When Uncomplicated Childbirth Causes Permanent Nerve Damage
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Electrophysiological Study of the Posterior Cutaneous Femoral Nerve
logy & N ro eu u r e o N p h f y o s l i a o l n o Brooks, J Neurol Neurophysiol 2011, 2:5 r g u y o J Journal of Neurology & Neurophysiology ISSN: 2155-9562 DOI: 10.4172/2155-9562.1000119 Research Article Article OpenOpen Access Access Electrophysiological Study of the Posterior Cutaneous Femoral Nerve: Normative Data Brooks1*, Silva C MD2, Kai MR2 and Leal GXP2 1Setor de Eletroneuromiografia do Instituto de Assistência à Saúde do Servidor Público Estadual de São Paulo – São Paulo- Brasil 2Hospital do Servidor Publico Estadual de São Paulo, São Paulo, Brazil Abstract The posterior cutaneous femoral nerve provides cutaneous inervation of the posterior surface of the thigh and leg, as well as the skin of the perineum. Using Dumitru et al. [1] technique for the assessment of this nerve, we studied one hundred and sixteen limbs from fifty-eight healthy volunteers. The mean values for the posterior cutaneous femoral nerve were as follows: onset latency 2.0 msec (±0.5), amplitude 7.0µV (±2.1), nerve conduction velocity 52 m/s (±4). The assessment of the posterior femoral cutaneous nerve is simple and reproducible. The results of this standardization were similar to the ones described in international literature. Keywords: Femoral nerve; Posterior cutaneous nerve Results Introduction The mean values for the posterior cutaneous femoral nerve were as follows: onset latency 2.0msec (±0.5), amplitude 7.0µV (±2,1), nerve The posterior cutaneous nerve of the thigh leaves the pelvis through conduction velocity 52 m/s (±4); Table 1 summarizes our findings. -

Lower Extremity Focal Neuropathies
LOWER EXTREMITY FOCAL NEUROPATHIES Lower Extremity Focal Neuropathies Arturo A. Leis, MD S.H. Subramony, MD Vettaikorumakankav Vedanarayanan, MD, MBBS Mark A. Ross, MD AANEM 59th Annual Meeting Orlando, Florida Copyright © September 2012 American Association of Neuromuscular & Electrodiagnostic Medicine 2621 Superior Drive NW Rochester, MN 55901 Printed by Johnson Printing Company, Inc. 1 Please be aware that some of the medical devices or pharmaceuticals discussed in this handout may not be cleared by the FDA or cleared by the FDA for the specific use described by the authors and are “off-label” (i.e., a use not described on the product’s label). “Off-label” devices or pharmaceuticals may be used if, in the judgment of the treating physician, such use is medically indicated to treat a patient’s condition. Information regarding the FDA clearance status of a particular device or pharmaceutical may be obtained by reading the product’s package labeling, by contacting a sales representative or legal counsel of the manufacturer of the device or pharmaceutical, or by contacting the FDA at 1-800-638-2041. 2 LOWER EXTREMITY FOCAL NEUROPATHIES Lower Extremity Focal Neuropathies Table of Contents Course Committees & Course Objectives 4 Faculty 5 Basic and Special Nerve Conduction Studies of the Lower Limbs 7 Arturo A. Leis, MD Common Peroneal Neuropathy and Foot Drop 19 S.H. Subramony, MD Mononeuropathies Affecting Tibial Nerve and its Branches 23 Vettaikorumakankav Vedanarayanan, MD, MBBS Femoral, Obturator, and Lateral Femoral Cutaneous Neuropathies 27 Mark A. Ross, MD CME Questions 33 No one involved in the planning of this CME activity had any relevant financial relationships to disclose. -
Current Overview of Neurovascular Structures in Hip Arthroplasty
1mon.qxd 2/2/04 10:26 AM Page 73 REVIEW Current Overview of Neurovascular Structures in Hip Arthroplasty: Anatomy, Preoperative Evaluation, Approaches, and Operative Techniques to Avoid Complications John-Paul H. Rue, MD* Nozomu Inoue, MD, PhD* Michael A. Mont, MD† A major neurovascular injury during total hip arthroplasty (THA) is uncom- Educational Objectives mon. Nevertheless, these are worri- some due to their devastating conse- As a result of reading this article, physicians should be able to: quences. As more THAs are performed 1. Identify the bony, vascular, and neural anatomy that is relevant to the each year, the chances of this potential- surgeon performing total hip arthroplasty. ly life- or limb-threatening injury 2. Describe the common approaches to avoid neurovascular complica- increase.1 It is crucial for the orthope- tions. dic surgeon to have a thorough under- 3. Discuss the appropriate clinical work-up of these patients. standing of the anatomy of the region 4. Describe the various neurovascular complications and how to handle and the potential complications. them. This article reviews the exposures to the acetabulum for simple and complex primary THA, as well as revision cases, with particular attention to the neu- ischium, and pubis (Figure 1). The Damage to any of these vessels by rovascular anatomy of the region. acetabulum is located at the junction of retraction, drilling, reaming, or dissec- these three bones. These bones unite tion can cause massive hemorrhage, ANATOMY anteriorly at the pubic symphysis and which can lead to exsanguination with- Bone posteriorly to the sacrum to form a ring in minutes. -

A Cadaveric Study of Ultrasound-Guided Subpectineal Injectate Spread Around the Obturator Nerve and Its Hip Articular Branches
REGIONAL ANESTHESIA AND ACUTE PAIN Regional Anesthesia & Pain Medicine: first published as 10.1097/AAP.0000000000000587 on 1 May 2017. Downloaded from ORIGINAL ARTICLE A Cadaveric Study of Ultrasound-Guided Subpectineal Injectate Spread Around the Obturator Nerve and Its Hip Articular Branches Thomas D. Nielsen, MD,* Bernhard Moriggl, MD, PhD, FIACA,† Kjeld Søballe, MD, DMSc,‡ Jens A. Kolsen-Petersen, MD, PhD,* Jens Børglum, MD, PhD,§ and Thomas Fichtner Bendtsen, MD, PhD* such high-volume blocks the most appropriate nerve blocks for Background and Objectives: The femoral and obturator nerves are preoperative analgesia in patients with hip fracture, because both assumed to account for the primary nociceptive innervation of the hip joint the femoral and obturator nerves have been found to innervate capsule. The fascia iliaca compartment block and the so-called 3-in-1-block the hip joint capsule.5 have been used in patients with hip fracture based on a presumption that local Several authors have since questioned the reliability of the anesthetic spreads to anesthetize both the femoral and the obturator nerves. FICB and the 3-in-1-block to anesthetize the obturator nerve.6–10 Evidence demonstrates that this presumption is unfounded, and knowledge Recently, a study, using magnetic resonance imaging to visualize about the analgesic effect of obturator nerve blockade in hip fracture patients the spread of the injectate, refuted any spread of local anesthetic to presurgically is thus nonexistent. The objectives of this cadaveric study were the obturator nerve after either of the 2 nerve block techniques.11 to investigate the proximal spread of the injectate resulting from the admin- Consequently, knowledge of the analgesic effect of an obturator istration of an ultrasound-guided obturator nerve block and to evaluate the nerve block in preoperative patients with hip fracture is nonexis- spread around the obturator nerve branches to the hip joint capsule. -

The Muscles That Act on the Lower Limb Fall Into Three Groups: Those That Move the Thigh, Those That Move the Lower Leg, and Those That Move the Ankle, Foot, and Toes
MUSCLES OF THE APPENDICULAR SKELETON LOWER LIMB The muscles that act on the lower limb fall into three groups: those that move the thigh, those that move the lower leg, and those that move the ankle, foot, and toes. Muscles Moving the Thigh (Marieb / Hoehn – Chapter 10; Pgs. 363 – 369; Figures 1 & 2) MUSCLE: ORIGIN: INSERTION: INNERVATION: ACTION: ANTERIOR: Iliacus* iliac fossa / crest lesser trochanter femoral nerve flexes thigh (part of Iliopsoas) of os coxa; ala of sacrum of femur Psoas major* lesser trochanter --------------- T – L vertebrae flexes thigh (part of Iliopsoas) 12 5 of femur (spinal nerves) iliac crest / anterior iliotibial tract Tensor fasciae latae* superior iliac spine gluteal nerves flexes / abducts thigh (connective tissue) of ox coxa anterior superior iliac spine medial surface flexes / adducts / Sartorius* femoral nerve of ox coxa of proximal tibia laterally rotates thigh lesser trochanter adducts / flexes / medially Pectineus* pubis obturator nerve of femur rotates thigh Adductor brevis* linea aspera adducts / flexes / medially pubis obturator nerve (part of Adductors) of femur rotates thigh Adductor longus* linea aspera adducts / flexes / medially pubis obturator nerve (part of Adductors) of femur rotates thigh MUSCLE: ORIGIN: INSERTION: INNERVATION: ACTION: linea aspera obturator nerve / adducts / flexes / medially Adductor magnus* pubis / ischium (part of Adductors) of femur sciatic nerve rotates thigh medial surface adducts / flexes / medially Gracilis* pubis / ischium obturator nerve of proximal tibia rotates -
Femoral Nerve Blocks
Femoral Nerve Blocks Julie Ronnebaum, DPT, GCS, CEEAA Objectives 1. Become familiar with the evolution of peripheral nerve blocks. 2. Describe the advantages and disadvantages of femoral nerve blocks 3. Identify up-to-date information on the use of femoral nerve block. 4. Recognize future implications. History of Anesthesia The use of anesthetics began over 160 years ago. General Anesthesia In 1845, Horace Wells used nitrous oxide gas during a tooth extraction 1st- public introduction of general anesthesia October 16, 1846. Known as “Ether Day” ( William Morton) In front of audience at Massachusetts General Hospital First reported deat h in 1847 due to the ether Other complications Inttouctoroduction to eteteher was ppoogerolonged Vomiting for hours to days after surgery Schatsky, 1995, Hardy, 2001 History of Anesthesia In 1874, morphine introduced as a pain killer. In 1884, August Freund discovers cy clopropane for surgery Problem is it is very flammable In 1898, heroin was introduced for the addiction to morphine In 1923 Arno Luckhardt administered ethylene oxygen for an anesthetic History of Anesthesia Society History of Anesthesia Alternatives to general anesthesia In the 1800’s Cocaine used by the Incas and Conquistadors 1845, Sir Francis Rynd applied a morphine solution directly to the nerve to relieve intractable neuralgg(ia. ( first recorded nerve block) Delivered it by gravity into a cannula In 1855, Alexander Wood is a glass syringe to deliver the medication for a nerve block. ( also known as regg)ional anesthesia) In 1868 a Peruvian surgeon discovered that if you inject cocaine into the skin it numbed it. In 1884, Karl Koller discovered cocaine could be used to anesthetized the eye of a frog. -

Intercostal, Ilioinguinal, and Iliohypogastric Nerve Transfers for Lower Limb Reinnervation After Spinal Cord Injury: an Anatomical Feasibility and Experimental Study
LABORATORY INVESTIGATION J Neurosurg Spine 30:268–278, 2019 Intercostal, ilioinguinal, and iliohypogastric nerve transfers for lower limb reinnervation after spinal cord injury: an anatomical feasibility and experimental study *Ahmed A. Toreih, MD,1 Asser A. Sallam, MD, PhD,1 Cherif M. Ibrahim, MD,2 Ahmed I. Maaty, MD,3 and Mohsen M. Hassan4 Departments of 1Orthopedic Surgery and Trauma and 3Physical Medicine, Rheumatology, and Rehabilitation, Suez Canal University Hospitals; 2Department of Anatomy, Suez Canal University; and 4Department of Surgery, Anesthesiology, and Radiology, Faculty of Veterinary Medicine, Suez Canal University, Ismailia, Egypt OBJECTIVE Spinal cord injury (SCI) has been investigated in various animal studies. One promising therapeutic ap- proach involves the transfer of peripheral nerves originating above the level of injury into those originating below the level of injury. The purpose of the present study was to evaluate the feasibility of nerve transfers for reinnervation of lower limbs in patients suffering SCI to restore some hip and knee functions, enabling them to independently stand or even step forward with assistive devices and thus improve their quality of life. METHODS The feasibility of transferring intercostal to gluteal nerves and the ilioinguinal and iliohypogastric nerves to femoral nerves was assessed in 5 cadavers. Then, lumbar cord hemitransection was performed below L1 in 20 dogs, followed by transfer of the 10th, 11th, and 12th intercostal and subcostal nerves to gluteal nerves and the ilioinguinal and iliohypogastric nerves to the femoral nerve in only 10 dogs (NT group). At 6 months, clinical and electrophysiological evaluations of the recipient nerves and their motor targets were performed. -
A Systematic Review and Meta-Analysis of the Hip Capsule Innervation and Its Clinical Implications
www.nature.com/scientificreports OPEN A systematic review and meta‑analysis of the hip capsule innervation and its clinical implications Joanna Tomlinson1*, Benjamin Ondruschka2, Torsten Prietzel3,5, Johann Zwirner1,2 & Niels Hammer4,5,6* Detailed understanding of the innervation of the hip capsule (HC) helps inform surgeons’ and anaesthetists’ clinical practice. Post‑interventional pain following radiofrequency nerve ablation (RFA) and dislocation following total hip arthroplasty (THA) remain poorly understood, highlighting the need for more knowledge on the topic. This systematic review and meta‑analysis focuses on gross anatomical studies investigating HC innervation. The main outcomes were defned as the prevalence, course, density and distribution of the nerves innervating the HC and changes according to demographic variables. HC innervation is highly variable; its primary nerve supply seems to be from the nerve to quadratus femoris and obturator nerve. Many articular branches originated from muscular branches of the lumbosacral plexus. It remains unclear whether demographic or anthropometric variables may help predict potential diferences in HC innervation. Consequently, primary targets for RFA should be the anterior inferomedial aspect of the HC. For THA performed on non‑risk patients, the posterior approach with capsular repair appears to be most appropriate with the lowest risk of articular nerve damage. Care should also be taken to avoid damaging vessels and muscles of the hip joint. Further investigation is required to form a coherent map of HC innervation, utilizing combined gross and histological investigation. When performing total hip arthroplasty (THA), one philosophy of orthopedic surgeons aiming to preserve and repair the hip joint capsule (HC) is to spare the surrounding muscles and surrounding tissue, in turn this may also spare the articular branches of nerves supplying the HC 1,2. -

Unilateral Variant Psoas Major with Split Femoral Nerve
S Journal of O p s e s n Acce Anatomy and Physiological Studies CASE REPORT Unilateral Variant Psoas Major with Split Femoral Nerve Tiraj Parikh*1, Caleb Parry1, Marina Motina1, Shahana Momin1, Rebecca Mickle1, Peter Nguyen1, Aaron Perez1, Cara Fisher PhD2 1Texas College of Osteopathic Medicine 2Center for Anatomical Sciences, University of North Texas Health Science Center Introduction [4]. Psoas tertius is described as a slip of muscle originating from the inner half of the 12th rib and transverse processes of The psoas major muscle includes slips of muscle that originate lumbar vertebrae 1-4 and attaching to the iliopsoas muscle [5]. from the transverse processes of lumbar vertebrae 1-5 and Another study describes their findings of an accessory psoas intervertebral discs of T12-L4. These slips of muscle combine major muscle originating on the left costal process of L3 and and join with the iliacus muscle to then course inferiorly and the intertransverse ligament between L3 and L4 [6]. Although insert onto the lesser trochanter of the femur [1].The psoas rare, these variants have also been shown to split the femoral muscle is considered one of the primary flexors of the hip nerve. It has been proposed that this occurrence is associated joint and is innervated by the femoral nerve, which arises with neuropathies. [5-9]. from ventral rami of lumbar spinal nerves 2-4. The femoral nerve then passes through the psoas major in an inferolateral Case Presentation direction until it emerges on the lateral border of the muscle Here we present a novel variant of the psoas major muscle. -

Fascicular Anatomy of Human Femoral Nerve: Implications for Neural Prostheses Using Nerve Cuff Electrodes
Volume 46, Number 7, 2009 JRRDJRRD Pages 973–984 Journal of Rehabilitation Research & Development Fascicular anatomy of human femoral nerve: Implications for neural prostheses using nerve cuff electrodes Kenneth J. Gustafson, PhD;1–2* Gilles C. J. Pinault, MD;2–3 Jennifer J. Neville, MD;4 Ishaq Syed, MD;4 John A. Davis Jr, MD;5 Jesse Jean-Claude, MD;2–3 Ronald J. Triolo, PhD1–2,5 1Department of Biomedical Engineering, Case Western Reserve University, Cleveland, OH; 2Louis Stokes Cleveland Department of Veterans Affairs Medical Center, Cleveland, OH; 3Department of Surgery, 4School of Medicine, and 5Department of Orthopedics, Case Western Reserve University, Cleveland, OH Abstract—Clinical interventions to restore standing or stepping ing or walking after paralysis resulting from upper motor by using nerve cuff stimulation require a detailed knowledge of neuron damage secondary to spinal cord injury (SCI), or femoral nerve neuroanatomy. We harvested eight femoral nerves peripheral nerve damage due to trauma, require a detailed with all distal branches and characterized the branching patterns knowledge of the morphology and fascicular anatomy of the and diameters. The fascicular representation of each distal nerve femoral nerve. However, the fascicular anatomy and spe- was identified and traced proximally to create fascicle maps of the cific dimensions of the human femoral nerve have not been compound femoral nerve in four cadaver specimens. Distal nerves fully described and must be quantitatively documented. were consistently represented as individual fascicles or distinct groups of fascicles in the compound femoral nerve. Branch-free The femoral nerve originates from the second, third, length of the compound femoral nerve was 1.50 +/– 0.47 cm and fourth lumbar spinal nerves and innervates the anterior (mean +/– standard deviation). -

Anatomical Variations of Accessory Obturator Nerve
International Journal of Anatomy and Research, Int J Anat Res 2016, Vol 4(2):2158-61. ISSN 2321-4287 Original Research Article DOI: http://dx.doi.org/10.16965/ijar.2016.168 ANATOMICAL VARIATIONS OF ACCESSORY OBTURATOR NERVE: A CADAVERIC STUDY WITH PROPOSED CLINICAL IMPLICATIONS Archana B.J *1, Nagaraj D.N 2, Pradeep P 3, Lakshmi Prabha Subhash 4. *1 Assistant Professor, Department of Anatomy, Sri Siddhartha Medical College, Tumkur, Karnataka, India. 2 Professor, Department of Anatomy, Sri Siddhartha Medical College, Tumkur, Karnataka, India. 3 Senior Resident, Department of Orthopaedics, Sri Siddhartha Medical College, Tumkur, Karnataka, India. 4 Professor and Head, Department of Anatomy, Sri Siddhartha Medical College, Tumkur, Karnataka, India. ABSTRACT Background: The accessory obturator nerve arises from the ventral branches of the third and fourth lumbar ventral rami. It is occasionally present in 10% of population. It descends along the medial border of psoas major, crosses the superior pubic ramus and divides into branches supplying the hip joint and pectineus. There is a high degree of variability in its formation. It may arise from the ventral rami of second and third lumbar nerves or second, third and fourth lumbar nerves or from third lumbar nerve alone. Sometimes the accessory obturator nerve is very small and supplies only pectineus. Any branch may be absent . Knowledge of these variations is important for surgeries of hip joint and in evaluation of groin pain. Aim: The aim of this study was to evaluate the incidence and variation in the formation of accessory obturator nerve and to analyse the variability of the frequency of this nerve, reported in the literature and to discuss its clinical implications. -
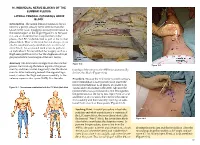
Chapter 16 – Individual Nerve Blocks of the Lumbar Plexus
16. INDIVIDUAL NERVE BLOCKS OF THE LUMBAR PLEXUS LATERAL FEMORAL CUTANEOUS NERVE BLOCK Introduction. The lateral femoral cutaneous (LFC) nerve is a purely sensory nerve derived from the L2–L3 nerve roots. It supplies sensory innervation to the lateral aspect of the thigh (Figure 16-1). Because it is one of six nerves that comprise the lumbar plexus, the LFC can be blocked as part of the lumbar plexus block. Most of the time, but not always, it can also be simultaneously anesthetized via a femoral nerve block. An occasional need arises to perform an individual LFC nerve block for surgery such as a thigh skin graft harvest or for the diagnosis of myal- gia paresthetica (a neuralgia of the LFC nerve). Anatomy. The LFC nerve emerges from the lumbar Figure 16-2 Figure 16-3 plexus, travels along the lateral aspect of the psoas muscle, and then crosses diagonally over the iliacus tionship of the nerve to the ASIS that anatomically muscle. After traversing beneath the inguinal liga- defines this block (Figure 16-2). ment, it enters the thigh and passes medially to the anterior superior iliac spine (ASIS). It is the rela- Procedure. Because the LFC nerve is purely sensory, nerve stimulation is not typically used. Insert the needle perpendicular to all planes at a point 2 cm Figure 16-1. Dermatomes anesthetized with the LFC block (dark blue) caudal and 2 cm medial to the ASIS. Advance the needle until a loss-of-resistance is felt; this signifies the penetration of the fascia lata. Inject 5 mL of local anesthetic at this location, then redirect the needle first medially and then laterally, injecting an addi- tional 5 mL at each of these points (Figure 16-3).