Pelvic Organ Prolapse: - a Guide for Women
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

What Is a Hysterectomy?
Greenwich Hospital What is a Hysterectomy? PATIENT/FAMILY INFORMATION SHEET What is a Hysterectomy? A hysterectomy is the surgical removal of the uterus (womb). Sometimes the fallopian tubes, ovaries, and cervix are removed at the same time that the uterus is removed. When the ovaries and both tubes are removed, this is called a bilateral salpingo- oophorectomy. There are three types of hysterectomies: • A complete or total hysterectomy, which is removal of the uterus and cervix. • A partial or subtotal hysterectomy, which is removal of the upper portion of the uterus, leaving the cervix in place. • A radical hysterectomy, which is removal of the uterus, cervix, the upper part of the vagina, and supporting tissue. If you have not reached menopause yet, a hysterectomy will stop your monthly periods. You also will not be able to get pregnant. How is a hysterectomy performed? A hysterectomy can be performed in three ways: • Abdominal hysterectomy: The surgeon will make a cut, or incision, in your abdomen either vertically (up and down) in the middle of the abdomen below the umbilicus (belly button); or horizontally (side ways) in the pelvic area. The horizontal incision is sometimes referred to as a “bikini” incision and is usually hidden by undergarments. • Vaginal hysterectomy: The surgeon goes through the vagina and the incision is on the inside of the vagina, not on the outside of the body. • Laparoscopically assisted vaginal hysterectomy: This involves using a small, telescope-like device called a laparoscope, which is inserted into the abdomen through a small cut. This brings light into the abdomen so that the surgeon can see inside. -

Perceived Gynecological Morbidity Among Young Ever-Married Women
Perceived Gynecological Morbidity among Young ever-married Women living in squatter settlements of Karachi, Pakistan Pages with reference to book, From 92 To 97 Fatima Sajan,Fariyal F. Fikree ( Department of Community Health Sciences, The Aga Khan University, Karachi, Pakistan. ) Abstract Background: Community-based information on obstetric and gynecological morbidity in developing countries is meager and nearly non-existent in Pakistan. Objectives: To estimate the prevalence of specific gynecological morbidities and investigate the predictors of pelvic inflammatory disease Methods: Users and non-users of modem contraceptives were identified from eight squatter settlements of Karachi, Pakistan and detailed information on basic demographics, contraceptive use, female mobility, decision-making and gynecological morbidities were elicited. Results: The perceived prevalence of menstrual disorders were 45.3%, uterine prolapse 19.1%, pelvic inflammatory disease 12.8% and urinary tract infection 5.4%. The magnitude of gynecological morbidity was high with about 55% of women reporting at least one gynecological morbidity though fewer reported at least two gynecological morbidities. Significant predictors of pelvic inflammatory disease were intrauterine contraceptive device users (OR = 3.1; 95% CI 1.7- 5.6), age <20 years (OR = 2.3; 95% CI 1.1 - 4.8) and urban life style (OR = 2.1; 95% CI 1.0-4.6). Conclusion: There is an immense burden of reproductive ill-health and a significant association between eyer users of intrauterine contraceptive device and pelvic inflammatory disease. We therefore suggest improvement in the quality of reproductive health services generally, but specifically for family planning services (JPMA 49:92, 1999). Introduction Gynecological morbidity has been defined as structural and functional disorders of the genital tract which are not directly related to pregnancy, delivery and puerperium. -

Uterine Prolapse
Uterine prolapse Definition Uterine prolapse is falling or sliding of the uterus from its normal position in the pelvic cavity into the vaginal canal. Alternative Names Pelvic relaxation; Pelvic floor hernia Causes The uterus is normally supported by pelvic connective tissue and the pubococcygeus muscle, and held in position by special ligaments. Weakening of these tissues allows the uterus to descend into the vaginal canal. Tissue trauma sustained during childbirth, especially with large babies or difficult labor and delivery, is typically the cause of muscle weakness. The loss of muscle tone and the relaxation of muscles, which are both associated with normal aging and a reduction in the female hormone estrogen, are also thought to play an important role in the development of uterine prolapse. Descent can also be caused by a pelvic tumor, however, this is fairly rare. Uterine prolapse occurs most commonly in women who have had one or more vaginal births, and in Caucasian women. Other conditions associated with an increased risk of developing problems with the supportive tissues of the uterus include obesity and chronic coughing or straining. Obesity places additional strain on the supportive muscles of the pelvis, as does excessive coughing caused by lung conditions such as chronic bronchitis and asthma. Chronic constipation and the pushing associated with it causes weakness in these muscles. Symptoms z Sensation of heaviness or pulling in the pelvis z A feeling as if "sitting on a small ball" z Low backache z Protrusion from the vaginal opening (in moderate to severe cases) z Difficult or painful sexual intercourse Exams and Tests A pelvic examination (with the woman bearing down) reveals protrusion of the cervix into the lower part of the vagina (mild prolapse), past the vaginal introitus/opening (moderate prolapse), or protrusion of the entire uterus past the vaginal introitus/opening (severe prolapse). -

Management of Uterine Prolapse: Is Hysterectomy Necessary?
DOI: 10.1111/tog.12220 2016;18:17–23 Review The Obstetrician & Gynaecologist http://onlinetog.org Management of uterine prolapse: is hysterectomy necessary? a b b, Helen Jefferis MRCOG, Simon Robert Jackson MD FRCOG, Natalia Price MD MRCOG * aSubspeciality Trainee in Urogynaecology, Department of Urogynaecology, Women’s Centre, John Radcliffe Hospital, Headley Way, Oxford OX3 9DU, UK bConsultant Urogynaecologist, Department of Urogynaecology, Women’s Centre, John Radcliffe Hospital, Headley Way, Oxford OX3 9DU, UK *Correspondence: Natalia Price. Email: [email protected] Accepted on 1 June 2015 Key content Fertility preservation remains the one absolute indication for Management of uterine prolapse is currently heavily influenced by hysteropexy. Other potential advantages include stronger apical patient and surgeon preferences. support and reduced vaginal surgery. The traditional approach to uterine prolapse is vaginal Colpocleisis remains a valid option for a small cohort of patients. hysterectomy. However, this does not address the underlying Learning objectives deficiency in connective tissue pelvic floor support, and prolapse Options for the management of uterine prolapse. recurrence is common. How to help patients decide on a management plan. Uterine preservation surgery is increasing in popularity, both with surgeons and patients; there is currently little evidence to show Keywords: colpocleisis / hysteropexy / pelvic organ prolapse / superior outcome to hysterectomy. uterine preservation surgery / vaginal hysterectomy Please cite this paper as: Jefferis H, Jackson SR, Price N. Management of uterine prolapse: is hysterectomy necessary? The Obstetrician & Gynaecologist 2016;18: 17–23. DOI: 10.1111/tog.12220 Introduction significantly associated with regression of prolapse, leading the authors to suggest that the damage obesity causes to the When a woman presents with pelvic organ prolapse, the pelvic floor may be irreversible. -

Uterine Prolapse Treatment Without Hysterectomy
Uterine Prolapse Treatment Without Hysterectomy Authored by Amy Rosenman, MD Can The Uterine Prolapse Be Treated Without Hysterectomy? A Resounding YES! Many gynecologists feel the best way to treat a falling uterus is to remove it, with a surgery called a hysterectomy, and then attach the apex of the vagina to healthy portions of the ligaments up inside the body. Other gynecologists, on the other hand, feel that hysterectomy is a major operation and should only be done if there is a condition of the uterus that requires it. Along those lines, there has been some debate among gynecologists regarding the need for hysterectomy to treat uterine prolapse. Some gynecologists have expressed the opinion that proper repair of the ligaments is all that is needed to correct uterine prolapse, and that the lengthier, more involved and riskier hysterectomy is not medically necessary. To that end, an operation has been recently developed that uses the laparoscope to repair those supporting ligaments and preserve the uterus. The ligaments, called the uterosacral ligaments, are most often damaged in the middle, while the lower and upper portions are usually intact. With this laparoscopic procedure, the surgeon attaches the intact lower portion of the ligaments to the strong upper portion of the ligaments with strong, permanent sutures. This accomplishes the repair without removing the uterus. This procedure requires just a short hospital stay and quick recovery. A recent study from Australia found this operation, that they named laparoscopic suture hysteropexy, has excellent results. Our practice began performing this new procedure in 2000, and our results have, likewise, been very good. -

Pessary Information
est Ridge obstetrics & gynecology, LLP 3101 West Ridge Road, Rochester, NY 14626 1682 Empire Boulevard, Webster, NY 14580 www.wrog.org Tel. (585) 225‐1580 Fax (585) 225‐2040 Tel. (585) 671‐6790 Fax (585) 671‐1931 USE OF THE PESSARY The pessary is one of the oldest medical devices available. Pessaries remain a useful device for the nonsurgical treatment of a number of gynecologic conditions including pelvic prolapse and stress urinary incontinence. Pelvic Support Defects The pelvic organs including the bladder, uterus, and rectum are held in place by several layers of muscles and strong tissues. Weaknesses in this tissue can lead to pelvic support defects, or prolapse. Multiple vaginal deliveries can weaken the tissues of the pelvic floor. Weakness of the pelvic floor is also more likely in women who have had a hysterectomy or other pelvic surgery, or in women who have conditions that involve repetitive bearing down, such as chronic constipation, chronic coughing or repetitive heavy lifting. Although surgical repair of certain pelvic support defects offers a more permanent solution, some patients may elect to use a pessary as a very reasonable treatment option. Classification of Uterine Prolapse: Uterine prolapse is classified by degree. In first‐degree uterine prolapse, the cervix drops to just above the opening of the vagina. In third‐degree prolapse, or procidentia, the entire uterus is outside of the vaginal opening. Uterine prolapse can be associated with incontinence. Types of Vaginal Prolapse: . Cystocele ‐ refers to the bladder falling down . Rectocele ‐ refers to the rectum falling down . Enterocele ‐ refers to the small intestines falling down . -

Pelvic Organ Prolapse
Pelvic Organ Prolapse An estimated 34 million women worldwide are affected by pelvic organ prolapse (POP). POP is found to be a difficult topic for women to talk about. POP is essentially a form of herniation of the vaginal wall due to laxity of the collagen, fascia and muscles within the pelvis and surrounding the vagina. Pelvic Organ Prolapse incudes: • Cystocele: bladder herniation through the upper vaginal wall. • Rectocele: rectum bulging through the lower vaginal wall. • Enterocele: bowel bulging through the deep vaginal wall. • Uterine prolapse: uterus falling into the vaginal wall. Detection and Diagnosis Common causes and symptoms of pelvic organ prolapse may be the sensation of a mass bulging from the vaginal region and a feeling of pelvic heaviness as well as vaginal irritation. The prolapse may occur at the level of the bladder bulging through the vagina or the rectum bulging through the bottom of the vagina. For that reason, we describe it as a herniating process through the vaginal wall. Once the symptoms are established, a proper history and physical should be obtained from a specialized physician/surgeon. Common causes we know are pregnancy, especially with vaginal childbirth. Vaginal childbirth increases a women’s risk of prolapse as well as urinary incontinence greater than an elective C-section. An emergency C-section would then cause a risk factor three times higher in terms of urinary incontinence as well as vaginal vault prolapse. The collagen-type tissue within the patient’s pelvis is a known cause of a patient being prone to vaginal vault prolapse as well as urinary incontinence. -

Pelvic Organ Prolapse
Quality ID #429: Pelvic Organ Prolapse: Preoperative Screening for Uterine Malignancy – National Quality Strategy Domain: Patient Safety – Meaningful Measure Area: Preventable Healthcare Harm 2019 COLLECTION TYPE: MEDICARE PART B CLAIMS MEASURE TYPE: Process – High Priority DESCRIPTION: Percentage of patients who are screened for uterine malignancy prior to vaginal closure or obliterative surgery for pelvic organ prolapse INSTRUCTIONS: This measure is to be submitted each time a prolapse organ repair surgery is performed during the performance period. There is no diagnosis associated with this measure. This measure may be submitted by Merit-based Incentive Payment System (MIPS) eligible clinicians who perform the quality actions described in the measure based on the services provided and the measure-specific denominator coding. Measure Submission Type: Measure data may be submitted by individual MIPS eligible clinicians using Medicare Part B claims. The listed denominator criteria are used to identify the intended patient population. The numerator quality-data codes included in this specification are used to submit the quality actions allowed by the measure on the claim form(s). All measure- specific coding should be submitted on the claim(s) representing the denominator eligible encounter and selected numerator option. DENOMINATOR: All patients undergoing surgery for pelvic organ prolapse involving vaginal closure/obliterative procedure Denominator Criteria (Eligible Cases): All patients, regardless of age AND Patient procedure during -

Histopathology Findings of the Pelvic Organ Prolapse
Review Histopathology fndings of the pelvic organ prolapse FERNANDA M.A. CORPAS1, ANDRES ILLARRAMENDI2, FERNANDA NOZAR3, BENEDICTA CASERTA4 1 Asistente Clínica Ginecotocológica A CHPR, 2 Residente de Ginecología, Clínica Ginecotocológica A CHPR, 3 Profesora Adjunta Clínica Ginecotocológica A CHPR, 4 Jefa del servicio de Anatomía Patológica del CHPR, Presidenta de la Sociedad de Anatomía Patológica del Uruguay, Centro Hospitalario Pereira Rossell (Chpr), Montevideo, Uruguay Abstract: Pelvic organ prolapse is a benign condition, which is the result of a weakening of the different components that provide suspension to the pelvic foor. Surgical treatment, traditionally involve a vaginal hysterectomy, although over the last few decades the preservation of the uterus has become more popular. The objective of the paper is to analyze the characteristics of those patients diagnosed with pelvic organ prolapse, whose treatment involved a vaginal hysterectomy and its correlation to the histopathological characteristics. Retrospective, descriptive study. Data recovered from the medical history of patients that underwent surgical treatment for pelvic organ prolapse through vaginal hysterectomy, were analyzed in a 2 years period, in the CHPR, and compared to the pathology results of the uterus. At the level of the cervix, 58,2% presented changes related to the prolapse (acantosis, para and hyperqueratosis) and 43,6% chronic endocervicitis. Findings in the corpus of the uterus were 58,2% atrophy of the endometrium, 21% of endometrial polyps and 30.9% leiomiomas and 1 case of simple hyperplasia without cellular atypias. No malignant lesions were found. The pathology results of the uterus reveal the presence of anatomical changes related to the pelvic organ prolapse and in accordance to the age of the patient, as well as associated pathologies to a lesser extent. -
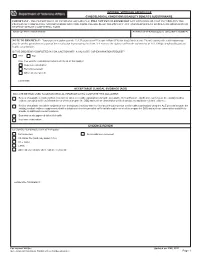
Gynecological-DBQ
INTERNAL VETERANS AFFAIRS USE GYNECOLOGICAL CONDITIONS DISABILITY BENEFITS QUESTIONNAIRE IMPORTANT - THE DEPARTMENT OF VETERANS AFFAIRS (VA) WILL NOT PAY OR REIMBURSE ANY EXPENSES OR COST INCURRED IN THE PROCESS OF COMPLETING AND/OR SUBMITTING THIS FORM. PLEASE READ THE PRIVACY ACT AND RESPONDENT BURDEN INFORMATION ON REVERSE BEFORE COMPLETING FORM. NAME OF PATIENT/VETERAN PATIENT/VETERAN'S SOCIAL SECURITY NUMBER NOTE TO PHYSICIAN - Your patient is applying to the U.S. Department of Veterans Affairs (VA) for disability benefits. VA will consider the information you provide on this questionnaire as part of their evaluation in processing the claim. VA reserves the right to confirm the authenticity of ALL DBQs completed by private health care providers. IS THIS DBQ BEING COMPLETED IN CONJUNCTION WITH A VA21-2507, C&P EXAMINATION REQUEST? YES NO If no, how was the examination completed (check all that apply)? In-person examination Records reviewed Other, please specify: Comments: ACCEPTABLE CLINICAL EVIDENCE (ACE) INDICATE METHOD USED TO OBTAIN MEDICAL INFORMATION TO COMPLETE THIS DOCUMENT: Review of available records (without in-person or video telehealth examination) using the Acceptable Clinical Evidence (ACE) process because the existing medical evidence provided sufficient information on which to prepare the DBQ and such an examination will likely provide no additional relevant evidence. Review of available records in conjunction with a telephone interview with the Veteran (without in-person or telehealth examination) using the ACE process because the existing medical evidence supplemented with a telephone interview provided sufficient information on which to prepare the DBQ and such an examination would likely provide no additional relevant evidence. -

Prevalence of Pelvic Floor Disorders in Various Gynecologic Cancers
42 Buchsbaum G1, Doyle P1, Glantz J C1, Sato H1, Thomas S1 1. University of Rochester PREVALENCE OF PELVIC FLOOR DISORDERS IN VARIOUS GYNECOLOGIC CANCERS Hypothesis / aims of study The prevalence of urinary incontinence and pelvic organ prolapsed is highest in women beyond childbearing age. This is also the group that is at highest risk for gynaecologic cancer. In a recent retrospective study of patients presenting to a gynaecologic oncology office revealed a prevalence of urinary incontinence of 53.2% and of pelvic organ prolapse to or beyond the hymen of 8.7%.1 Risk factors differ for various gynaecologic cancers. Endometrial cancer is associated with unopposed estrogen exposure and obesity, ovarian cancer with nulliparity and familial factors, and cervical cancer with smoking and HPV. Pelvic floor disorders are associated with familial factors, age, parity and obesity. Based on different risk factors for different gynaecologic malignancies, it would be reasonable to assume that the prevalence of pelvic floor disorders varies between gynaecologic malignancies. Since this hypothesis has not been explored previously, we assessed the prevalence of urinary incontinence and pelvic organ prolapse stratified by type of gynaecologic malignancy: endometrial, cervical, and ovarian. We hypothesized that women with endometrial cancer will have a higher prevalence of pelvic floor disorders given both share common major risk factors. The objective of this study was to determine whether the prevalence of urinary incontinence and pelvic organ prolapse differs - in patients with different gynecological malignancies such as endometrial, ovarian, and cervical cancer and - in women with gynecologic malignancy compared to women presenting with benign gynecologic conditions. -

Painful Sex (Dyspareunia) Labia Majora a Guide for Women Labia Minora 1
Clitoris Painful Sex (Dyspareunia) Labia majora A Guide for Women Labia minora 1. What is dyspareunia? Perineum 2. How common is dyspareunia? 3. What causes dyspareunia? 4. How is dyspareunia diagnosed? 5. How is dyspareunia treated? These issues may start suddenly or occur gradually over a period of time and may be traced back to an event such as What is dysperunia? a previous infection. Additionally, certain disorders of the Dyspareunia, or female sexual pain, is a term used to describe urethra (the tube through which urine is emptied from the pelvic and/or vaginal pain during intercourse. The duration of bladder) can cause significant pain involving the vagina. Ex- the pain can be limited to the duration of intercourse but may last amples include urethritis (inflammation/pain in the urethra, for up to 24 hours after intercourse has finished. The duration sometimes caused by sexually transmitted diseases) and of symptoms varies widely and sometimes can be traced back urethral diverticulum (a weakness in the wall of the urethra to a specific time or event. It is often difficult to diagnose the which forms a pocket in which urine can be trapped). exact source of discomfort (muscular, vascular, foreign bodies, • Musculoskeletal issues. At times, women will describe a surgery, trauma, aging, emotional) as well as to implement the pain like being ‘stabbed in the vagina’ or chronic soreness. correct treatment options. This can be related to increased tension of the pelvic floor musculature so that it cannot properly relax. This phenom- How common is dyspareunia? enon (levator spasm) can cause constant or intermittent pain Dyspareunia is common but probably under-reported.