Kaimur Table of Contents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

LIST of DISTRICTS for WALKATHON on 2Nd FEB 2020
LIST OF DISTRICTS FOR WALKATHON ON 2nd FEB 2020 Sr.No. District Headquarters State Company Class of City 1 Pune Pune Maharashtra BPCL Tier I 2 Malappuram Malappuram Kerala BPCL Tier II 3 Thiruvananthapuram Thiruvananthapuram Kerala BPCL Tier II 4 Ernakulam Kakkanad Kerala BPCL Tier II 5 Thrissur Thrissur Kerala BPCL Tier II 6 Kozhikode Kozhikode Kerala BPCL Tier II 7 Palakkad Palakkad Kerala BPCL Tier II 8 Kollam Kollam Kerala BPCL Tier II 9 Kannur Kannur Kerala BPCL Tier II 10 Kottayam Kottayam Kerala BPCL Tier II 11 Nashik Nashik Maharashtra BPCL Tier II 12 Nagpur Nagpur Maharashtra BPCL Tier II 13 Solapur Solapur Maharashtra BPCL Tier II 14 Kolhapur Kolhapur Maharashtra BPCL Tier II 15 Aurangabad Aurangabad Maharashtra BPCL Tier II 16 Nanded Nanded Maharashtra BPCL Tier II 17 Amravati Amravati Maharashtra BPCL Tier II 18 Sangli Sangli Maharashtra BPCL Tier II 19 Ludhiana Ludhiana Punjab BPCL Tier II 20 Amritsar Amritsar Punjab BPCL Tier II 21 Jalandhar Jalandhar Punjab BPCL Tier II 22 Allahabad Allahabad Uttar Pradesh BPCL Tier II 23 Moradabad Moradabad Uttar Pradesh BPCL Tier II 24 Lucknow Lucknow Uttar Pradesh BPCL Tier II 25 Bareilly Bareilly Uttar Pradesh BPCL Tier II 26 Gorakhpur Gorakhpur Uttar Pradesh BPCL Tier II 27 Mathura Mathura Uttar Pradesh BPCL Tier II 28 Jhansi Jhansi Uttar Pradesh BPCL Tier II 29 Paschim Bardhaman Asansol West Bengal BPCL Tier II 30 Darjeeling Darjeeling West Bengal BPCL Tier II 31 East Champaran Motihari Bihar BPCL Tier III 32 Muzaffarpur Muzaffarpur Bihar BPCL Tier III 33 Madhubani Madhubani Bihar -

DISTRICT-LEVEL STUDY on CHILD MARRIAGE in INDIA What Do We Know About the Prevalence, Trends and Patterns?
DISTRICT-LEVEL STUDY ON CHILD MARRIAGE IN INDIA What do we know about the prevalence, trends and patterns? PADMAVATHI SRINIVASAN NIZAMUDDIN KHAN RAVI VERMA International Center for Research on Women (ICRW), India DORA GIUSTI JOACHIM THEIS SUPRITI CHAKRABORTY United Nations International Children’s Educational fund (UNICEF), India International Center for Research on Women ICRW where insight and action connect 1 1 This report has been prepared by the International Center for Research on Women, in association with UNICEF. The report provides an analysis of the prevalence of child marriage at the district level in India and some of its key drivers. Suggested Citation: Srinivasan, Padmavathi; Khan, Nizamuddin; Verma, Ravi; Giusti, Dora; Theis, Joachim & Chakraborty, Supriti. (2015). District-level study on child marriage in India: What do we know about the prevalence, trends and patterns? New Delhi, India: International Center for Research on Women. 2 3 ACKNOWLEDGEMENT The International Center for Research on Women (ICRW), New Delhi, in collaboration with United Nations Children’s Fund (UNICEF), New Delhi, conducted the District-level Study on Child Marriage in India to examine and highlight the prevalence, trends and patterns related to child marriage at the state and district levels. The first stage of the project, involving the study of prevalence, trends and patterns, quantitative analyses of a few key drivers of child marriage, and identification of state and districts for in-depth analysis, was undertaken and the report prepared by Dr. Padmavathi Srinivasan, with contributions from Dr. Nizamuddin Khan, under the strategic guidance of Dr. Ravi Verma. We would like to acknowledge the contributions of Ms. -

Demp Kaimur (Bhabua)
DEMP KAIMUR (BHABUA) SL SUBJECT REMARKS NO. 1 2 3 1. DISTRICT BRIEF PROFILE DISTRICT POLITICAL MAP KEY STATISTICS BRIEF NOTES ON THE DISTRICT 2. POLLING STATIONS POLLING STATIONS LOCATIONS AND BREAK UP ACCORDING TO NO. OF PS AT PSL POLLING STATION OVERVIEW-ACCESSIBILITY POLLING STATION OVERVIEW-TELECOM CONNECTIVITY POLLING STATION OVERVIEW-BASIC MINIMUM FACILITIES POLLING STATION OVERVIEW-INFRASTRUCTURE VULNERABLES PS/ELECTIORS POLLING STATION LOCATION WISE ACCESSIBILITY & REACH DETAILS POLLING STATION WISE BASIC DETAISLS RPOFILING AND WORK TO BE DONE 3. MANPOWER PLAN CADRE WISE PERSONNEL AVAILABILITY FOR EACH CATEGORY VARIOUS TEAMS REQUIRED-EEM VARIOUS TEAMS REQUIRED-OTHERS POLLING PERSONNEL REQUIRED OTHER PERSONNEL REQUIRED PERSONNEL REQUIRED & AVAILABILITY 4. COMMUNICATION PLAN 5. POLLING STAFF WELFARE NODAL OFFICERS 6. BOOTH LIST 7. LIST OF SECTOR MAGISTRATE .! .! .! .! !. .! Assembly Constituency map State : BIHAR .! .! District : KAIMUR (BHABUA) AC Name : 205 - Bhabua 2 0 3 R a m g a r h MOHANIA R a m g a r h 9 .! ! 10 1 2 ! ! ! 5 12 ! ! 4 11 13 ! MANIHAR!I 7 RUP PUR 15 3 ! 14 ! ! 6 ! 8 73 16 ! ! ! RATWAR 19 76 ! 2 0 4 ! 18 .! 75 24 7774 17 ! M o h a n ii a (( S C )) ! ! ! 20 23 DUMRAITH ! ! 78 ! 83 66 21 !82 ! ! .! 32 67 DIHARA 22 ! ! 68 ! 30 80 ! 26 ! 31 79 ! ! ! ! 81 27 29 33 ! RUIYA 70 ! 25 ! 2 0 9 69 ! 2 0 9 KOHARI ! 28 KAITHI 86 ! K a r g a h a r 85 ! 87 72 K a r g a h a r ! ! 36 35 ! 71 60 ! ! ! 34 59 52 38 37 ! ! ! ! 53 KAIMUR (BHABUA) BHABUA (BL) 64 ! ! 40 84 88 62 55 MIRIA ! ! ! ! BAHUAN 54 ! 43 39 !89 124125 63 61 ! ! -

Vlcc Merchant VLCC KOTWALI PATNA1 Patna 800001 PATNA Vlcc
BIHAR MERCHANT NAME STORE NAME ADDRESS1 PINCODE STORE CITY Vlcc Merchant VLCC KOTWALI PATNA1 patna 800001 PATNA Vlcc Merchant VLCC ALAMGANJ CITY PATNA2 patna 800013 PATNA Samsung Mobile AXIS Ritik In Touch -Patna Verma Complex Boring Road Bihd1080 403601 PATNA Reliance Digital RDKHAJPURAPATNA Plot No 968, 998, 969, 971, 970, Thana No-11, 800014 PATNA Samsung Mobile BIHD19538 SHREE HARI Om Vihar Complex, Nala Road 800004 PATNA RELIANCE RETAIL RR Kankarbagh Patna B - 51, Sadho Shivam Complex, Type A, Thana No- 9 800008 PATNA RELIANCE RETAIL RR Gujri Bazaar Patna Holding No 30- 25-18A,Plot No - 950,Circle No-110 800008 PATNA RELIANCE RETAIL RD ASHOK RAJPATH PATNA Ward No 4130, Circle No 27, Circle, Bankipur 800004 PATNA RELIANCE RETAIL RR 7949 Civil Line GB Road Gaya Khata No 342, Plot No - 1201 Ka, Kha, Ga/ 13915 823001 GAYA RELIANCE RETAIL RD 7951 RAMPUR GAYA BIHAR Khata No 2252, Plot No 5585, 5411, Ward No 31 823001 GAYA RELIANCE RETAIL RD 7948 BATA MORE GAYA House No 355, Ward No 18, Khata No 118 823001 GAYA RELIANCE RETAIL RD 7238 BAHADURPUR PATNA Holding No 594/2/147/2 (Old), Ward No- 46, Circle 800020 PATNA RELIANCE RETAIL RD Patliputra Manpura C 22, Patliputra Industrial Estate 800013 PATNA RELIANCE RETAIL RD DHAKANPURA Shop No 213, Ground Floor, Brij Laxmi Mansion 800005 PATNA RELIANCE RETAIL RD 7801 DANAPUR PATNA Ward No 22, Holding No 23 Circle 801503 PATNA RELIANCE RETAIL RD 7822 BAILEY ROAD PATNA Mouza Rukanpura, P S Danapur Thana, No 18 800014 PATNA NOKIA MOBILE MOBTEL FRAZER RD PATNA Frazer Road 800001 PATNA RELIANCE RETAIL RD 6384 PHULWARI PATNA Holding No. -

Of India 100935 Parampara Foundation Hanumant Nagar ,Ward No
AO AO Name Address Block District Mobile Email Code Number 97634 Chandra Rekha Shivpuri Shiv Mandir Road Ward No 09 Araria Araria 9661056042 [email protected] Development Foundation Araria Araria 97500 Divya Dristi Bharat Divya Dristi Bharat Chitragupt Araria Araria 9304004533 [email protected] Nagar,Ward No-21,Near Subhash Stadium,Araria 854311 Bihar Araria 100340 Maxwell Computer Centre Hanumant Nagar, Ward No 15, Ashram Araria Araria 9934606071 [email protected] Road Araria 98667 National Harmony Work & Hanumant Nagar, Ward No.-15, Po+Ps- Araria Araria 9973299101 [email protected] Welfare Development Araria, Bihar Araria Organisation Of India 100935 Parampara Foundation Hanumant Nagar ,Ward No. 16,Near Araria Araria 7644088124 [email protected] Durga Mandir Araria 97613 Sarthak Foundation C/O - Taranand Mishra , Shivpuri Ward Araria Araria 8757872102 [email protected] No. 09 P.O + P.S - Araria Araria 98590 Vivekanand Institute Of 1st Floor Milan Market Infront Of Canara Araria Araria 9955312121 [email protected] Information Technology Bank Near Adb Chowk Bus Stand Road Araria Araria 100610 Ambedkar Seva Sansthan, Joyprakashnagar Wardno-7 Shivpuri Araria Araria 8863024705 [email protected] C/O-Krishnamaya Institute Joyprakash Nagar Ward No -7 Araria Of Higher Education 99468 Prerna Society Of Khajuri Bazar Araria Bharga Araria 7835050423 [email protected] Technical Education And ma Research 100101 Youth Forum Forbesganj Bharga Araria 7764868759 [email protected] -

State District Name of Bank Bank Branch/ Financial Literacy Centre
State District Name of Bank Branch/ Address ITI Code ITI Name ITI Address State District Phone Email Bank Financial Category Number Literacy Centre Bihar Araria State Araria Lead Bank Office, PR10000055 Al-Sahaba Industrial P Alamtala Forbesganj Bihar Araria NULL Bank of ADB Building, Training Institute India Araria, Pin- 854311 Bihar Arwal PNB ARWAL ARWAL PR10000083 Adarsh ITC P Umerabad Bihar Arwal NULL Bihar Arwal PNB ARWAL ARWAL PR10000284 Shakuntalam ITC P Prasadi English Bihar Arwal NULL Bihar Arwal PNB ARWAL ARWAL PR10000346 Aditya ITC P At. Wasilpur, Main Road, Bihar Arwal NULL P.O. Arwal, Bihar Arwal PNB ARWAL ARWAL PR10000396 Vikramshila Private P At. Rojapar, P.O. Arwal Bihar Arwal NULL ITI Bihar Arwal PNB ARWAL ARWAL PR10000652 Ram Bhaman Singh P At-Purani Bazar P.o+P.S- Bihar Arwal NULL Private ITI Arwal Bihar Arwal PNB ARWAL ARWAL PR10000677 Sukhdeo Institute Of P Kurtha, Arwal Bihar Arwal NULL Tecnology Private ITI, Bihar Arwal PNB ARWAL ARWAL PR10000707 Dr. Rajendra Prasad P Mubarkpur, Kurtha Arwal Bihar Arwal NULL Private ITI, Bihar Aurangabad PUNJAB DAUDNAGAR DAUDNAGAR PR10000027 New Sai Private ITI- P Aurangabad Road, Bihar Aurangabad NULL NATIONA Bhakharuan More, , Tehsil- L BANK Daudnagar , , Aurangabad - 824113 Bihar Aurangabad PUNJAB AURANGABAD AURANGABAD PR10000064 Adharsh Industrial P Josai More Udyog Bihar Aurangabad NULL NATIONA Training Centre Pradhikar Campus L BANK Bihar Aurangabad MADHYA DAUDNAGAR DAUDNAGAR PR10000108 Sardar Vallabh Bhai P Daudnagar Bihar Aurangabad NULL BIHAR Patel ITC, Daudnagar GRAMIN BANK Bihar Aurangabad MADHYA DAUDNAGAR DAUDNAGAR PR10000142 Adarsh ITC, P AT-,Growth centre ,Jasoia Bihar Aurangabad NULL BIHAR Daudnagar More Daudnagar GRAMIN BANK Bihar Aurangabad PUNJAB RATANUA RATANUA PR10000196 Progresive ITC P At-Growth Center Josia Bihar Aurangabad NULL NATIONA More L BANK Bihar Aurangabad MADHYA DAUDNAGAR DAUDNAGAR PR10000199 Arya Bhatt ITC P Patel Nagar, Daud Nagar Bihar Aurangabad NULL BIHAR GRAMIN BANK Bihar Aurangabad PUNJAB OLD GT RD. -

Agro-Economic Alerts Aiding the Future of India’S Farmers and Agriculture
Agro-Economic Alerts Aiding the future of India’s farmers and agriculture Emerging Critical Situations and Threats in India’s Agricultural Economy Issue 9, January 2019 Alert 1 – Onion Price Increase and Volatility Likely Due to Shortage Alert 2 – Problems of Palk Bay Fishermen in Tamil Nadu Alert 3 – Problem of Non-Germination of Certified Seeds in Bihar Compiled and Edited by Center for Management in Agriculture (CMA) Indian Institute of Management Ahmedabad Contact: Prof. Ranjan Ghosh or Prof. Vasant P. Gandhi Chairperson CMA [email protected] Phone: +91-79-6632-4651 Acknowledgements: Nikita Pandey, Nicky Johnson, Dipali Chauhan Based on Research & For kind attention of: Contributions of: 15 Agro- The Hon’ble Prime Minister’s Office, Economic Research Centers the Ministry of Agriculture and Farmers Welfare, and Units, supported by and all others interested Ministry of Agriculture & Farmers Welfare Alert 1: Onion Price Increase and Volatility Likely Due to Shortage Key highlights now, had been eyeing a bumper crop earlier • The state of Maharashtra has declared as the area under onion cultivation had almost drought in 151 talukas this year (2018-19), doubled in four years due to an upswing in including eight talukas in the Nashik district prices. itself. • The cultivation had picked up pace after • Inadequate rain and water scarcity have led the average wholesale price of the cash to a decline in the summer onion cultivation crop had hit an all-time high of Rs. 5,700 to 84 thousand hectares. The area under per quintal in August 2015. The crop area in cultivation for summer onions has halved this Nasik increased from 1.24 lakh hectares in year. -
Cbwtf/1838/2019
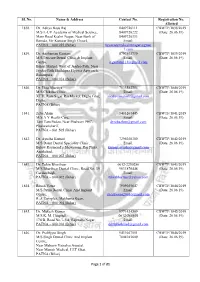
Sl. No. Name & Address Contact No. Registration No. Allotted 1838. Dr. Aditya Basu Raj 8409726111 CBWTF/1838/2019 M/S L-UV Academy of Medical Science, 8409726222 (Date: 26.06.19) Main Road Keshri Nagar, Near Bank of 8409726333 Baroda, Vir Kunwar Singh Chowk, Email: PATNA – 800 025 (Bihar) luvacademykeshrinagar@gmai l.com 1839. Dr. Anshuman Gautam 8797503739 CBWTF/1839/2019 M/S Pericare Dental Clinic & Implant Email: (Date: 26.06.19) Centre, [email protected] Bihari Market, West of Jagdeo Path, Near Jagdeo Path Sheikhpra Flyover Approach, Rukanpura, PATNA – 800 014 (Bihar) 1840. Dr. Ekta Bhartiya 7033582754 CBWTF/1840/2019 M/S Chikitsa Clinic, Email: (Date: 26.06.19) XTTI, Ram Sagar Rai Market, Digha Ghat, [email protected] Digha, PATNA (Bihar) 1841. Zeba Alam 9431267445 CBWTF/1841/2019 M/S A Y Health Care, Email: (Date: 26.06.19) Tam Tam Padao, Near Phulwari PHC, [email protected] Phulwarisharif, PATNA – 801 505 (Bihar) 1842. Dr. Ayusha Kumari 7295038300 CBWTF/1842/2019 M/S Daant Dental Speciality Clinic, Email: (Date: 26.06.19) Below Raymond’s Showroom, Raj Plaza, [email protected] Anishabad, PATNA – 800 002 (Bihar) 1843. Dr. Tuhin Bharthuar 0612-2250286 CBWTF/1843/2019 M/S Bharthuar Dental Clinic, Road No. 39, 9631876448 (Date: 26.06.19) Gardanibagh, Email: PATNA – 800 002 (Bihar) [email protected] 1844. Ritesh Vatsa 7909055647 CBWTF/1844/2019 M/S Patna Dental Clinic And Implant Email: (Date: 26.06.19) Centre, [email protected] R. J. Complex, Makhania Kuan, PATNA – 800 004 (Bihar) 1845. Dr. Mukesh Kumar 9771424509 CBWTF/1845/2019 M/S K. -
Observed Rainfall Variability and Changes Over Bihar State
CLIMATE RESEARCH AND SERVICES INDIA METEOROLOGICAL DEPARTMENT MINISTRY OF EARTH SCIENCES PUNE Observed Rainfall Variability and Changes over Bihar State Met Monograph No. : ESSO/IMD/HS/Rainfall Variability/04(2020)/28 Pulak Guhathakurta, Sudeepkumar B L, Preetha Menon, Ashwini Kumar Prasad, Neha Sangwan and S C Advani GOVERNMENT OF INDIA MINISTRY OF EARTH SCIENCES INDIA METEOROLOGICAL DEPARTMENT Met Monograph No.: ESSO/IMD/HS/Rainfall Variability/04(2020)/28 Observed Rainfall Variability and Changes Over Bihar State Pulak Guhathakurta, Sudeepkumar B L, Preetha Menon, Ashwini Kumar Prasad, Neha Sangwan and S C Advani INDIA METEOROLOGICAL DEPARTMENT PUNE - 411005 1 DOCUMENT AND DATA CONTROL SHEET 1 Document Title Observed Rainfall Variability and Changes Over Bihar State 2 Issue No. ESSO/IMD/HS/Rainfall Variability/04(2020)/28 3 Issue Date January 2020 4 Security Unclassified Classification 5 Control Status Uncontrolled 6 Document Type Scientific Publication 7 No. of Pages 27 8 No. of Figures 42 9 No. of References 4 10 Distribution Unrestricted 11 Language English 12 Authors Pulak Guhathakurta, Sudeepkumar B L, Preetha Menon, Ashwini Kumar Prasad, Neha Sangwan and S C Advani 13 Originating Division/ Climate Research Division/ Climate Application & Group User Interface Group/ Hydrometeorology 14 Reviewing and Director General of Meteorology, India Approving Authority Meteorological Department, New Delhi 15 End users Central and State Ministries of Water resources, agriculture and civic bodies, Science and Technology, Disaster Management Agencies, Planning Commission of India 16 Abstract India is in the tropical monsoon zone and receives plenty of rainfall as most of the annual rainfall during the monsoon season every year. However, the rainfall is having high temporal and spatial variability and due to the impact of climate changes there are significant changes in the mean rainfall pattern and their variability as well as in the intensity and frequencies of extreme rainfall events. -

Notice: Centre List of Candidates According to Roll No. For
Centre List of Candidates According to Roll Number Advt. No: 02/2019 Bihar Police Constable Recruitment Candidates Can Check up their Exam Centre for written exam to be held on 20/01/2020 Sl. Centre District Roll No. Roll No. Name & Address of Centre No. Code From To 1 1001 Patna 4410010001 4410012496 College of Commerce Arts and Science, Patna 2 1001 Patna 5510010001 5510012496 College of Commerce Arts and Science, Patna 3 1002 Patna 4410020001 4410022376 A. N. College, Patna. 4 1002 Patna 5510020001 5510022376 A. N. College, Patna. 5 1003 Patna 4410030001 4410031392 T. P. S. College, Chiraiyatand, Patna 6 1003 Patna 5510030001 5510031392 T. P. S. College, Chiraiyatand, Patna 7 1004 Patna 5510040001 5510041200 R. P. Sharma Institute of Technology (1/2 k.m. East of Khagaul Road) Saguna More, Khagaul Road, Danapur, Patna 8 1004 Patna 4410040001 4410041200 R. P. Sharma Institute of Technology (1/2 k.m. East of Khagaul Road) Saguna More, Khagaul Road, Danapur, Patna 9 1005 Patna 4410050001 4410051200 R.P.S. Public School Venue-01, Patna-Masaudhi Road, New Bypass Road, Bari Pahari, Patna 10 1005 Patna 5510050001 5510051200 R.P.S. Public School Venue-01, Patna-Masaudhi Road, New Bypass Road, Bari Pahari, Patna 11 1006 Patna 4410060001 4410060984 R.P.S. Girls Public School Venue-01, Saguna More, Khagaul Road, St. Karens Secondary School ke samne, Danapur, Patna 12 1006 Patna 5510060001 5510060984 R.P.S. Girls Public School Venue-01, Saguna More, Khagaul Road, St. Karens Secondary School ke samne, Danapur, Patna 13 1007 Patna 4410070001 4410070984 Dr. -

State District Branch Address Centre Ifsc Contact1 Contact2 Contact3 Micr Code
STATE DISTRICT BRANCH ADDRESS CENTRE IFSC CONTACT1 CONTACT2 CONTACT3 MICR_CODE ANDAMAN NO 26. MG ROAD AND ABERDEEN BAZAR , NICOBAR PORT BLAIR -744101 704412829 704412829 ISLAND ANDAMAN PORT BLAIR ,A & N ISLANDS PORT BLAIR IBKL0001498 8 7044128298 8 744259002 UPPER GROUND FLOOR, #6-5-83/1, ANIL ANIL NEW BUS STAND KUMAR KUMAR ANDHRA ROAD, BHUKTAPUR, 897889900 ANIL KUMAR 897889900 PRADESH ADILABAD ADILABAD ADILABAD 504001 ADILABAD IBKL0001090 1 8978899001 1 1ST FLOOR, 14- 309,SREERAM ENCLAVE,RAILWAY FEDDER ROADANANTAPURA ANDHRA NANTAPURANDHRA ANANTAPU 08554- PRADESH ANANTAPUR ANANTAPUR PRADESH R IBKL0000208 270244 D.NO.16-376,MARKET STREET,OPPOSITE CHURCH,DHARMAVA RAM- 091 ANDHRA 515671,ANANTAPUR DHARMAVA 949497979 PRADESH ANANTAPUR DHARMAVARAM DISTRICT RAM IBKL0001795 7 515259202 SRINIVASA SRINIVASA IDBI BANK LTD, 10- RAO RAO 43, BESIDE SURESH MYLAPALL SRINIVASA MYLAPALL MEDICALS, RAILWAY I - RAO I - ANDHRA STATION ROAD, +91967670 MYLAPALLI - +91967670 PRADESH ANANTAPUR GUNTAKAL GUNTAKAL - 515801 GUNTAKAL IBKL0001091 6655 +919676706655 6655 18-1-138, M.F.ROAD, AJACENT TO ING VYSYA BANK, HINDUPUR , ANANTAPUR DIST - 994973715 ANDHRA PIN:515 201 9/98497191 PRADESH ANANTAPUR HINDUPUR ANDHRA PRADESH HINDUPUR IBKL0001162 17 515259102 AGRICULTURE MARKET COMMITTEE, ANANTAPUR ROAD, TADIPATRI, 085582264 ANANTAPUR DIST 40 ANDHRA PIN : 515411 /903226789 PRADESH ANANTAPUR TADIPATRI ANDHRA PRADESH TADPATRI IBKL0001163 2 515259402 BUKARAYASUNDARA M MANDAL,NEAR HP GAS FILLING 91 ANDHRA STATION,ANANTHAP ANANTAPU 929710487 PRADESH ANANTAPUR VADIYAMPETA UR -

TACR: India: Preparing the Bihar State Highways II Project
Technical Assistance Consultant’s Report Project Number: 41629 October 2010 India: Preparing the Bihar State Highways II Project Prepared by Sheladia Associates, Inc. Maryland, USA For Road Construction Department Government of Bihar This consultant’s report does not necessarily reflect the views of ADB or the Government concerned, and ADB and the Government cannot be held liable for its contents. (For project preparatory technical assistance: All the views expressed herein may not be incorporated into the proposed project’s design. TA No. 7198-INDIA: Preparing the Bihar State Highways II Project Final Report TTTAAABBBLLLEEE OOOFFF CCCOOONNNTTTEEENNNTTTSSS 1 INTRODUCTION .............................................................................................................................. 8 1.1 INTRODUCTION .............................................................................................................................. 8 1.2 PROJECT APPRECIATION............................................................................................................. 8 1.2.1 Project Location and Details 9 1.2.2 Road Network of Bihar 11 1.3 PERFORMANCE OF THE STUDY ................................................................................................ 14 1.3.1 Staff Mobilization 14 1.3.2 Work Shop 14 1.4 STRUCTURE OF THE FINAL REPORT ....................................................................................... 14 2 SOCIO ECONOMIC PROFILE OF PROJECT AREA ..................................................................