical and emotional aspects possibly attributable to vulvodynia. Specialists who may need to be involved include sexual counselors, clinical psychologists, physical therapists, and pain specialists. Patients may perceive this approach to mean the practitioner does not believe their pain is “real”; thus, it is important to begin any treatment approach with a detailed discussion, including an explanation of the diagnosis and determination of realistic treatment goals. Future research should aim at evaluating a multimodal approach in the treatment of vulvodynia, along with more research on the etiologies of vulvodynia. -

September 2007
NVA RESEARCH UPDATE NEWSLETTER September 2007 www.nva.org This newsletter has been supported, in part, through a grant from the Enterprise Rent-A-Car Foundation. www.enterprise.com This newsletter is quarterly and contains abstracts from medical journals published between June and September 2007 (abstracts presented at scientific meetings may also be included). Please direct any comments regarding this newsletter to [email protected]. Vulvodynia / Pain The result of treatment on vestibular and general pain thresholds in women with provoked vestibulodynia. Bohm-Starke N, Brodda-Jansen G, Linder J, Danielsson I Clin J Pain. 2007 Sep;23(7):598-604 OBJECTIVE: To correlate changes in vestibular pain thresholds to general pain thresholds in a subgroup of women with provoked vestibulodynia taking part in a treatment study. METHODS: Thirty-five women with provoked vestibulodynia were randomized to 4 months' treatment with either electromyographic biofeedback (n=17) or topical lidocaine (n=18). Vestibular and general pressure pain thresholds (PPTs) were measured and the health survey Short Form-36 (SF-36) was filled out before treatment and at a 6- month follow-up. Subjective treatment outcome and bodily pain were analyzed. Thirty healthy women of the same age served as controls for general PPTs and SF-36. RESULTS: No differences in outcome measures were observed between the 2 treatments. Vestibular pain thresholds increased from median 30 g before to 70 g after treatment in the anterior vestibule (P<0.001) and from median 20 to 30 g in the posterior vestibule (P<0.001). PPTs on the leg and arm were lower in the patients as compared with controls both before and at the 6-month follow-up. -

Vulvar Pain Syndromes a Bounty of Treatments— but Not All of Them Are Proven
second of 3 parTs VulVar paIn syndroMes a bounty of treatments— but not all of them are proven Treatments for vulvodynia and vestibulodynia range from lifestyle adjustments and application of topical agents to tricyclic antidepressants and nerve blocks— but the data on their efficacy are not as bountiful neal M. lonky, Md, MpH, moderator; libby edwards, Md, Jennifer Gunter, Md, and Hope K. Haefner, Md, panelists s we discussed in the first installment vulva. Cool gel packs are sometimes helpful. of this three-part series in the Sep- In thIs When it comes to intercourse, I recom- Article A tember issue of OBG Management, mend adequate lubrication using any of a the causes of vulvar pain are many, and the number of effective products, such as olive Therapies discussed diagnosis of this common complaint can be oil, vitamin E oil, Replens, Slippery Stuff, As- by the panel difficult. Once the diagnosis of vulvodynia troglide, KY Liquid, and others. page 34 has been made, however, the challenge shifts There is an extensive list of lubricants at to finding an effective treatment. Here, our http://www.med.umich.edu/sexualhealth/ How to determine expert panel discusses the many options resources/guide.htm which treatments available, the data (or lack of it) behind each are best therapy, and what to do in refractory cases. In Part 3 of this series, in the November Topical agents might offer relief page 35 issue, the focus will be vestibulodynia. —but so might placebo Dr. Lonky: What is the role of topical medi- Is physical therapy cations, including anesthetics, for treating underrated? Management of vulvar pain vulvar pain syndromes? page 38 begins with simple measures Dr. -

The Clinical Role of LASER for Vulvar and Vaginal Treatments in Gynecology and Female Urology: an ICS/ISSVD Best Practice Consensus Document
Received: 30 November 2018 | Accepted: 3 January 2019 DOI: 10.1002/nau.23931 SOUNDING BOARD The clinical role of LASER for vulvar and vaginal treatments in gynecology and female urology: An ICS/ISSVD best practice consensus document Mario Preti MD1 | Pedro Vieira-Baptista MD2,3 | Giuseppe Alessandro Digesu PhD4 | Carol Emi Bretschneider MD5 | Margot Damaser PhD5,6,7 | Oktay Demirkesen MD8 | Debra S. Heller MD9 | Naside Mangir MD10,11 | Claudia Marchitelli MD12 | Sherif Mourad MD13 | Micheline Moyal-Barracco MD14 | Sol Peremateu MD12 | Visha Tailor MD4 | TufanTarcanMD15 | EliseJ.B.DeMD16 | Colleen K. Stockdale MD, MS17 1 Department of Obstetrics and Gynecology, University of Torino, Torino, Italy 2 Hospital Lusíadas Porto, Porto, Portugal 3 Lower Genital Tract Unit, Centro Hospitalar de São João, Porto, Portugal 4 Department of Urogynaecology, Imperial College Healthcare, London, UK 5 Center for Urogynecology and Pelvic Reconstructive Surgery, Obstetrics, Gynecology and Women's Health Institute, Cleveland Clinic, Cleveland, Ohio 6 Glickman Urological and Kidney Institute and Department of Biomedical Engineering Lerner Research Institute, Cleveland Clinic, Cleveland, Ohio 7 Advanced Platform Technology Center, Louis Stokes Cleveland VA Medical Center, Cleveland, Ohio 8 Faculty of Medicine, Department of Urology, Istanbul University Cerrahpaşa, Istanbul, Turkey 9 Department of Pathology and Laboratory Medicine, Rutgers-New Jersey Medical School, Newark, New Jersey 10 Kroto Research Institute, Department of Material Science and Engineering,