2019 Final Rx Tracker 3.12.2021 Update.Xlsx
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Listed the Senate and House Education Committees Below Because That’S the Two We Most Often Deal With
Here is a link to the House roster where you will find contact information for House members: http://www.wvlegislature.gov/house/roster.cfm Here is a link to the Senate roster where you will find contact information for Senate members: https://www.wvlegislature.gov/senate1/roster.cfm Please make sure you are familiar with your local legislators as well as those in leadership positions. The new directory is available on the legislative site. I listed the Senate and House Education Committees below because that’s the two we most often deal with. WEST VIRGINIA STATE SENATE LEADERSHIP SENATE PRESIDENT— CRAIG P. BLAIR PREIDENT PRO TEMPORE – DONNA BOLEY MAJORITY LEADER – TOM TAKUBO MAJORITY WHIP – RYAN W. WELD MINORITY LEADER – STEPHEN BALDWIN MINORITY WHIP – MICHAEL WOELFEL SENATE EDUCATION COMMITTEE Patricia Rucker - Chair Robert Karnes - Vice Chair Azinger, Beach, Boley, Clements, Grady, Plymale, Roberts, Romano, Stollings, Tarr, Trump, Unger SENATE FINANCE Eric Tarr - Chair Dave Sypolt - Vice Chair Baldwin, Boley, Clements, Hamilton, Ihlenfeld, Jeffries, Maroney, Martin, Nelson, Plymale, Roberts, Stollings, Swope, Takubo, Unger SENATE DISTRICT - 01 William Ihlenfeld (D - Ohio) Ryan Weld (R - Brooke) SENATE DISTRICT - 02 Michael Maroney (R - Marshall) Charles Clements (R - Wetzel) SENATE DISTRICT - 03 Donna Boley (R - Pleasants) Michael Azinger (R - Wood) SENATE DISTRICT - 04 Amy Grady (R - Mason) Eric Tarr (R - Putnam) SENATE DISTRICT - 05 Robert Plymale (D - Wayne) Michael Woelfel (D - Cabell) SENATE DISTRICT - 06 Chandler Swope (R - Mercer) -

Contact Information
AFT West Virginia 82nd West Virginia Legislature Education Committee Members The Senate and House Education Committees are the starting points for all education legislation. Call these legislators to voice your concerns on proposed education bills. Senate Education Committee Senate Education Senate Education Chair Senate Education Senate Judiciary Chair Senator Dave Sypolt – District 14(R) Senator Charles S. Trump IV – District 15(R) Capitol: (304) 357-7914 Capitol: (304) 357-7980 [email protected] [email protected] Home County: Preston Home County: Morgan District: Barbour, Grant, Mineral, Preston District: Berkeley, Hampshire, Mineral, Morgan Taylor, Tucker Senate Education Education Vice-Chair Senate Education Senator Donna J. Boley – District 3(R) Senator Robert D. Beach – District 13(D) Capitol: (304) 357-7905 Capitol: (304) 357-7919 [email protected] [email protected] Home County: Pleasants Home County: Monongalia District: Pleasants, Roane, Wood, Wirt District: Marion, Monongalia Senate Education Senate Majority Leader Senate Education Senator Mitch Carmichael – District 4(R) Senator William R. Laird IV – District 10(D) Capitol: (304) 357-7855 Capitol: (304) 357-7849 [email protected] [email protected] Home County: Jackson Home County: Fayette District: Jackson, Mason, Putnam, Roane District: Fayette, Greenbrier, Monroe, Summers Senate Education Senate Finance Chair Senate Education Senator Mike Hall – District 4(R) Senator Robert H. Plymale – District 5(D) Capitol: (304) -

05 Overview of MEREDA's Legislative Agenda
2021 Public Policy Update Presented by: Andrea Cianchette Maker, Pierce Atwood LLP Elizabeth M. Frazier, Pierce Atwood LLP Meeting the 130th Legislature. from afar Senate House President Troy Jackson Speaker Ryan Fecteau 21 Democrats, 13 Republicans 80 Democrats, 66 Republicans, 4 Independents, 1 empty seat 1 Libertarian, 3 nonvoting Tribal Representatives • Majority Leader: Nate Libby • • Assistant Majority Leader: Eloise Vitelli Majority Leader: Michelle Dunphy • • Minority Leader: Jeff Timberlake Assistant Majority Leader: Rachel Talbot Ross • • Assistant Minority Leader: Matt Pouliot Minority Leader: Kathleen Dillingham • Assistant Minority Leader: Joel Stetkis Participating During a Pandemic ❖ State House remains closed ❖ Committee hearings, work sessions to be broadcast on the Maine Legislature’s YouTube Channel ❖ Testimony, work session participation via Zoom ❖ House, Senate meeting schedule and location uncertain Economic Recovery, Budget Gap Economic Recovery Committee Report • INNOVATION & Better than ENTREPRENEURSHIP anticipated Cost cutting, hiring freeze • TALENT DEVELOPMENT & revenues TALENT ATTRACTION • BROADBAND / INTERNET ACCESS CARES Act, PPP • EARLY CARE AND EDUCATION SUPPORTS $250 million shortfall • STRUCTURAL remaining in FY ‘21 INEQUITIES • RECOMMENDED $400 million budget shortfall INVESTMENTS for FY ’22/23 Biennium Climate Council Recommendations Strategies to Reduce Greenhouse Gas Emissions A: Embrace the Future of Transportation in Maine B: Modernize Maine’s Buildings C: Reduce Carbon Emissions in Energy and Industrial Sectors D: Grow Maine’s Clean-Energy Economy and Protect our Natural Resource Industries E: Protect Maine’s Environment F: Build Healthy and Resilient Communities G: Invest in Climate-Ready Infrastructure H: Engage with Maine People and Communities By 2024, develop a long-term plan to phase-in modern, energy efficient building codes to reach net zero carbon emissions for new construction in Maine by 2035. -
Draft Report of the Massachusetts Autonomous Vehicles Working Group
REPORT OF THE MASSACHUSETTS AUTONOMOUS VEHICLES WORKING GROUP DRAFT FOR DISCUSSION PURPOSES ONLY – ACTIVE POLICY DEVELOPMENT v4.0 Submitted Pursuant to Executive Order 572 September 12, 2018 DRAFT FOR DISCUSSION PURPOSES ONLY – ACTIVE POLICY DEVELOPMENT Table of Contents 1 Autonomous Vehicles Working Group Members ................................................................. 3 2 Introduction ...................................................................................................................................... 4 3 Connected and Autonomous Vehicles – Technology Overview ...................................... 7 3.1 C/AV Industry in Massachusetts .......................................................................................................... 11 4 Governance ..................................................................................................................................... 14 5 Policy Considerations ................................................................................................................. 18 5.1 Establishing a C/AV Committee ........................................................................................................... 20 5.2 Engaging First Responders and Law Enforcement ...................................................................... 22 5.3 Moving From Executive Order to Regulation ................................................................................. 23 5.4 Establishing Legislation ......................................................................................................................... -

Nicholas Saggese Bruce Tarr
Awards Banquet ~ October 27th, 2018 Nicholas Saggese Detective (Ret.) Boston Police Department 2018 Recipient Saint Michael e Archangel Award Bruce Tarr State Senator (First Essex and Middlesex District) 2018 Recipient Saint Michael e Archangel Award 194 South Main Street, Middleton, MA 01949 978-777-2196 Proud Supporter of Masschusetts Association of Italian American Police Officers Massachusetts Association of Italian American Police Officers, Inc. SINCE 1968 Association President’s Message Welcome to the 50th Annual Awards Banquet of the National /Massachusetts Italian American Police Officer’s Association Dear Friends, Since 1968 the National Association of Italian American Police Officers has been promoting the role of law enforcement in our communities and honoring our Italian Heritage. This is the 50th year as an Association and we continue to provide recognition of the courageous actions of members of law enforcement in their efforts to preserve the peace and maintain order. The Association was started by a group of Boston Police Department Officers that sought to organize for upward mobility in the department and in celebration of their Italian Heritage. Over the years the organization has expanded throughout Massachusetts and around the country. We have members in Florida, California, Texas, and Illinois to name a few. Law enforcement careers are one of the few where each day you do not know what violent or potentially life threatening event you may be confronted with. So far in 2018, 110 officers have been killed in the line of duty. Despite some highly publicized incidents of rouge officers dishonoring the badge the vast majority of officers work hard every day to protect the public and control crime. -

380 Bills / Regs.)
Available Bills / Regulations (380 bills / regs.) Bill/Reg. # Categories Summary Status Alabama Mortgage Lending: Eminent domain, condemnation actions, land acquisitions of rights-of-way, waiver valuations authorized under certain 05/22/2019 - HB 98 Appraisals conditions, Secs. 18-1A-3, 18-1A-22 am'd. Signed by 2019 Real Estate: Governor; Enacted Ellis Condemnation, General History Alabama Mortgage Lending: Mobile Co., transfer of duties from judge of probate to revenue commissioner, legislative intent clarified, Act 2015-265, 05/13/2019 - HB 214 Foreclosure 2015 Reg. Sess., am'd. Signed by 2019 Proceedings/Admin Governor; Enacted Pringle History Alabama Electronic Commerce: E- Business entities, revising the Alabama Business Corporation Law, to reflect national standards set by the Model 05/01/2019 - HB 250 Sign/Disclosure Business Corporation Act, Secs. 10A-2A-1.01 to 10A-2A-17.06, inclusive added; Secs. 10A-1-1.02, 10A-1-1.03, 10A- Signed by 2019 Mortgage Lending: 1-1.08, 10A-1-1.12, 10A-1-3.05, 10A-1-3.06, 10A-1-3.32, 10A-1-3.42, ... Governor; Enacted Poole Appraisals History Securities & Investments: Trusts/Funds/Bonds/Options Alabama Mortgage Lending: Real Estate Appraisers Board, evaluations of property for financial institutions authorized by federal financial 05/29/2019 - HB 304 Appraisal Management institutions regulatory agencies, excluded from regulation by the board, investigators employed by board authorized to Signed by 2019 Companies, Appraisals be licensees, Secs. 34-27A-2, 34-27A-3, 34-27A-5, 34-27A-23 am'd. Governor; Enacted Rep. Merika History Coleman-Evans (D-AL) Alabama Mortgage Lending: Geneva Co., office of judge of probate, special recording fee, authorized, distrib. -
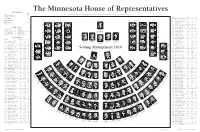
2020 Minnesota House of Representatives Seating Chart
The Minnesota House of Representatives House Leadership Seat Melissa Hortman .................................... 139 Minnesota House of Representatives Public Information Services, 651-296-2146 or 800-657-3550 Speaker of the House District Room* 296- Seat Ryan Winkler.......................................... 102 44A Klevorn, Ginny (DFL) .........581 ....... 5511 ..... 104 Majority Leader 37A Koegel, Erin (DFL) .............375 ....... 5369 ..... 126 48B Kotyza-Witthuhn, Carlie (DFL) ....567 ............7449 ...........81 Golden Valley—45B Bloomington—49B Shelly Christensen Kurt Daudt ............................................... 23 Mike Freiberg Stillwater—39B 58A Koznick, Jon (R) .................229 ....... 6926 ......... 5 Seat 129 Steve Elkins Seat 135 Minority Leader Seat 124 9B Kresha, Ron (R) ...................207 ....... 4247 ....... 12 Seat 6 41B Kunesh-Podein, Mary (DFL)... 445 ..........4331 ......... 97 Seat 1 Seat 11 Mary Franson Luverne—22A Alexandria—8B Joe Schomacker 5B Layman, Sandy (R) ..............233 ....... 4936 ....... 38 Shane Mekeland House Officers Clear Lake—15B Maplewood—53A Rosemount—57B St. Peter—19A Jeff Brand 59A Lee, Fue (DFL) ....................485 ....... 4262 ..... 125 Seat 128 John Huot Tou Xiong Tou Seat 134 Patrick D. Murphy .......... 142 Marilee Davis .................. 141 Seat 123 Seat 139 Chief Clerk Desk Clerk Melissa Hortman 66B Lesch, John (DFL) ...............563 ....... 4224 ..... 116 Timothy M. Johnson ....... 143 David G. Surdez ............. 140 Brooklyn Park—36B Seat 7 Seat 2 26A Liebling, Tina (DFL) ...........477 ....... 0573 ..... 114 Speaker of the House Seat 12 Peggy Scott Ron Kresha 1st Asst. Chief Clerk Legislative Clerk John Poston Andover—35B Little Falls—9B Brooklyn Center—40B Lake Shore—9A International Falls—3A 4A Lien, Ben (DFL) ..................415 ....... 5515 ....... 72 Gail C. Romanowski ....... 144 Bob Meyerson ................... 69 South St. Paul—52A Samantha Vang Seat 127 2nd Asst. -

Legislative Profiles Spring 2019 |
Legislative Profiles Spring 2019 | Announcement Inside This Issue This portfolio contains the profiles of all legislators that belong to PG. 2: Forward key committees within the Commonwealth of Massachusetts. PG. 4: House Bill – H.2366 Each key committee will play a role in the review and approval of the retirement bills that have been filed. PG. 8: Senate Bill – SD.1962 PG. 11: Joint Committee on Public Service – Profiles PG. 29: House Ways & Means – Profiles This portfolio is for the members of MCSA to use to determine PG. 63: House Committee on Third Reading – Profiles which members reside within their regions so contact can be made with each legislator for support of both retirement bills. PG. 67: Senate Ways & Means – Profiles PG. 86: Senate Committee on Third Reading – Profiles PG. 92: Talking Point Tips PG. 93: Legislative Members by MCSA Regions FORWARD Many of us do not have experience with advocating for legislation or meeting with our legislative representatives. This booklet was created with each you in mind to assist in determining which members reside within your region or represent your town and city. We request you contact your respective legislators for support of both retirement bills. If you are familiar with the legislative process and your representatives this may seem rudimentary. The Massachusetts Legislature is comprised of 200 members elected by the people of the Commonwealth. The Senate is comprised of 40 members, with each representing a district of approximately 159,000 people. The House of Representatives is comprised of 160 members, with each legislator representing districts consisting of approximately 40,000 people. -
2020 Annual Report
Essex County Sheriff's Department 2020 Annual Report SHERIFF KEVIN F. COPPINGER Table ooff Contents Sheriff’s Message i Executive Team Photos 1 Department Policy, Mission Statement & Correctional Officer’s Core Values 2 Sheriff Kevin F. Coppinger 3 By the Numbers 4 Department Overview 5 Department’s Three Correctional Facilities 7 Middleton Facility 7 Classification _ 9 Programs & Treatment 12 Chaplaincy 15 Specialized Re-Entry Services 16 Medication Assisted Treatment (MAT) 16 Clean and Sober Existence (CASE) 19 Correctional Alternatives for Re-Entry (CARE) 22 Essex Medication Assisted Treatment Program (EMAT) 22 Essex County Mental Health Diversion Program 23 Correctional Opportunity for Personal Enrichment (COPE) 24 Essex County Pre-Release and Re-Entry Center 25 Programs & Treatment 26 Career Training 28 Education 29 The Farm 30 Profiles in Perseverance 31 Women In Transition Facility 32 Community Service & Work Release 34 Offices of Community Corrections 36 One-Year Recidivism Rates 40 Daily Workings of ECSD 41 Middleton Intake 41 Criminal Records 41 Transportation 42 Inmate Property 43 Video Conferencing 43 Central Control 45 Outer Perimeter Security 46 Female Holding Area 47 Visits 47 Tool Control 47 Key Control 48 Inmate Mail 48 DNA Collection 48 Armory 49 Incident Command Structure 50 Housing Units, Inspections, & Audits 51 Environmental Health & Safety/Fire Safety 51 Housing Units 52 Audits 54 Office of Professional Standards____________ 56 Centralized Scheduling 58 Human Resources 59 Training & Staff Development 67 Internal -

Current Office Holders
Federal Name Party Office Term Next Election Joe Biden Democrat U.S President 4 Years 2024 Kamala Harris Democrat U.S. Vice President 4 Years 2024 Joe Manchin Democratic U.S. Senate 6 Years 2024 Shelley Moore Capito Republican U.S. Senate 6 Years 2026 David McKinley Republican U.S House, District 1 2 Years 2022 Alexander Mooney Republican U.S. House, District 2 2 Years 2022 Carol Miller Republican U.S. House, District 3 2 Years 2022 State Name Party Office Term Next Election Jim Justice Republican Governor 4 Years 2024 Mac Warner Republican West Virginia Secretary of State 4 Years 2024 John "JB" McCuskey Republican West Virginia State Auditor 4 Years 2024 Riley Moore Republican West Virginia State Treasurer 4 Years 2024 Patrick Morrisey Republican Attorney General of West Virginia 4 Years 2024 Kent Leonhardt Republican West Virginia Commissioner of Agriculture 4 Years 2024 West Virginia State Senate Name Party District Next election Ryan W. Weld Republican 1 2024 William Ihlenfeld Democrat 1 2022 Mike Maroney Republican 2 2024 Charles Clements Republican 2 2022 Donna J. Boley Republican 3 2024 Mike Azinger Republican 3 2022 Amy Grady Republican 4 2024 Eric J. Tarr Republican 4 2022 Robert H. Plymale Democrat 5 2024 Mike Woelfel Democrat 5 2022 Chandler Swope Republican 6 2024 Mark R Maynard Republican 6 2022 Rupie Phillips Republican 7 2024 Ron Stollings Democrat 7 2022 Glenn Jeffries Democrat 8 2024 Richard Lindsay Democrat 8 2022 David Stover Republican 9 2024 Rollan A. Roberts Republican 9 2022 Jack Woodrum Republican 10 2024 Stephen Baldwin Democrat 10 2022 Robert Karnes Republican 11 2024 Bill Hamilton Republican 11 2022 Patrick Martin Republican 12 2024 Mike Romano Democrat 12 2022 Mike Caputo Democrat 13 2024 Robert D. -

S/L Sign on Letter Re: Rescue Plan State/Local
February 17, 2021 U.S. House of Representatives Washington, D.C. 20515 U.S. Senate Washington, D.C. 20510 Dear Members of Congress: As elected leaders representing communities across our nation, we are writing to urge you to take immediate action on comprehensive coronavirus relief legislation, including desperately needed funding for states, counties, cities, and schools, and an increase in states’ federal medical assistance percentage (FMAP). President Biden’s ambitious $1.9 trillion American Rescue Plan will go a long way towards alleviating the significant financial strain COVID-19 has placed on our states, counties, cities, and schools, and the pocketbooks of working families. Working people have been on the frontlines of this pandemic for nearly a year and have continued to do their jobs during this difficult time. Dedicated public servants are still leaving their homes to ensure Americans continue to receive the essential services they rely upon: teachers and education workers are doing their best to provide quality education and keep their students safe, janitors are still keeping parks and public buildings clean, while healthcare providers are continuing to care for the sick. Meanwhile, it has been ten months since Congress passed the CARES Act Coronavirus Relief Fund to support these frontline workers and the essential services they provide. Without significant economic assistance from the federal government, many of these currently-middle class working families are at risk of falling into poverty through no fault of their own. It is a painful irony that while many have rightly called these essential workers heroes, our country has failed to truly respect them with a promise to protect them and pay them throughout the crisis. -

Wild Blueberry Commission
SEN. NATHAN LIBBY, SENATE CHAIR REP. GENEVIEVE MCDONALD, HOUSE CHAIR MEMBERS: MAINE STATE LEGISLATURE SEN. LISA KEIM GOVERNMENT OVERSIGHT COMMITTEE SEN. DONNA BAILEY SEN. RICHARD BEN NETT SEN. JEFFREY TIMBERLAKE SEN. ELOISE VITELLI REP. KATHLEEN R. J . DILLINGHAM REP. AMY ARATA REP. H . SAWIN MILLETT, JR. REP. MARGARET O ’ NEIL REP. HOLLY STOVER Date: March 5, 2021 To: Senator James Dill, Senate Chair Representative Margaret O’Neil, House Chair Joint Standing Committee on Agriculture, Conservation and Forestry From: Senator Nathan L. Libby, Senate Chair Representative Genevieve McDonald, House Chair Government Oversight Committee RE: Wild Blueberry Commission At its February 26, 2021 meeting, the Government Oversight Committee (GOC) considered a request for review of the Wild Blueberry Commission, which was presented by Senator Marianne Moore on behalf of a group of 6 legislators. A copy of the written request for review, submitted by letter to the GOC on February 28, 2020, is attached for your reference. We are writing to request the assistance and input of the ACF committee regarding the requested review of the Wild Blueberry Commission from your standpoint as the policy committee with oversight of the commission. To assist us in our decision regarding the review request, we would appreciate receiving your input and any recommendations by March 26, 2021. To inform your input on this matter, the GOC recommends you consider the following actions: 1. Holding a meeting with the ACF committee chairs, Senator Moore and other Legislative sponsors of the request, as appropriate; and 2. Inviting the Legislative sponsors of the request and representatives of the Wild Blueberry Commission and its staff to brief the committee and provide relevant documents related to the questions posed in the request.