Uterine Tachysystole, Hypertonus and Hyperstimulation: an Urgent Need to Get the Definitions Right to Avoid Intrapartum Hypoxic- Ischaemic Brain Injury
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Placental Abruption
Placental Abruption Definition: Placental separation, either partial or complete prior to the birth of the fetus Incidence 0.5 – 1% (4). Risk factors include hypertension, smoking, preterm premature rupture of membranes, cocaine abuse, uterine myomas, and previous abruption (5). Diagnosis: Symptoms (may present with any or all of these) o Vaginal bleeding (usually dark and non-clotting). o Abdominal pain and/or back pain varying from intermittent to severe. o Uterine contractions are usually present and may vary from low amplitude/high frequency to hypertonus. o Fetal distress or fetal death. Ultrasound o Adherent retroplacental clot OR may just appear to be a thick placenta o Resolving hematomas become hypoechoic within one week and sonolucent within 2 weeks May be a diagnosis of exclusion if vaginal bleeding and no other identified etiology Consider in differential with uterine irritability on toco and cat II-III tracing, as small proportion present without bleeding Classification: Grade I: Slight vaginal bleeding and some uterine irritability are usually present. Maternal blood pressure, and fibrinogen levels are unaffected. FHR remains normal. Grade II: Mild to moderate vaginal bleeding seen; tetanic contractions may be present. Blood pressure usually normal, but tachycardia may be present. May be postural hypotension. Decreased fibrinogen; with levels below 250 mg percent; may be evidence of fetal distress. Reviewed 01/16/2020 1 Updated 01/16/2020 Grade III: Bleeding is moderate to severe, but may be concealed. Uterus tetanic and painful. Maternal hypotension usually present. Fetal death has occurred. Fibrinogen levels are less then 150 mg percent with thrombocytopenia and coagulation abnormalities. -

Uterine Rupture After Misoprostol Use for Termination of Pregnancy in Second Trimester with Previous Caesarean Section: a Case Report Marjan Ghaemi*
Case Report iMedPub Journals Critical Care Obstetrics and Gynecology 2018 http://www.imedpub.com/ Vol.4 No.3:14 ISSN 2471-9803 DOI: 10.21767/2471-9803.1000167 Uterine Rupture after Misoprostol Use for Termination of Pregnancy in Second Trimester with Previous Caesarean Section: A Case Report Marjan Ghaemi* Yas Hospital, Tehran University of Medical Sciences, Tehran, Iran *Corresponding author: Marjan Ghaemi, Yas Hospital, Tehran University of Medical Sciences, Tehran, Iran, Tel: 0098-912-1967735; E-mail: [email protected] Received date: September 25, 2018; Accepted date: October 16, 2018; Published date: October 22, 2018 Copyright: © 2018 Ghaemi M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Citation: Ghaemi M (2018) Uterine Rupture after Misoprostol Use for Termination of Pregnancy in Second Trimester with Previous Caesarean Section: A Case Report. Crit Care Obst Gyne Vol.4 No.3:14. cesarean section, hospitalized for severe oligohydramnios with unknown etiology and no history of fluid leakage. In her Abstract previous surgical history, she mentioned laparoscopic cholecystectomy 10 years ago. Considering her medical history Modalities for termination of pregnancy may result in some and normal kidney and bladder in fetal ultrasound, we did not adverse effects especially uterine rupture in women with have proved data for her severe oligohydramnios. Amnio- the previous cesarean section. Here we report uterine infusion was performed to prevent foetal cord compression and rupture in the 23rd week of pregnancy after Misoprostol uses for abortion induction in second pregnancy with the to assess foetal structures. -

Management of Prolonged Decelerations ▲
OBG_1106_Dildy.finalREV 10/24/06 10:05 AM Page 30 OBGMANAGEMENT Gary A. Dildy III, MD OBSTETRIC EMERGENCIES Clinical Professor, Department of Obstetrics and Gynecology, Management of Louisiana State University Health Sciences Center New Orleans prolonged decelerations Director of Site Analysis HCA Perinatal Quality Assurance Some are benign, some are pathologic but reversible, Nashville, Tenn and others are the most feared complications in obstetrics Staff Perinatologist Maternal-Fetal Medicine St. Mark’s Hospital prolonged deceleration may signal ed prolonged decelerations is based on bed- Salt Lake City, Utah danger—or reflect a perfectly nor- side clinical judgment, which inevitably will A mal fetal response to maternal sometimes be imperfect given the unpre- pelvic examination.® BecauseDowden of the Healthwide dictability Media of these decelerations.” range of possibilities, this fetal heart rate pattern justifies close attention. For exam- “Fetal bradycardia” and “prolonged ple,Copyright repetitive Forprolonged personal decelerations use may onlydeceleration” are distinct entities indicate cord compression from oligohy- In general parlance, we often use the terms dramnios. Even more troubling, a pro- “fetal bradycardia” and “prolonged decel- longed deceleration may occur for the first eration” loosely. In practice, we must dif- IN THIS ARTICLE time during the evolution of a profound ferentiate these entities because underlying catastrophe, such as amniotic fluid pathophysiologic mechanisms and clinical 3 FHR patterns: embolism or uterine rupture during vagi- management may differ substantially. What would nal birth after cesarean delivery (VBAC). The problem: Since the introduction In some circumstances, a prolonged decel- of electronic fetal monitoring (EFM) in you do? eration may be the terminus of a progres- the 1960s, numerous descriptions of FHR ❙ Complete heart sion of nonreassuring fetal heart rate patterns have been published, each slight- block (FHR) changes, and becomes the immedi- ly different from the others. -
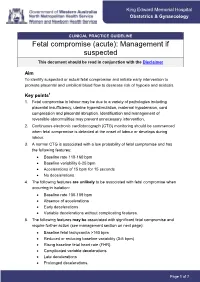
Fetal Compromise (Acute): Management If Suspected This Document Should Be Read in Conjunction with the Disclaimer
King Edward Memorial Hospital King Edward Memorial Hospital Obstetrics & Gynaecology Obstetrics & Gynaecology CLINICAL PRACTICE GUIDELINE Fetal compromise (acute): Management if suspected This document should be read in conjunction with the Disclaimer Aim To identify suspected or actual fetal compromise and initiate early intervention to promote placental and umbilical blood flow to decrease risk of hypoxia and acidosis. Key points1 1. Fetal compromise in labour may be due to a variety of pathologies including placental insufficiency, uterine hyperstimulation, maternal hypotension, cord compression and placental abruption. Identification and management of reversible abnormalities may prevent unnecessary intervention. 2. Continuous electronic cardiotocograph (CTG) monitoring should be commenced when fetal compromise is detected at the onset of labour or develops during labour. 3. A normal CTG is associated with a low probability of fetal compromise and has the following features: Baseline rate 110-160 bpm Baseline variability 6-25 bpm Accelerations of 15 bpm for 15 seconds No decelerations. 4. The following features are unlikely to be associated with fetal compromise when occurring in isolation: Baseline rate 100-109 bpm Absence of accelerations Early decelerations Variable decelerations without complicating features. 5. The following features may be associated with significant fetal compromise and require further action (see management section on next page): Baseline fetal tachycardia >160 bpm Reduced or reducing baseline variability -

Intra-Vaginal Prostaglandin E2 Versus Double-Balloon Catheter for Labor Induction in Term Oligohydramnios
Journal of Perinatology (2015) 35, 95–98 © 2015 Nature America, Inc. All rights reserved 0743-8346/15 www.nature.com/jp ORIGINAL ARTICLE Intra-vaginal prostaglandin E2 versus double-balloon catheter for labor induction in term oligohydramnios G Shechter-Maor1, G Haran1, D Sadeh-Mestechkin1, Y Ganor-Paz1, MD Fejgin1,2 and T Biron-Shental1,2 OBJECTIVE: Compare mechanical and pharmacological ripening for patients with oligohydramnios at term. STUDY DESIGN: Fifty-two patients with oligohydramnios ⩽ 5 cm and Bishop score ⩽ 6 were randomized for labor induction with a vaginal insert containing 10 mg timed-release dinoprostone (PGE2) or double-balloon catheter. The primary outcome was time from induction to active labor. Time to labor, neonatal outcomes and maternal satisfaction were also compared. RESULT: Baseline characteristics were similar. Time from induction to active labor (13 with PGE2 vs 19.5 h with double-balloon catheter; P = 0.243) was comparable, with no differences in cesarean rates (15.4 vs 7.7%; P = 0.668) or neonatal outcomes. The PGE2 group had higher incidence of early device removal (76.9 vs 26.9%; P = 0.0001), mostly because of active labor or non-reassuring fetal heart rate. Fewer PGE2 patients required oxytocin augmentation for labor induction (53.8 vs 84.6% P = 0.034). Time to delivery was significantly shorter with PGE2 (16 vs 20.5 h; P = 0. 045) CONCLUSION: Intravaginal PGE2 and double-balloon catheter are comparable methods for cervical ripening in term pregnancies with oligohydramnios. Journal of Perinatology (2015) 35, 95–98; doi:10.1038/jp.2014.173; published online 2 October 2014 INTRODUCTION better mimic the natural course of labor and might have an Ultrasound estimation of amniotic fluid volume is an important advantage in cervical ripening. -

INTRODUCTION Effect of Different Dosages of Intravaginal Misoprostol
Original Article Gynecology and Obstetrics Medical Journal of Islamic World Academy of Sciences Effect of Different Dosages of Intravaginal Misoprostol for Second Trimester Pregnancy Termination Maysoon Sharief1, Enaas S. Al-Khayat1 1Department of Gynecology and Obstetrics, College of Medicine, University of Basrah, Basrah, Iraq. ABSTRACT Miscarriage is a common complication of early pregnancy; however; curettage and dilation are considered standard methods taking care of early pregnancy failure. Misoprostol has been used as an alternative agent for termination of early pregnancy. Therefore, this study was aimed to compare the efficacy and side effects of two different intravaginal misoprostol trials for the second trimester pregnancy termination of missed miscarriage between 14 and 23 weeks. A clinical trial was carried out in Basrah Maternity & Children Hospital during the period from October 2011 to November 2012. A total of 100 women experienced missed miscarriages at 14-23 weeks of gestation were admitted for medical termination of pregnancy. Patients were divided into the following two groups: Group 1: 50 patients received 400 µg of intravaginal misoprostol/8 hours. Group 2: 50 patients received 800 µg of intravaginal misoprostol/8 hours. The patients were followed up for 24 hours. The primary outcome measure was induction-miscarriage interval; the secondary outcomes were the rate of successful miscarriage and complete miscarriage; the incidence of side effects was compared in both groups. The rates of successful termination of pregnancy in both groups 1 and 2 were 86% and 90%, respectively. The success rates of the drug in group 1 were 0%, 12%, 36%, 34%, 10%, and 4% after first, second, third, fourth, fifth, and sixth doses, respectively; whereas, the success rates in group 2 were 24%, 34%, 24%, 12%, 4%, and 0% after first, second, third, fourth, fifth, and sixth doses, respectively. -

Confidential: for Review Only Continued Versus Discontinued Oxytocin Stimulation in the Active Phase of Labour (CONDISOX)- a Double-Blind Randomised Controlled Trial
BMJ Confidential: For Review Only Continued versus discontinued oxytocin stimulation in the active phase of labour (CONDISOX)- A double-blind randomised controlled trial Journal: BMJ Manuscript ID BMJ-2020-063027 Article Type: Research BMJ Journal: BMJ Date Submitted by the 09-Nov-2020 Author: Complete List of Authors: Boie, Sidsel; Randers Regional Hospital, Obstetrics and Gynaecology Glavind, Julie; Aarhus University Hospital, Obstetrics and Gynaecology Uldbjerg, Niels; Aarhus University Hospital, Obstetrics and Gynecology Steer, Philip; Imperial College London, Academic Department of Obstetrics and Gynaecology Bothazi, Attila; Aalborg University Hospital, Obstetrics and Gynaecology Sundtoft, Iben ; Hospitalsenheden Vest, Obstetrics and Gynaecology Bakker, Jannet; Amsterdam UMC Location AMC, Obstetrics and Gynaecology Van der Post, Joris; Amsterdam UMC Location AMC, Obstetrics and Gynaecology Renault, Kristina; Rigshospitalet, Obstetrics and Gynaecology Huusom, Lene; Hvidovre Hospital, Obstetrics and Gynaecology Hvidman, Lone; Aarhus University Hospital, Obstetrics and Gynaecology Rask, Maja; Odense University Hospital, Obstetrics and Gynaecology Khalil, Mohammed; Sygehus Lillebalt Kolding Sygehus, Obstetrics and Gynaecology Møller, Nini; Nordsjaellands Hospital, Obstetrics and Gynaecology Greve, Tine; Hvidovre Hospital, Obstetrics and Gynaecology Bor, Pinar; Randers Regional Hospital, Obstetrics and Gynaecology induction of labour, oxytocin, discontinuation, Caesarean section, active Keywords: phase of labour, uterine tachysystole -

Concurrent Intraoperative Uterine Rupture and Placenta Accreta. Do
Concurrent intraoperative uterine rupture and placenta accreta Romanian Journal of Anaesthesia and Intensive Care 2018 Vol 25 No 1, 83-85 CASE REPORT DOI: http://dx.doi.org/10.21454/rjaic.7518.251.acc Concurrent intraoperative uterine rupture and placenta accreta. Do preoperative chronic hypertension, preterm premature rupture of membranes, chorioamnionitis, and placental abruption provide warning to this rare occurrence? M. Anthony Cometa, Scott M. Wasilko, Adam L. Wendling Department of Anesthesiology, Division of Obstetric Anesthesiology, University of Florida College of Medicine, Gainesville, FL, USA Abstract Uterine and placental pathology can be a major cause of morbidity and mortality in the parturient and infant. When presenting alone, placental abruption, uterine rupture, or placenta accreta can result in significant peripartum hemorrhage, requiring aggressive surgical and anesthetic management; however, the presence of multiple concurrent uterine and placental pathologies can result in significant morbidity and mortality. We present the anesthetic management of a parturient who underwent an urgent cesarean delivery for non- reassuring fetal tracing in the setting of chronic hypertension, preterm premature rupture of membranes, and chorioamnionitis who was subsequently found to have placental abruption, uterine rupture, and placenta accreta. Keywords: preterm premature rupture of membranes (PPROM), chorioamnionitis, placental abruption, uterine rupture, placenta accrete, cesarean-hysterectomy Received: 14 March 2018 / Accepted: 30 March 2018 Rom J Anaesth Intensive Care 2018; 25: 83-85 operative bleeding that requires aggressive fluid and blood product management and resuscitation [5]. At present, the literature does not reference the Introduction presentation and anesthetic management of these aforementioned conditions being concurrently present Various placental and uterine pathologies can result in one parturient. -

Terms/Definitions
9th Annual AABC Birth Institute 10/1/2015 HEAD COMPRESSION: PLAINTIFF’S NEW THEORY TO EXPLAIN CEREBRAL PALSY 9th ANNUAL AABC BIRTH INSTITUTE OCTOBER 1-4, 2015, SCOTTSDALE, AZ OCTOBER 2, 2015 Julia K. McNelis, R.N., J.D. Kitch Drutchas Wagner Valitutti & Sherbrook Mt. Clemens, Michigan (Detroit, Marquette, Lansing, Chicago, Toledo) Terms/Definitions • Freemans, 3rd Ed. 2003 • NICHD 2008 • ACOG 2009 • Williams, 23nd Ed. 2010 • Freeman’s, 4th Ed. 2012 1 9th Annual AABC Birth Institute 10/1/2015 Freeman’s 3rd Ed (2003) • Primary function of ctx is expulsion of uterine contents • Manual palpation has been traditional method of monitoring ctx • During labor strength varies 30mm Hg average early labor to 50 mm Hg later first stage • 50mm Hg to 80 mm Hg second stage • Once labor starts ctx become more frequent and stronger Freeman’s 3rd (2003) Fig 5.8 2 9th Annual AABC Birth Institute 10/1/2015 NICHD (2008) • Normal-5 or less ctx in 10 minutes, averaged over 30 minutes • Tachysystole-> 5 ctx in 10 minutes, averaged over 30 minutes • “Hyperstimulation” and “hypercontractility” are not defined and should be abandoned ACOG # 107 (2009) • Adopts NICHD definitions • Tachysystole should always be qualified as to the presence or absence of associated FHR decelerations • The term tachysystole applies to both spontaneous and stimulated labor 3 9th Annual AABC Birth Institute 10/1/2015 Williams 23 Ed. 2010 • Ctx in normal labor-forces are greatest and last longest at the fundus and diminish towards the cervix • The Montevideo group ascertained that the lowest limit of ctx pressure required to dilate the cervix is 15 mm Hg Williams 23 Ed. -

Misoprostol Tablets
Cytotec® misoprostol tablets WARNINGS CYTOTEC (MISOPROSTOL) ADMINISTRATION TO WOMEN WHO ARE PREGNANT CAN CAUSE BIRTH DEFECTS, ABORTION, PREMATURE BIRTH OR UTERINE RUPTURE. UTERINE RUPTURE HAS BEEN REPORTED WHEN CYTOTEC WAS ADMINISTERED IN PREGNANT WOMEN TO INDUCE LABOR OR TO INDUCE ABORTION. THE RISK OF UTERINE RUPTURE INCREASES WITH ADVANCING GESTATIONAL AGES AND WITH PRIOR UTERINE SURGERY, INCLUDING CESAREAN DELIVERY (see also PRECAUTIONS and LABOR AND DELIVERY). CYTOTEC SHOULD NOT BE TAKEN BY PREGNANT WOMEN TO REDUCE THE RISK OF ULCERS INDUCED BY NONSTEROIDAL ANTI-INFLAMMATORY DRUGS (NSAIDs) (see CONTRAINDICATIONS, WARNINGS, and PRECAUTIONS). PATIENTS MUST BE ADVISED OF THE ABORTIFACIENT PROPERTY AND WARNED NOT TO GIVE THE DRUG TO OTHERS. Cytotec should not be used for reducing the risk of NSAID-induced ulcers in women of childbearing potential unless the patient is at high risk of complications from gastric ulcers associated with use of the NSAID, or is at high risk of developing gastric ulceration. In such patients, Cytotec may be prescribed if the patient has had a negative serum pregnancy test within 2 weeks prior to beginning therapy. is capable of complying with effective contraceptive measures. has received both oral and written warnings of the hazards of misoprostol, the risk of possible contraception failure, and the danger to other women of childbearing potential should the drug be taken by mistake. will begin Cytotec only on the second or third day of the next normal menstrual period. DESCRIPTION Cytotec oral tablets contain either 100 mcg or 200 mcg of misoprostol, a synthetic prostaglandin E1 analog. 1 Reference ID: 4228046 Misoprostol contains approximately equal amounts of the two diastereomers presented below with their enantiomers indicated by (±): Misoprostol is a water-soluble, viscous liquid. -

20180523 Vlemminx
Real-time electrohysterography Citation for published version (APA): Vlemminx, M. W. C. (2018). Real-time electrohysterography: a novel technology used on the labour ward. Technische Universiteit Eindhoven. Document status and date: Published: 23/05/2018 Document Version: Publisher’s PDF, also known as Version of Record (includes final page, issue and volume numbers) Please check the document version of this publication: • A submitted manuscript is the version of the article upon submission and before peer-review. There can be important differences between the submitted version and the official published version of record. People interested in the research are advised to contact the author for the final version of the publication, or visit the DOI to the publisher's website. • The final author version and the galley proof are versions of the publication after peer review. • The final published version features the final layout of the paper including the volume, issue and page numbers. Link to publication General rights Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. • Users may download and print one copy of any publication from the public portal for the purpose of private study or research. • You may not further distribute the material or use it for any profit-making activity or commercial gain • You may freely distribute the URL identifying the publication in the public portal. If the publication is distributed under the terms of Article 25fa of the Dutch Copyright Act, indicated by the “Taverne” license above, please follow below link for the End User Agreement: www.tue.nl/taverne Take down policy If you believe that this document breaches copyright please contact us at: [email protected] providing details and we will investigate your claim. -

PPH 2Nd Edn #23.Vp
43 Standard Medical Therapy for Postpartum Hemorrhage J. Unterscheider, F. Breathnach and M. Geary INTRODUCTION firm contraction of the organ. If severe haemorrhage has already set in, it is highly recommended that the drug should Failure of the uterus to contract and retract following be given by the intravenous route. For this purpose one-third childbirth has for centuries been recognized as the of the standard size ampoule may be injected or, for those most striking cause of postpartum hemorrhage (PPH) who wish accurate dosage, a special ampoule containing and complicates up to 10% of pregnancies globally. In 0.125 mg is manufactured. An effect may be looked for in less the developing world, PPH is responsible for one than one minute.’ maternal death every 7 minutes1. Another uterotonic agent, oxytocin, the hypothalamic In the 19th century, uterine atony was treated by polypeptide hormone released by the posterior pitu- intrauterine placement of various agents with the aim itary, was discovered in 1909 by Sir Henry Dale8 and of achieving a tamponade effect. ‘A lemon imperfectly synthesized in 1954 by du Vigneaud9. The develop- quartered’ or ‘a large bull’s bladder distended with ment of oxytocin constituted the first synthesis of water’ were employed for this purpose, with apparent a polypeptide hormone and gained du Vigneaud a success. Douching with vinegar or iron perchloride Nobel Prize for his work. was also reported2,3. Historically, the first uterotonic The third group of uterotonics comprises the ever- drugs were ergot alkaloids,