Botulinum Toxin a and Osteosarcopenia in Experimental Animals: a Scoping Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Local Control of Human Umbilical Vessel Tone
LOCAL CONTROL OF HUMAN UMBILICAL VESSEL TONE. Thesis submitted to the University of London for the degree of Doctor of Philosophy in the Faculty of Science. by Anita-Jane Sexton B.Sc. (Hons.) Department of Anatomy and Developmental Biology University College London. ProQuest Number: 10017796 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a complete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. uest. ProQuest 10017796 Published by ProQuest LLC(2016). Copyright of the Dissertation is held by the Author. All rights reserved. This work is protected against unauthorized copying under Title 17, United States Code. Microform Edition © ProQuest LLC. ProQuest LLC 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106-1346 ABSTRACT This thesis examines the influence of the vascular endothelium on the local control of human feto-placental vascular tone and how these influences may vary with gestation. Electron microscopic studies have revealed that human umbilical vessels are devoid of nerves throughout gestation. Structural changes in the arterial and venous wall could be detected throughout gestation. The presence of a subpopulation of endothelial cells containing nitric oxide synthase (NOS)-like immunoreactivity was identified only in late pregnancy. The umbilical artery and vein, from both early and late pregnancy, did not relax to acetylcholine (ACh), adenosine 5-triphosphate (ATP), substance P (SP) and calcium ionophore A23187, known to be endothelium-dependent vasodilators, but did relax to sodium nitroprusside (SNP). -
Surgical Challenges in Complex Primary Total Hip Arthroplasty
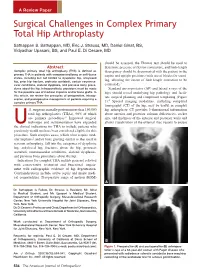
A Review Paper Surgical Challenges in Complex Primary Total Hip Arthroplasty Sathappan S. Sathappan, MD, Eric J. Strauss, MD, Daniel Ginat, BS, Vidyadhar Upasani, BS, and Paul E. Di Cesare, MD should be assessed, the Thomas test should be used to Abstract determine presence of flexion contracture, and limb-length Complex primary total hip arthroplasty (THA) is defined as discrepancy should be documented with the patient in the primary THA in patients with compromised bony or soft-tissue supine and upright positions (with use of blocks for stand- states, including but not limited to dysplastic hip, ankylosed hip, prior hip fracture, protrusio acetabuli, certain neuromus- ing, allowing the extent of limb-length correction to be 3 cular conditions, skeletal dysplasia, and previous bony proce- estimated). dures about the hip. Intraoperatively, provisions must be made Standard anteroposterior (AP) and lateral x-rays of the for the possible use of modular implants and/or bone grafts. In hips should reveal underlying hip pathology and facili- this article, we review the principles of preoperative, intraop- tate surgical planning and component templating (Figure erative, and postoperative management of patients requiring a 4 complex primary THA. 1). Special imaging modalities, including computed tomography (CT) of the hip, may be useful in complex .S. surgeons annually perform more than 150,000 hip arthroplasty. CT provides 3-dimensional information total hip arthroplasties (THAs), 90% of which about anterior and posterior column deficiencies, socket are primary procedures.1 Improved surgical size, and thickness of the anterior and posterior walls and technique and instrumentation have expanded allows visualization of the external iliac vessels to ensure Uthe clinical indications for THA to include patients who previously would not have been considered eligible for this procedure. -

Tonic and Rhythmic Spinal Activity Underlying Locomotion
Send Orders for Reprints to [email protected] Current Pharmaceutical Design, 2017, 23, 1-11 1 REVIEW ARTICLE Tonic and Rhythmic Spinal Activity Underlying Locomotion Yury P. Ivanenkoa,*, Victor S. Gurfinkelb, Victor A. Selionovc, Irina A. Solopovac, Francesca Sylos-Labinid, Pierre A Guertine and Francesco Lacquanitia,d,f aLaboratory of Neuromotor Physiology, Santa Lucia Foundation, 00179 Rome, Italy; bBiomedical Engineering Department, Oregon Health and Science University, Portland, Oregon, USA; cLaboratory of Neurobiology of Motor Control, Institute for Information Transmission Problems, Moscow 127994, Russia; dCentre of Space Bio-medicine, University of Rome Tor Vergata, 00133 Rome, Italy, City, Country; eDepartment of Psychiatry and Neurosciences, Laval University, Québec City, Canada G1V 4G2; fDepartment of Systems Medicine, University of Rome Tor Vergata, 00133 Rome, Italy Abstract: In recent years, many researches put significant efforts into understanding and assessing the functional state of the spinal locomotor circuits in humans. Various techniques have been developed to stimulate the spinal A R T I C L E H I S T O R Y cord circuitries, which may include both diffuse and quite specific tuning effects. Overall, the findings indicate that tonic and rhythmic spinal activity control are not separate phenomena but are closely integrated to properly initiate and sustain stepping. The spinal cord does not simply transmit information to and from the brain. Its Received: November 2, 2016 Accepted: January 20, 2017 physiologic state determines reflex, postural and locomotor control and, therefore, may affect the recovery of the locomotor function in individuals with spinal cord and brain injuries. This review summarizes studies that exam- ine the rhythmogenesis capacity of cervical and lumbosacral neuronal circuitries in humans and its importance in DOI: 10.2174/1381612823666170125 developing central pattern generator-modulating therapies. -

Cerebral Palsy
Cerebral Palsy Cerebral palsy encompasses a group of non-progressive and non-contagious motor conditions that cause physical disability in various facets of body movement. Cerebral palsy is one of the most common crippling conditions of childhood, dating to events and brain injury before, during or soon after birth. Cerebral palsy is a debilitating condition in which the developing brain is irreversibly damaged, resulting in loss of motor function and sometimes also cognitive function. Despite the large increase in medical intervention during pregnancy and childbirth, the incidence of cerebral palsy has remained relatively stable for the last 60 years. In Australia, a baby is born with cerebral palsy about every 15 hours, equivalent to 1 in 400 births. Presently, there is no cure for cerebral palsy. Classification Cerebral palsy is divided into four major classifications to describe different movement impairments. Movements can be uncontrolled or unpredictable, muscles can be stiff or tight and in some cases people have shaky movements or tremors. These classifications also reflect the areas of the brain that are damaged. The four major classifications are: spastic, ataxic, athetoid/dyskinetic and mixed. In most cases of cerebral palsy, the exact cause is unknown. Suggested possible causes include developmental abnormalities of the brain, brain injury to the fetus caused by low oxygen levels (asphyxia) or poor circulation, preterm birth, infection, and trauma. Spastic cerebral palsy leads to increased muscle tone and inability for muscles to relax (hypertonic). The brain injury usually stems from upper motor neuron in the brain. Spastic cerebral palsy is classified depending on the region of the body affected; these include: spastic hemiplegia; one side being affected, spastic monoplegia; a single limb being affected, spastic triplegia; three limbs being affected, spastic quadriplegia; all four limbs more or less equally affected. -

Back-To-Basics: the Intricacies of Muscle Contraction
Back-to- MIOTA Basics: The CONFERENCE OCTOBER 11, Intricacies 2019 CHERI RAMIREZ, MS, of Muscle OTRL Contraction OBJECTIVES: 1.Review the anatomical structure of a skeletal muscle. 2.Review and understand the process and relationship between skeletal muscle contraction with the vital components of the nervous system, endocrine system, and skeletal system. 3.Review the basic similarities and differences between skeletal muscle tissue, smooth muscle tissue, and cardiac muscle tissue. 4.Review the names, locations, origins, and insertions of the skeletal muscles found in the human body. 5.Apply the information learned to enhance clinical practice and understanding of the intricacies and complexity of the skeletal muscle system. 6.Apply the information learned to further educate clients on the importance of skeletal muscle movement, posture, and coordination in the process of rehabilitation, healing, and functional return. 1. Epithelial Four Basic Tissue Categories 2. Muscle 3. Nervous 4. Connective A. Loose Connective B. Bone C. Cartilage D. Blood Introduction There are 3 types of muscle tissue in the muscular system: . Skeletal muscle: Attached to bones of skeleton. Voluntary. Striated. Tubular shape. Cardiac muscle: Makes up most of the wall of the heart. Involuntary. Striated with intercalated discs. Branched shape. Smooth muscle: Found in walls of internal organs and walls of vascular system. Involuntary. Non-striated. Spindle shape. 4 Structure of a Skeletal Muscle Skeletal Muscles: Skeletal muscles are composed of: • Skeletal muscle tissue • Nervous tissue • Blood • Connective tissues 5 Connective Tissue Coverings Connective tissue coverings over skeletal muscles: .Fascia .Tendons .Aponeuroses 6 Fascia: Definition: Layers of dense connective tissue that separates muscle from adjacent muscles, by surrounding each muscle belly. -

1 Human Resting Muscle Tone
Human Resting Muscle Tone (HRMT): Narrative Introduction and Modern Concepts Alfonse T. Masi, MD, DR.P.H. * Professor of Medicine and Epidemiology University of Illinois College of Medicine at Peoria One Illini Drive, Peoria, IL 61656, USA Tel: +1 309 671 8428 Fax: +1 309 671 8513 Email: [email protected] John Charles Hannon, DC Certified Feldenkrais Practitioner 1141 Pacific Suite B San Luis Obispo, CA 93401, USA Tel: +1 805 542 9925 Fax: +1 805 541 2391 Email: [email protected] Key Words: passive tone or tonus; viscoelastic; skeletal muscle; fascia; myofascial, biotensegrity *Correspondence to: Dr. AT Masi 1 Abstract Human resting muscle studies have been performed to establish (myofascial) tone (HRMT) is the passive normal frequency distributions of degrees of tonus or tension of skeletal muscle that myofascial tone. Clinical experience derives from its intrinsic (EMG-silent) indicates that persons with certain molecular viscoelastic properties. The word symptomatic musculoskeletal conditions tone has been used to convey varying may have palpably increased resting muscle clinical and physiological features that have firmness or hardness (EMG-silent), such as led to confusion and controversy. HRMT is that of the upper trapezius in tension-type the vital low-level, passive tension, and headache, and the lumbodorsal extensors resistance to stretch that contributes (hartspann) in degenerative lumbar disc importantly to maintaining postural stability disease and ankylosing spondylitis. in balanced equilibrium positions. In contrast, co-contraction of muscle is an In summary, resting skeletal muscle tone is active neuromotor control that provides an intrinsic viscoelastic tension exhibited greater levels of tonus for increased within the body’s kinematic chains. -

Rule 17, Exhibit 1
RULE 17, EXHIBIT 1 Low Back Pain Medical Treatment Guidelines Revised: February 3, 2014 Effective: March 30, 2014 Adopted: March 24, 1993 Effective: April 30, 1993 Revised: March 11, 1994 Effective: April 30, 1994 Revised: January 9, 1995 Effective: March 2, 1995 Revised: January 8, 1998 Effective: March 15, 1998 Revised: October 4, 2001 Effective: December 1, 2001 Revised: September 29, 2005 Effective: January 1, 2006 Revised: April 26, 2007 Effective: July 1, 2007 Presented by: State of Colorado Department of Labor and Employment DIVISION OF WORKERS' COMPENSATION TABLE OF CONTENTS SECTION DESCRIPTION PAGE A. INTRODUCTION .............................................................................................................................. 1 B. GENERAL GUIDELINE PRINCIPLES ............................................................................................ 2 1. APPLICATION OF GUIDELINES ....................................................................................... 2 2. EDUCATION ....................................................................................................................... 2 3. INFORMED DECISION MAKING ....................................................................................... 2 4. TREATMENT PARAMATER DURATION ........................................................................... 2 5. ACTIVE INTERVENTIONS ................................................................................................. 2 6. ACTIVE THERAPEUTIC EXERCISE PROGRAM ............................................................. -

Muscle Physiology Dr
Muscle Physiology Dr. Ebneshahidi Copyright © 2004 Pearson Education, Inc., publishing as Benjamin Cummings Skeletal Muscle Figure 9.2 (a) Copyright © 2004 Pearson Education, Inc., publishing as Benjamin Cummings Functions of the muscular system . 1. Locomotion . 2. Vasoconstriction and vasodilatation- constriction and dilation of blood vessel Walls are the results of smooth muscle contraction. 3. Peristalsis – wavelike motion along the digestive tract is produced by the Smooth muscle. 4. Cardiac motion . 5. Posture maintenance- contraction of skeletal muscles maintains body posture and muscle tone. 6. Heat generation – about 75% of ATP energy used in muscle contraction is released as heat. Copyright. © 2004 Pearson Education, Inc., publishing as Benjamin Cummings . Striation: only present in skeletal and cardiac muscles. Absent in smooth muscle. Nucleus: smooth and cardiac muscles are uninculcated (one nucleus per cell), skeletal muscle is multinucleated (several nuclei per cell ). Transverse tubule ( T tubule ): well developed in skeletal and cardiac muscles to transport calcium. Absent in smooth muscle. Intercalated disk: specialized intercellular junction that only occurs in cardiac muscle. Control: skeletal muscle is always under voluntary control‚ with some exceptions ( the tongue and pili arrector muscles in the dermis). smooth and cardiac muscles are under involuntary control. Copyright © 2004 Pearson Education, Inc., publishing as Benjamin Cummings Innervation: motor unit . a) a motor nerve and a myofibril from a neuromuscular junction where gap (called synapse) occurs between the two structures. at the end of motor nerve‚ neurotransmitter (i.e. acetylcholine) is stored in synaptic vesicles which will release the neurotransmitter using exocytosis upon the stimulation of a nerve impulse. Across the synapse the surface the of myofibril contains receptors that can bind with the neurotransmitter. -

Cerebral Palsy
Cerebral Palsy What is Cerebral Palsy? Doctors use the term cerebral palsy to refer to any one of a number of neurological disorders that appear in infancy or early childhood and permanently affect body movement and muscle coordination but are not progressive, in other words, they do not get worse over time. • Cerebral refers to the motor area of the brain’s outer layer (called the cerebral cortex), the part of the brain that directs muscle movement. • Palsy refers to the loss or impairment of motor function. Even though cerebral palsy affects muscle movement, it is not caused by problems in the muscles or nerves. It is caused by abnormalities inside the brain that disrupt the brain’s ability to control movement and posture. In some cases of cerebral palsy, the cerebral motor cortex has not developed normally during fetal growth. In others, the damage is a result of injury to the brain either before, during, or after birth. In either case, the damage is not repairable and the disabilities that result are permanent. Patients with cerebral palsy exhibit a wide variety of symptoms, including: • Lack of muscle coordination when performing voluntary movements (ataxia); • Stiff or tight muscles and exaggerated reflexes (spasticity); • Walking with one foot or leg dragging; • Walking on the toes, a crouched gait, or a “scissored” gait; • Variations in muscle tone, either too stiff or too floppy; • Excessive drooling or difficulties swallowing or speaking; • Shaking (tremor) or random involuntary movements; and • Difficulty with precise motions, such as writing or buttoning a shirt. The symptoms of cerebral palsy differ in type and severity from one person to the next, and may even change in an individual over time. -

By Request: a Discussion About Carnitine
Aunt Cathy’s Guide to Nutrition: Sanford Medical Center 12-2015 By Request: A Discussion about Carnitine The role of supplemental carnitine in conditions characterized by excessive obesity, hunger, lethargy, hypotonia, and poor exercise endurance. Aunt Cathy Cathy Breedon PhD, RD, CSP, FADA Clinical and Metabolic Nutrition Specialist / Prenatal/Pediatric Nutrition Specialist Sanford Medical Center, and Clinical Associate Professor UND School of Medicine, Fargo, ND Carnitine is a substance we normally make in the liver, kidney and brain. It is also available in small amounts in meats. It is a tiny substance made from a molecule of methionine and a molecule of lysine — two essential amino acids that we need to make all of our body’s protein. Carnitine plays a critical role in the ability to burn fat for fuel because it is part of the enzyme system "carnitine palmitoyl transferase" which transfers fat molecules into the mitochondria to produce energy as ATP. This picture of a logging truck illustrates the role of carnitine if you imagine the long trees as long chains of fat. Carnitine “trucks” are needed to get the fat into the saw mill to cut it up into small enough bits to go into the furnace. [The sign on the door of the truck says that it is the “Cart-It-In Trucking Company” to help remember that one very important function of carnitine is to cart fat (the fuel) into the mitochondria (the furnace) to convert it to energy we can use.] 1 Muscle (including heart muscle and the diaphragm) is very dependent on fat fuels for aerobic energy production. -

Active and Passive Characteristics of Muscle Tone and Their Relationship Models of Subluxation/Joint Dysfunction Part I
0008-3194/2003/168–179/$2.00/©JCCA 2003 Muscle tone Active and passive characteristics of muscle tone and their relationship models of subluxation/joint dysfunction Part I Gary A Knutson, DC* Edward F Owens, Jr., MS, DC** The relationship of muscles to the causes and effects of La relation entre les muscles et les causes et effets de the pathophysiologic entity referred to as chiropractic l’entité physiopathologique renvoyant à une subluxation subluxation or joint dysfunction is critical. Part I of this ou à un dysfonctionnement des articulations s’avère paper reviews complexities of skeletal muscle in regards particulièrement critique. La première partie de ce texte to anatomy, active and passive tone, detection of muscle examine la complexité des muscles du squelette au tone, neurophysiology, and how muscle function fits into regard de l’anatomie, de la tonicité active et passive, de a variety of subluxation/joint dysfunction models. The la détection de la tonicité musculaire, de la review culminates in Part II with a hypothesis to neurophysiologie et du fonctionnement des muscles par describe and explain varying degrees of muscle tone rapport à une variété de modèles de subluxation ou de that may be encountered clinically. It is hoped that dysfonctionnement des articulations. Dans la deuxième knowledge of the differing levels of muscle tone and their partie du texte, une hypothèse est formulée pour décrire causes will help the clinician to better determine the et expliquer les divers degrés de tonicité musculaire qui underlying cause of a neuro-musculoskeletal problem peuvent être rencontrés en clinique. Il est à souhaiter allowing application of necessary and proper que la connaissance des différents degrés de tonicité intervention. -

Hypertonicity in Children with Cerebral Palsy: a New Perspective
Iranian Rehabilitation Journal, Vol. 9, December 2011 Review Hypertonicity in Children with Cerebral Palsy: a New Perspective Mehdi Rassafiani, PhD Pediatric Neurorehabilitation Research Center, Department of Occupational Therapy, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran Robab Sahaf*; MD, PhD Iranian Research Center on Aging, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran Objectives: Hypertonicity is a major problem in children with cerebral palsy that has not been explained effectively to address clinical decision making. Therefore, this article aims to provide a theoretical framework about hypertonicity for clinicians, rehabilitation and medical practitioners to be used in their practice. Methods: Literature was reviewed to examine the new perspectives towards the hypertonicity and its signs and symptoms. Then, these symptoms were scrutinized to identify various aspects of the phenomena. Results: The results of this review revealed various components of hypertonicity, including neural and biomechanical. Neural component was also classified into positive and negative symptoms. These components altogether influence gross and fine motor function and consequently disturb children in their daily activities. Conclusion: Using term “spasticity” is not definitively enough to explain various aspects of the affected persons. Therefore, the term “hypertonicity” appears to be much appropriate to be used by professions in their daily practices. Furthermore, to have a very effective intervention, practitioners should consider all various signs and symptoms of hypertonicity that are explained in this review. Key words: Hypertonicity, Cerebral palsy, Children Introduction Cerebral Palsy As individuals with cerebral palsy (CP) present a large Cerebral palsy is the most common cause of group of clients visited by occupational therapists, movement disorders in children (6-8).