Open the Guidelines for Febrile Neutropenia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Infection Control for Neutropenic Cancer Patients : the Libraryuse of Prophylactic Antibiotics Lecture Author Jean A
Infection control for neutropenic cancer patients : the Libraryuse of prophylactic antibiotics Lecture author Jean A. Klastersky Onlineby Institut Jules Bordet,© Université Libre de Bruxelles (ULB) Brussels, Belgium ESCMID Complications and mortality associated with febrile neutropenia Library No Bacteremia Bacteremia Total ComplicationsLectureDeaths Total Complications Deaths author Solid tumors 784 60 (8 %) 25 135 30 (22 %) 17 Onlineby (3 %) (13 % ) © Hematological cancer 859 111 (13 %) 32 364 76 (21 %) 32 (4 %) (9 %) ESCMID J. Klastersky et al., 2007 2 Complications associated with febrile neutropenia Library Hypotension : systolic blood pressure less than 90 mmHg or need for pressor support to maintain blood pressure Respiratory failure : arterial oxygen pressure less than 60mmHg while breathing room air or needLecture for mechanical ventilation Disseminated intravascular coagulation Confusion or altered mental state author Congestive cardiac failure seen on chest X-ray and requiring treatment Onlineby Bleeding severe enough to require© transfusion Arrhythmia or ECG changes requiring treatment Renal failure requiring investigation and/or treatment with IV fluids, dialysis, or any other intervention ESCMID J. Klastersky et al., 2000 3 Cost of febrile neutropenia Library Initial hospitalization Initial hospitalization plus all downstreamLecture neutropenia care author 2.010 $ Onlineby 14.407 $ © ESCMID D. Weyckler et al., 2008 4 Use of oral antibiotics in protected units environment : clinical effectiveness and role in the emergence -

Neutropenia Fact Sheet
Neutropenia in Barth Syndrome i ii (Chronic, Cyclic or Intermittent) What problems can Neutropenia cause? Neutrophils are the main white blood cell for fighting or preventing bacterial or fungal infections. They may be referred to as polymorphonuclear cells (polys or PMNs), white cells with segmented nuclei (segs), or neutrophils in the complete blood cell count (CBC) report. Immature neutrophils are referred to as bands. When someone is neutropenic (an abnormally low level of neutrophils in the blood), the risk of infection increases. The absolute neutrophil count (ANC) is a measure of the total number of neutrophils present in the blood. When the ANC is less than 1,000, the risk of infection increases. Most infections occur in the ears, skin or throat and to a lesser extent, the chest. These infections can be very serious and may require antibiotics to clear infections. When someone with Barth syndrome is neutropenic his defenses are weakened, he is likely to become seriously ill more quickly than someone with a normal neutrophil count. Tips: • No rectal temperatures as any break in the skin can lead to an infection. • If the individual has a temperature > 100.4° F (38° C) or has infectious symptoms, the primary physician or hematologist should be notified. The individual may need to be seen. • If the individual has a temperature of 100.4° F (38° C) – 100.5° F (38.05° C)> 8 hours or a temperature > 101.5° F (38.61° C), an immediate examination by the physician is warranted. Some or all of the following studies may be ordered: CBC with differential and ANC Urinalysis Blood, urine, and other appropriate cultures C-Reactive Protein Echocardiogram if warranted • The physician may suggest antibiotics (and G-CSF if the ANC is low) for common infections such as otitis media, stomatitis. -

Hodgkin Lymphoma Treatment Regimens
HODGKIN LYMPHOMA TREATMENT REGIMENS (Part 1 of 5) Clinical Trials: The National Comprehensive Cancer Network recommends cancer patient participation in clinical trials as the gold standard for treatment. Cancer therapy selection, dosing, administration, and the management of related adverse events can be a complex process that should be handled by an experienced health care team. Clinicians must choose and verify treatment options based on the individual patient; drug dose modifications and supportive care interventions should be administered accordingly. The cancer treatment regimens below may include both U.S. Food and Drug Administration-approved and unapproved indications/regimens. These regimens are provided only to supplement the latest treatment strategies. These Guidelines are a work in progress that may be refined as often as new significant data become available. The NCCN Guidelines® are a consensus statement of its authors regarding their views of currently accepted approaches to treatment. Any clinician seeking to apply or consult any NCCN Guidelines® is expected to use independent medical judgment in the context of individual clinical circumstances to determine any patient’s care or treatment. The NCCN makes no warranties of any kind whatsoever regarding their content, use, or application and disclaims any responsibility for their application or use in any way. Classical Hodgkin Lymphoma1 Note: All recommendations are Category 2A unless otherwise indicated. Primary Treatment Stage IA, IIA Favorable (No Bulky Disease, <3 Sites of Disease, ESR <50, and No E-lesions) REGIMEN DOSING Doxorubicin + Bleomycin + Days 1 and 15: Doxorubicin 25mg/m2 IV push + bleomycin 10units/m2 IV push + Vinblastine + Dacarbazine vinblastine 6mg/m2 IV over 5–10 minutes + dacarbazine 375mg/m2 IV over (ABVD) (Category 1)2-5 60 minutes. -

R-Eshap Patient Information Leaflet Keep All Medicine
R-ESHAP PATIENT HE-I- INFORMATION 049 LEAFLET KEEP ALL MEDICINE OUT OF THE SIGHT AND REACH OF CHILDREN R-ESHAP What is R-ESHAP? R-ESHAP is the name of a combination of cancer drugs used to treat non Hodgkin’s lymphoma (NHL). R-ESHAP is ESHAP chemotherapy with the drug rituximab. Rituximab is a type of biological therapy called a monoclonal antibody. R-ESHAP is made up of the drugs • R = Rituximab (Mabthera) • E = Etoposide - a chemotherapy drug • SH = Methylprednisolone, which is a steroid • A = Cytarabine (also known as Ara C) – a chemotherapy drug • P = Cisplatin – a chemotherapy drug How you have R-ESHAP • All the R-ESHAP drugs are clear colourless fluids. You have them into your bloodstream (intravenously). You can have them through a central line, a portacath. These are long, plastic tubes that give the drugs directly into a large vein in your chest. You have the tube put in just before your course of treatment starts and it stays in place as long as you need it. • You usually have R-ESHAP as cycles of treatment. Each cycle lasts 4 weeks. You usually have between 2 and 8 cycles. • Each cycle of treatment is given in the following way. o On the first day you have ▪ Rituximab as a slow drip (infusion) before all the other drugs – see details below ▪ Etoposide as a drip for 1 hour ▪ Methylprednisolone (steroid) as a drip for 15 to 30 minutes ▪ Cytarabine as a drip for 2 hours – this may be on the fifth day instead ▪ Cisplatin as a drip that lasts for 96 hours (4 days) o On the second, third and fourth days you ▪ Continue with your cisplatin ▪ Repeat the etoposide and methylprednisolone drips ▪ On the fifth day the cisplatin finishes and you have ▪ Another dose of methylprednisolone ▪ Another dose of cytarabine • You have no treatment for just over 3 weeks. -

Vancomycin-Resistant Enterococci Colonization in Patients with Hematological Malignancies: Screening and Its Cost-Effectiveness
Vancomycin-resistant enterococci colonization in patients with hematological malignancies: screening and its cost-effectiveness Gedik Habip1, Şimşek Funda1, Kantürk Arzu1, Yıldırmak Taner1, Arıca Deniz2, Aydın Demet2, Yokuş Osman2, Demirel Naciye2 1. Department of Infectious Diseases and Clinical Microbiology, Ministry of Health Okmeydanı Training and Research Hospital, Istanbul 2. Department of Hematology, Ministry of Health Okmeydanı Training and Research Hospital, Istanbul Abstract: Background and objective: We evaluated the rates of vancomycin-resistant enterococci (VRE) colonization and VRE- related bacteremia in patients with hematological malignancies in terms of routine screening culture and its cost-effective- ness. Materials and Methods: All patients of the hematology department who were older than 14 years of age and who devel- oped at least one febrile neutropenia episode during chemotherapy for hematological cancers between November 2010 and November 2012 were evaluated retrospectively. Results: We retrospectively analyzed 282 febrile episodes in 126 neutropenic patients during a two-year study period. The study included 65 cases in the first study-year and 78 cases in the second study-year. The numbers of colonization days and colonized patient were748 days of colonization in 29 patients (44%) in the first study-year and 547 colonization days in 21 patients (26%) in the second study-year, respectively. Routine screening culture for VRE cost $4516,4 (427 cultures) in the first study-year, $5082,7 (504 cultures) in the second study-year depending on the number of patients and their length of stay. Conclusion: In line with our study results, routine screening of hematological patients for VRE colonization is not cost- effective. Routine surveillance culture for VRE should be considered with respect to the conditions of health care setting. -

Neonatal Leukopenia and Thrombocytopenia
Neonatal Leukopenia and Thrombocytopenia Vandy Black, M.D., M.Sc., FAAP March 3, 2016 April 14, 2011 Objecves • Summarize the differenHal diagnosis of leukopenia and/or thrombocytopenia in a neonate • Describe the iniHal steps in the evaluaon of a neonate with leukopenia and/or thrombocytopenia • Review treatment opHons for leukopenia and/ or thrombocytopenia in the NICU Clinical Case 1 • One day old male infant admiUed to the NICU for hypoglycemia and a sepsis rule out • Born at 38 weeks EGA by SVD • Birth weight 4 lbs 13 oz • Exam shows a small cephalohematoma; no dysmorphic features • PLT count 42K with an otherwise normal CBC Definions • Normal WBC count 9-30K at birth – Mean 18K • What is the ANC and ALC – <1000/mm3 is abnormal – 6-8% of infants in the NICU • Normal platelet count: 150-450,000/mm3 – Not age dependent – 22-35% of infants in the NICU have plts<150K Neutropenia Absolute neutrophil count <1500/mm3 Category ANC* InfecHon risk • Mild 1000-1500 None • Moderate 500-1000 Minimal • Severe <500 Moderate to Severe (Highest if <200) • Recurrent bacterial or fungal infecHons are the hallmark of symptomac neutropenia! • *ANC = WBC X % (PMNs + Bands) / 100 DefiniHon of Neutropenia Black and Maheshwari, Neoreviews 2009 How to Approach Cytopenias • Normal vs. abnormal (consider severity) • Malignant vs. non-malignant • Congenital vs. acquired • Is the paent symptomac • Transient, recurrent, cyclic, or persistent How to Approach Cytopenias • Adequate vs. decreased marrow reserve • Decreased producHon vs. increased destrucHon/sequestraon Decreased neutrophil/platelet producon • Primary – Malignancy/leukemia/marrow infiltraon – AplasHc anemia – Genec disorders • Secondary – InfecHous – Drug-induced – NutriHonal • B12, folate, copper Increased destrucHon/sequestraon • Immune-mediated • Drug-induced • Consumpon à Hypersplenism vs. -

Enterococcal Bacteremia in Febrile Neutropenic Children and Adolescents with Underlying Malignancies, and Clinical Impact of Vancomycin Resistance
Infection (2019) 47:417–424 https://doi.org/10.1007/s15010-018-1260-z ORIGINAL PAPER Enterococcal bacteremia in febrile neutropenic children and adolescents with underlying malignancies, and clinical impact of vancomycin resistance Kil‑Seong Bae1,2 · Ju Ae Shin1 · Seong koo Kim1,3 · Seung Beom Han1,2 · Jae Wook Lee1,3 · Dong‑Gun Lee2,3,4 · Nack‑Gyun Chung1,3 · Bin Cho1,3 · Dae Chul Jeong1,2 · Jin Han Kang1,2 Received: 28 August 2018 / Accepted: 15 December 2018 / Published online: 19 December 2018 © Springer-Verlag GmbH Germany, part of Springer Nature 2018 Abstract Purpose Enterococci are a common cause of bacteremia in immunocompromised patients. Although the increase of van- comycin-resistant enterococci (VRE) makes appropriate antibiotic therapy difficult, clinical characteristics of enterococcal bacteremia and the impact of VRE infection on outcomes have rarely been reported in immunocompromised children. Methods We enrolled children and adolescents (< 19 years of age) with underlying malignancies who were diagnosed with enterococcal bacteremia during febrile neutropenia between 2010 and 2017. Medical records of the enrolled children were retrospectively reviewed to evaluate the clinical characteristics of enterococcal bacteremia and impact of VRE infection on outcomes. Results Thirty-six episodes of enterococcal bacteremia were identified in 30 patients. VRE infection was identified in 11 epi- sodes (30.6%); the 7- and 30-day mortalities were 27.8% and 44.4%, respectively. Acute lymphoblastic leukemia (50.0%) and acute myeloid leukemia (30.6%) were the most common underlying disorders. Three (8.3%) of the patients were in complete remission, and palliative and reinduction chemotherapies were administered in 47.2% and 36.1% of episodes, respectively. -

Neutropenia : an Analysis of the Risk Factors for Infection Steven Ira Rosenfeld Yale University
Yale University EliScholar – A Digital Platform for Scholarly Publishing at Yale Yale Medicine Thesis Digital Library School of Medicine 1980 Neutropenia : an analysis of the risk factors for infection Steven Ira Rosenfeld Yale University Follow this and additional works at: http://elischolar.library.yale.edu/ymtdl Recommended Citation Rosenfeld, Steven Ira, "Neutropenia : an analysis of the risk factors for infection" (1980). Yale Medicine Thesis Digital Library. 3087. http://elischolar.library.yale.edu/ymtdl/3087 This Open Access Thesis is brought to you for free and open access by the School of Medicine at EliScholar – A Digital Platform for Scholarly Publishing at Yale. It has been accepted for inclusion in Yale Medicine Thesis Digital Library by an authorized administrator of EliScholar – A Digital Platform for Scholarly Publishing at Yale. For more information, please contact [email protected]. NEUTROPENIA: AN ANALYSIS OF THE RISK FACTORS FOR INFECTION by Steven Ira Rosenfeld B.A. Johns Hopkins University 1976 A Thesis Submitted to The Yale University School of Medicine In Partial Fulfillment of the Requirements for the Degree of Doctor of Medicine 1980 Med Li^> Ya ABSTRACT The risk factors for infection were evaluated retrospectively in 107 neutropenic patients without underlying malignancy or cyto¬ toxic drug therapy. Neutrophil count was an independent risk factor for infection, with the incidence of infection increasing as the neutrophil count decreased. The critical neutrophil count, below which the incidence of infection was significantly increased was 250/mnr*, (p<.001). Eighty five percent of the <250 group entered with, or developed infection. Additional risk factors for infection included increased duration of neutropenia, age less than 1 year old, male sex, hypogammaglobulinemia, and recent antibiotic therapy. -

Febrile Neutropenia Intro Hi Everyone, My Name Is Dr. Chris
PedsCases Podcast Scripts This is a text version of a podcast from Pedscases.com on “Febrile Neutropenia.” These podcasts are designed to give medical students an overview of key topics in pediatrics. The audio versions are accessible on iTunes or at www.pedcases.com/podcasts. Febrile Neutropenia Developed by Chris Novak, and Dr. Bev Wilson for PedsCases.com. January 27, 2016 Intro Hi everyone, my name is Dr. Chris Novak. I’m a pediatric resident at the Stollery Children’s Hospital at the University of Alberta. Today’s podcast is designed to give an organized approach to febrile neutropenia in children. This podcast was developed with Dr. Bev Wilson, a pediatric oncologist and Professor at the University of Alberta and in Edmonton, Alberta. Let’s start with a clinical case. You are on an emergency medicine rotation in a peripheral hospital. You sign up to see Hakim, a 4-year-old male with a fever, measured 38.9oC at triage. Upon entering the room Hakim’s parents quickly tell you that he is being treated with outpatient chemotherapy for acute lymphoblastic leukemia, and that his oncology team told the family to go to emergency immediately if he develops a fever. You recognize that Hakim is at risk for febrile neutropenia. What do you need to consider when assessing this patient? What time-sensitive investigations and therapies need to be initiated? We will come back to the case of Hakim as an example as we go through the podcast. In the neutropenic patient, a fever can be an ominous sign of a serious infection. -

Approved Amendment 2 07 May 2019 Confidentiality Notice This Document Contains Confidential Information of Amgen Inc
Product: Blinatumomab Protocol Number: 20150292 Date: 07 May 2019 Page 1 of 115 Title: A Phase 2/3 Multi-center Study to Evaluate the Safety and Efficacy of Blinatumomab in Subjects With Relapsed/Refractory Aggressive B-Cell Non Hodgkin Lymphoma Amgen Protocol Number (Product Name: Blinatumomab) 20150292 EudraCT number 2016‐002044‐16 Clinical Study Sponsor: Amgen Inc. One Amgen Center Drive Thousand Oaks, California 91320 United States Phone: +1-805-447-1000 Fax: +1-805-480-4978 Key Sponsor Contact(s): Clinical Research Medical Director Email: Global Clinical Trial Manager Phone: Email: Date: 27 June 2016 Amendment 1 16 March 2017 Superseding Amendment 1: 27 April 2017 Approved Amendment 2 07 May 2019 Confidentiality Notice This document contains confidential information of Amgen Inc. This document must not be disclosed to anyone other than the site study staff and members of the institutional review board/independent ethics committee/institutional scientific review board or equivalent. The information in this document cannot be used for any purpose other than the evaluation or conduct of the clinical investigation without the prior written consent of Amgen Inc. If you have questions regarding how this document may be used or shared, call the Amgen Medical Information number: US sites, 1- 800-77-AMGEN, Canadian sites, 1-866-50-AMGEN; <<for all other countries, insert the local toll-free Medical Information number>> Amgen’s general number in the US (1-805-447-1000). NCT Number: NCT02910063 This NCT number has been applied to the document for purposes of posting on Clinical trials.gov CONFIDENTIAL Product: Blinatumomab Protocol Number: 20150292 Date: 07 May 2019 Page 2 of 115 Investigator’s Agreement I have read the attached protocol entitled “A Phase 2/3 Multi-center Study to Evaluate the Safety and Efficacy of Blinatumomab in Subjects with Relapsed/Refractory Aggressive B-Cell Non Hodgkin Lymphoma,” dated 07 May 2019 and agree to abide by all provisions set forth therein. -

Recent Advances in Oligonucleotide Therapeutics in Oncology
International Journal of Molecular Sciences Review Recent Advances in Oligonucleotide Therapeutics in Oncology Haoyu Xiong 1, Rakesh N. Veedu 2,3 and Sarah D. Diermeier 1,* 1 Department of Biochemistry, University of Otago, Dunedin 9016, New Zealand; [email protected] 2 Centre for Molecular Medicine and Innovative Therapeutics, Murdoch University, Perth 6150, Australia; [email protected] 3 Perron Institute for Neurological and Translational Science, Perth 6009, Australia * Correspondence: [email protected] Abstract: Cancer is one of the leading causes of death worldwide. Conventional therapies, including surgery, radiation, and chemotherapy have achieved increased survival rates for many types of cancer over the past decades. However, cancer recurrence and/or metastasis to distant organs remain major challenges, resulting in a large, unmet clinical need. Oligonucleotide therapeutics, which include antisense oligonucleotides, small interfering RNAs, and aptamers, show promising clinical outcomes for disease indications such as Duchenne muscular dystrophy, familial amyloid neuropathies, and macular degeneration. While no approved oligonucleotide drug currently exists for any type of cancer, results obtained in preclinical studies and clinical trials are encouraging. Here, we provide an overview of recent developments in the field of oligonucleotide therapeutics in oncology, review current clinical trials, and discuss associated challenges. Keywords: antisense oligonucleotides; siRNA; aptamers; DNAzymes; cancers Citation: Xiong, H.; Veedu, R.N.; 1. Introduction Diermeier, S.D. Recent Advances in Oligonucleotide Therapeutics in According to the Global Cancer Statistics 2018, there were more than 18 million new Oncology. Int. J. Mol. Sci. 2021, 22, cancer cases and 9.6 million deaths caused by cancer in 2018 [1]. -
ESHAP and R-ESHAP
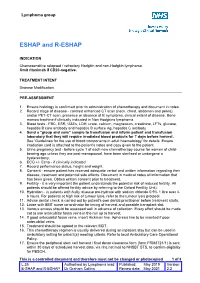
Lymphoma group ESHAP and R-ESHAP INDICATION Chemosensitive relapsed / refractory Hodgkin and non-Hodgkin lymphoma. Omit rituximab if CD20-negative. TREATMENT INTENT Disease Modification. PRE-ASSESSMENT 1. Ensure histology is confirmed prior to administration of chemotherapy and document in notes. 2. Record stage of disease - contrast enhanced CT scan (neck, chest, abdomen and pelvis), and/or PET-CT scan, presence or absence of B symptoms, clinical extent of disease. Bone marrow trephine if clinically indicated in Non Hodgkins lymphoma. 3. Blood tests - FBC, ESR, U&Es, LDH, urate, calcium, magnesium, creatinine, LFTs, glucose, hepatitis B core antibody and hepatitis B surface Ag, hepatitis C antibody 4. Send a "group and save" sample to transfusion and inform patient and transfusion laboratory that they will require irradiated blood products for 7 days before harvest. See ‘Guidelines for the use of blood components in adult haematology' for details. Ensure irradiation card is attached to the patient's notes and copy given to the patient. 5. Urine pregnancy test • before cycle 1 of each new chemotherapy course for women of child- bearing age unless they are post-menopausal, have been sterilised or undergone a hysterectomy. 6. ECG +/- Echo - if clinically indicated. 7. Record performance status, height and weight. 8. Consent - ensure patient has received adequate verbal and written information regarding their disease, treatment and potential side effects. Document in medical notes all information that has been given. Obtain written consent prior to treatment. 9. Fertility - it is very important the patient understands the potential risk of reduced fertility. All patients should be offered fertility advice by referring to the Oxford Fertility Unit).