Obstetrics Healthcare Atlas
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
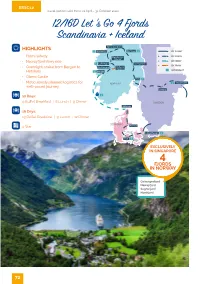
12/16D Let 'S Go 4 Fjords Scandinavia + Iceland
ESSC12 Travel period valid from 01 April - 31 October 2020 12/16D Let ’s Go 4 Fjords Scandinavia + Iceland eirangerfjord HIGHLIGHTS 1 Hornindal ombås 1 BY FLIGHT BY COACH • Flam railway Bøyabreen lacier BY FERRY • Nærøyfjord ferry ride 1 Leikanger illehammer BY TRAIN • Overnight cruise from Bergen to udvangen Aurland Tunnel OVERNIGHT Hirtshals 1 Bergen • Öbero Castle Oslo 1 • Meticulously planned logistics for NORWAY 1 Stockholm well-paced journey Örebro 12 Days: 1 9 Buffet Breakfast | 8 Lunch | 9 Dinner SN Hirtshals 16 Days: 13 Buffet Breakfast | 9 Lunch | 12 Dinner NMR 4 Star Aarhus Copenhagen 1 Fyn 1 EXCLUSIVELY IN SINGAPORE 4 FJORDS IN NORWAY Geirangerfjord Nærøyfjord Sognefjord Nordfjord 72 Day 01 Departure - Stockholm • Assemble at the airport for your long-haul flight to Stockholm, Sweden. Day 02 Stockholm Dinner • City Hall – Visit the Cathedral and Royal Palace. • Drottningholm Palace – Sweden’s best preserved royal palace constructed in the seventeenth century which is also the permanent resident of the royal family and one of Stockholm’s three World Heritage Sites. Stockholm Day 03 Stockholm - Örebro Castle - Oslo Buffet Breakfast | Lunch | Dinner • Örebro Castle – Photo stop at the castle that is surrounded by the river. • Transfer to Oslo via Karlstad. • Oslo City Tour – Visit the City Hall, Royal Palace and Oslo University with a photo stop at Vigeland Sculpture Park. Day 04 Oslo - Lillehammer - Dombås Buffet Breakfast | Lunch | Dinner • Lillehammer – Enjoy the breathtaking view along the way. • Lysgårdsbakkene – Photo stop at the Ski Jumping Arena. City Hall, Oslo Day 05 Dombås - Eagle Road - Geirangerfjord - Hornindal Buffet Breakfast | Lunch | Dinner • Eagle Road – Known for its name because at its highest point, it passed through terrain that had traditionally been the domain of a large number of eagles. -
Annual Report 2020
Annual Report Research Activity 2020 Division of Clinical Neuroscience University of Oslo and Oslo University Hospital 0 Contents Oslo University Hospital and the University of Oslo .................................................................................. 4 Division of Clinical Neuroscience .............................................................................................................. 4 Division of Clinical Neuroscience (NVR) Organizational Chart ................................................................... 5 Department of Physical Medicine and Rehabilitation Rehabilitation after trauma..................................................................................................................... 6 Group Leader: Nada Andelic Painful musculoskeletal disorders ........................................................................................................... 10 Group Leader: Cecilie Røe Department of Refractory Epilepsy - National Centre for Epilepsy Complex epilepsy ................................................................................................................................... 11 Group Leader: Morten Lossisus Department of Neurosurgery Neurovascular-Cerebrospinal Fluid Research Group ............................................................................. 17 Group Leader: Per Kristian Eide Oslo Neurosurgical Outcome Study Group (ONOSG) ................................................................................ 20 Group Leader: Eirik Helseth and Torstein Meling Vilhelm -
Detailed-Program-6Th-Ocher-2017
6th OCHER workshop on Clinical Communication Research January 11-13, 2017 The Oslo Communication in Healthcare Education and Research (OCHER) group The aims of OCHER workshops are two: 1) To provide a fruitful arena for discussion of research projects at all stages of development, with particular attention to challenges in methodology 2) To build a Scandinavian network (with international collaboration partners) of multidisciplinary researchers with interest in communication in health care Program Start: Wednesday 11 January, 10:00 End: Friday 13 January, 16:00 Venue: Thon Hotel Triaden, Lørenskog, Norway Address: Gamleveien 88 1476 Rasta Telephone: +47 66 10 97 00 Lecturers and group discussants: Professor J. Randall Curtis, University of Washington, Seattle, USA Keynote titles: - Measuring and improving communication about palliative care: What have we learned and where do we go from here? - Communication and decision-making with families of critically ill patients: Lessons from the successes and failures Professor Vikki Entwistle, University of Aberdeen, Scotland, UK Keynote titles: - Support for self-management among people with long-term conditions: re-formulating the concept to reflect and promote good practice - “How will we know if I’ve done a good job?” The challenges of evaluating person- centred care Local faculty: Pål Gulbrandsen, Arnstein Finset, and Jan Svennevig, University of Oslo, Hilde Eide, University College of Southeast Norway, Jennifer Gerwing, Akershus University Hospital Working languages: English, Scandinavian Page 1 of 36 Wednesday January 11 Time Activity Plenary room / Room A Room B 1000 Plenary Introduction, mutual presentation 1045 Break 1100 Plenary Vikki Entwistle Support for self-management keynote 1 among people with long-term conditions: re-formulating the concept to reflect and promote good practice 1230 Lunch 1315 Plenary J. -

NORE OG UVDAL KOMMUNE Næring, Miljø Og Kommunalteknikk
NORE OG UVDAL KOMMUNE Næring, miljø og kommunalteknikk LANDBRUKS- OG MATDEPARTEMENTET Postboks 8007 Dep 0030 OSLO Deres ref: Vår ref: Saksbeh: Arkivkode: Dato: 2017/1059 SLB - 31024613 V31 18.10.2017 Høringsuttalelse - Endringer i reglene om nydyrking - Forbud mot nydyrking av myr Vi viser til deres høringsbrev datert 11.7.2017. Hovedutvalg for næring, miljø og kommunalteknikk behandlet høringen i møte 12.10.2017 sak 74/17. Vedtak Hovedutvalg for næring, miljø og kommunalteknikk – 12.10.2017: «Generelt: Nore og Uvdal kommune stiller spørsmålstegn ved den strukturdrivende landbrukspolitikken som har blitt ført de siste årene, spesielt i forhold til at driftsbygninger bør ha tilstrekkelig arealgrunnlag. Det foreslåtte forbudet mot nydyrking av myr passer ikke inn i denne sammenhengen. Det påpekes også at den samfunnsøkonomiske besparelsen ved et slikt forbud bare er på kr 1 million for hele landet, og at dette er lite i forhold til den ulempen enkelte gårdbrukere får. Det meste av det dyrkbare arealet, inkludert dyrkbar myr, ligger i klimasoner som uansett ikke egner seg for kornproduksjon. Et forbud mot nydyrking av myr vil derfor i stor grad få negativ betydning for husdyrholdet og matproduksjonen i Norge. Dette momentet bør fremstilles bedre når Stortingsproposisjonen skal utarbeides. Jordlova: § 11 Drift av jordbruksareal, nydyrking og driftsvegar Ingen merknad. Nydyrkingsforskrifta: § 1 Formål Det vil være uheldig at § 3 fjerde ledd annet punktum om adkomst til bakenforliggende areal, ikke videreføres etter denne flyttingen. Dette er et viktig moment i vurderingen av søknader om godkjenning av plan for nydyrking, for å hindre at eksisterende ferdselsveier og større stier blir avskåret av innmark. -

Utviklingsprosjekt Ved Nordfjord Sjukehus
Utviklingsprosjekt ved Nordfjord sjukehus Analyse av pasientstraumar og forbruksrater i Nordfjordregionen Bruk av somatiske spesialisthelsetenester i kommunane Selje, Vågsøy, Eid, Hornindal, Stryn, Gloppen og Bremanger Deloitte AS Føresetnader og informasjon om datagrunnlaget i pasientstraumanalysen Analysane for 2010 er basert på 3 ulike datauttrekk. 1. DRG-gruppert NPR-melding (fra NPR) for alle pasientar i Helse Vest RHF, på HF-nivå pr kommune 2. DRG-gruppert uttrekk innhenta frå Helse Førde HF, dette for å få data på sjukehusnivå i føretaket 3. DRG gruppert uttrekk innhenta frå Helse Møre og Romsdal HF, over aktivitet på Volda og Mork for pasienter fra Nordfjord-regionen Det er et marginalt avvik mellom datagrunnlag for Helse Vest RHF og datagrunnlaget vi har motteke direkte frå Helse Førde HF. Helse Førde HF rapporterar 41 (+1,4 %) flere dagopphald og 49 (-0,9 %), færre døgnopphald og 4 (-0,01 %) færre polikliniske konsultasjonar enn dei «lukka» filane for Helse Vest RHF. Datagrunnlag for 2011 er basert på grupperte NPR-meldingar innhenta fra Helse Førde HF, samt Volda sjukehus og Mork rehabiliteringssenter Tellar-eininga i datagrunnlaget, er sjukehusopphald/konsultasjonar som inngår i ISF-ordninga. Aktivitet som inngår i ISF-grunnlaget er noko lavare enn den totale aktiviteten. For pasientar frå Nordfjord- regionene og ved sjukehusa Førde sentralsjukehus, Nordfjord sjukehus, Volda sjukehus og Mork rehabiliteringssenter, er avvika som følgjer: Døgnopphald 0,2% lavare, Dagopphold 1,3 % lavare og Polikliniske konsultasjoner 9,9% -

Delprosjekt Eidsvoll
Norges vassdrags- og energidirektorat Telefon: 22 95 95 95 Middelthunsgate 29 Telefaks: 22 95 90 00 Postboks 5091 Majorstua Internett: www.nve.no 0301 Oslo Flomsonekart Delprosjekt Eidsvoll Ahmed Reza Naserzadeh Julio Pereira 2 2007 FLOMSONEKART Flomsonekart nr 2/2007 Delprosjekt Eidsvoll Utgitt av: Norges vassdrags- og energidirektorat Forfattere: Ahmed Reza Naserzadeh Julio Pereira Trykk: NVEs hustrykkeri Opplag: 100 Forsidefoto: Sundet, vårflommen 10.06.1995 ©FOTONOR ISSN: 1504-5161 Emneord: Flomsone, flom, flomanalyse, flomareal, flomberegning, vannlinjeberegning, Vorma, Mjøsa, Eidsvoll kommune Norges vassdrags- og energidirektorat Middelthuns gate 29 Postboks 5091 Majorstua 0301 OSLO Telefon: 22 95 95 95 Telefaks: 22 95 90 00 Internett: www.nve.no Januar 2007 Sammendrag Rapporten inneholder detaljer rundt flomsonekartlegging av Vorma, fra Steinerud til Minnesund, en strekning på totalt ca 11 km. Området ligger i Eidsvoll kommune i Akershus. Grunnlaget for flomsonekartene er flomfrekvensanalyse og vannlinjeberegninger. Digitale flomsoner for 10-, 100-, 200-, og 500-årsflom dekker hele den kartlagte strekningen. I tillegg er det gitt vannstander for 20-, og 50-årsflom. Det er produsert flomsonekart for et område ved Minnesund og ved Sundet. Flomsonekart for 200-årsflommen samt flomdybdekart for 200-årsflommen ved Sundet er vedlagt rapporten. For at de beregnede flommene skal være mest mulig representative for fremtiden, er det valgt å betrakte perioden etter 1961, dvs. perioden etter de viktigste reguleringene fant sted. Det er derfor ikke tatt hensyn til flommer før 1961. Det er vårflommene som er de største både i Mjøsa og i Vorma. De fleste opptrer fra slutten av mai til midten av juli. Flom i Vorma innebærer en langsom vannstandsstigning på grunn av Mjøsa. -

How Uniform Was the Old Norse Religion?
II. Old Norse Myth and Society HOW UNIFORM WAS THE OLD NORSE RELIGION? Stefan Brink ne often gets the impression from handbooks on Old Norse culture and religion that the pagan religion that was supposed to have been in Oexistence all over pre-Christian Scandinavia and Iceland was rather homogeneous. Due to the lack of written sources, it becomes difficult to say whether the ‘religion’ — or rather mythology, eschatology, and cult practice, which medieval sources refer to as forn siðr (‘ancient custom’) — changed over time. For obvious reasons, it is very difficult to identify a ‘pure’ Old Norse religion, uncorroded by Christianity since Scandinavia did not exist in a cultural vacuum.1 What we read in the handbooks is based almost entirely on Snorri Sturluson’s representation and interpretation in his Edda of the pre-Christian religion of Iceland, together with the ambiguous mythical and eschatological world we find represented in the Poetic Edda and in the filtered form Saxo Grammaticus presents in his Gesta Danorum. This stance is more or less presented without reflection in early scholarship, but the bias of the foundation is more readily acknowledged in more recent works.2 In the textual sources we find a considerable pantheon of gods and goddesses — Þórr, Óðinn, Freyr, Baldr, Loki, Njo3rðr, Týr, Heimdallr, Ullr, Bragi, Freyja, Frigg, Gefjon, Iðunn, et cetera — and euhemerized stories of how the gods acted and were characterized as individuals and as a collective. Since the sources are Old Icelandic (Saxo’s work appears to have been built on the same sources) one might assume that this religious world was purely Old 1 See the discussion in Gro Steinsland, Norrøn religion: Myter, riter, samfunn (Oslo: Pax, 2005). -

Bremnes Seashore Joins Salmon Group
Press release 2020-10-26 Bremnes Seashore joins Salmon Group SALMA producer Bremnes Seashore today enters as shareholder in Salmon Group, a network of 41 fish farmers who emphasize local ownership and interaction with the local communities. Through the ownership, Bremnes Seashore also takes part in Salmon Group's innovative feed collaboration. - Salmon Group is very pleased to welcome a company who has such a good eye for the important drivers. Through a long period of conversations and discussion on important matters for us both, we are now well acquainted to each other. We are very confident that Bremnes Seashore is an aquaculture farmer who will fit well in our network, says Jan Olav Langeland, CEO of Salmon Group. - We have a common set of values with the other owners in Salmon Group, a group of salmon and trout farmers who are at the forefront of the development of sustainable farming. All companies will contribute to activity and jobs in the local communities along the coast. This makes us a good fit with the network, says Einar Eide, CEO of Bremnes Seashore. Common sustainability philosophy In recent years, Salmon Group has distinguished itself with its systematic and concrete work on sustainability. Based on their feasibility study "Sustainable farming of salmon and trout - What is that?", the network has been able to make specific adjustments of its own feed recipe. The changes are specific and have so far resulted in a 36% reduction in the carbon footprint from the production of salmon and trout that are fed with SG feed. - Salmon Group has taken major steps to reduce the footprint from feed production and transport and set the standard for sustainable feed for the aquaculture industry. -

Lasting Legacies
Tre Lag Stevne Clarion Hotel South Saint Paul, MN August 3-6, 2016 .#56+0).')#%+'5 6*'(7674'1(1742#56 Spotlights on Norwegian-Americans who have contributed to architecture, engineering, institutions, art, science or education in the Americas A gathering of descendants and friends of the Trøndelag, Gudbrandsdal and northern Hedmark regions of Norway Program Schedule Velkommen til Stevne 2016! Welcome to the Tre Lag Stevne in South Saint Paul, Minnesota. We were last in the Twin Cities area in 2009 in this same location. In a metropolitan area of this size it is not as easy to see the results of the Norwegian immigration as in smaller towns and rural communities. But the evidence is there if you look for it. This year’s speakers will tell the story of the Norwegians who contributed to the richness of American culture through literature, art, architecture, politics, medicine and science. You may recognize a few of their names, but many are unsung heroes who quietly added strands to the fabric of America and the world. We hope to astonish you with the diversity of their talents. Our tour will take us to the first Norwegian church in America, which was moved from Muskego, Wisconsin to the grounds of Luther Seminary,. We’ll stop at Mindekirken, established in 1922 with the mission of retaining Norwegian heritage. It continues that mission today. We will also visit Norway House, the newest organization to promote Norwegian connectedness. Enjoy the program, make new friends, reconnect with old friends, and continue to learn about our shared heritage. -

Norwegian Journal of Epidemiology Årgang 27, Supplement 1, Oktober 2017 Utgitt Av Norsk Forening for Epidemiologi
1 Norsk Epidemiologi Norwegian Journal of Epidemiology Årgang 27, supplement 1, oktober 2017 Utgitt av Norsk forening for epidemiologi Redaktør: Trond Peder Flaten EN NORSKE Institutt for kjemi, D 24. Norges teknisk-naturvitenskapelige universitet, 7491 Trondheim EPIDEMIOLOGIKONFERANSEN e-post: [email protected] For å bli medlem av Norsk forening for TROMSØ, epidemiologi (NOFE) eller abonnere, send e-post til NOFE: [email protected]. 7.-8. NOVEMBER 2017 Internettadresse for NOFE: http://www.nofe.no e-post: [email protected] WELCOME TO TROMSØ 2 ISSN 0803-4206 PROGRAM OVERVIEW 3 Opplag: 185 PROGRAM FOR PARALLEL SESSIONS 5 Trykk: NTNU Grafisk senter Layout og typografi: Redaktøren ABSTRACTS 9 Tidsskriftet er åpent tilgjengelig online: LIST OF PARTICIPANTS 86 www.www.ntnu.no/ojs/index.php/norepid Også via Directory of Open Access Journals (www.doaj.org) Utgis vanligvis med to regulære temanummer pr. år. I tillegg kommer supplement med sammendrag fra Norsk forening for epidemiologis årlige konferanse. 2 Norsk Epidemiologi 2017; 27 (Supplement 1) The 24th Norwegian Conference on Epidemiology Tromsø, November 7-8, 2017 We would like to welcome you to Tromsø and the 24th conference of the Norwegian Epidemiological Association (NOFE). The NOFE conference is an important meeting point for epidemiologists to exchange high quality research methods and findings, and together advance the broad research field of epidemiology. As in previous years, there are a diversity of topics; epidemiological methods, cardiovascular disease, diabetes, cancer, nutrition, female health, musculo-skeletal diseases, infection and behavioral epidemiology, all within the framework of this years’ conference theme; New frontiers in epidemiology. The conference theme reflects the mandate to pursue methodological and scientific progress and to be in the forefront of the epidemiological research field. -

Norway's 2018 Population Projections
Rapporter Reports 2018/22 • Astri Syse, Stefan Leknes, Sturla Løkken and Marianne Tønnessen Norway’s 2018 population projections Main results, methods and assumptions Reports 2018/22 Astri Syse, Stefan Leknes, Sturla Løkken and Marianne Tønnessen Norway’s 2018 population projections Main results, methods and assumptions Statistisk sentralbyrå • Statistics Norway Oslo–Kongsvinger In the series Reports, analyses and annotated statistical results are published from various surveys. Surveys include sample surveys, censuses and register-based surveys. © Statistics Norway When using material from this publication, Statistics Norway shall be quoted as the source. Published 26 June 2018 Print: Statistics Norway ISBN 978-82-537-9768-7 (printed) ISBN 978-82-537-9769-4 (electronic) ISSN 0806-2056 Symbols in tables Symbol Category not applicable . Data not available .. Data not yet available … Not for publication : Nil - Less than 0.5 of unit employed 0 Less than 0.05 of unit employed 0.0 Provisional or preliminary figure * Break in the homogeneity of a vertical series — Break in the homogeneity of a horizontal series | Decimal punctuation mark . Reports 2018/22 Norway’s 2018 population projections Preface This report presents the main results from the 2018 population projections and provides an overview of the underlying assumptions. It also describes how Statistics Norway produces the Norwegian population projections, using the BEFINN and BEFREG models. The population projections are usually published biennially. More information about the population projections is available at https://www.ssb.no/en/befolkning/statistikker/folkfram. Statistics Norway, June 18, 2018 Brita Bye Statistics Norway 3 Norway’s 2018 population projections Reports 2018/22 4 Statistics Norway Reports 2018/22 Norway’s 2018 population projections Abstract Lower population growth, pronounced aging in rural areas and a growing number of immigrants characterize the main results from the 2018 population projections. -

International Response to Infectious Salmon Anemia: Prevention, Control, and Eradication: Proceedings of a Symposium; 3Ð4 September 2002; New Orleans, LA
United States Department of Agriculture International Response Animal and Plant Health to Infectious Salmon Inspection Service Anemia: Prevention, United States Department of the Interior Control, and Eradication U.S. Geological Survey United States Department of Commerce National Marine Fisheries Service Technical Bulletin No. 1902 The U.S. Departments of Agriculture (USDA), the Interior (USDI), and Commerce prohibit discrimination in all their programs and activities on the basis of race, color, national origin, sex, religion, age, disability, political beliefs, sexual orientation, or marital or family status. (Not all prohibited bases apply to all programs.) Persons with disabilities who require alternative means for communication of program information (Braille, large print, audiotape, etc.) should contact USDA’s TARGET Center at (202) 720–2600 (voice and TDD). To file a complaint of discrimination, write USDA, Director, Office of Civil Rights, Room 326–W, Whitten Building, 1400 Independence Avenue, SW, Washington, DC 20250–9410 or call (202) 720–5964 (voice and TDD). USDA, USDI, and Commerce are equal opportunity providers and employers. The opinions expressed by individuals in this report do not necessarily represent the policies of USDA, USDI, or Commerce. Mention of companies or commercial products does not imply recommendation or endorsement by USDA, USDI, or Commerce over others not mentioned. The Federal Government neither guarantees nor warrants the standard of any product mentioned. Product names are mentioned solely to report factually on available data and to provide specific information. Photo credits: The background illustration on the front cover was supplied as a photo micrograph by Michael Opitz, of the University of Maine, and is reproduced by permission.