CONTENTS ISUOG President Contents ● Lawrence D
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Successful Uterovaginal Anastomosis in an Unusual Presentation Of
JSAFOMS Successful Uterovaginal Anastomosis in an Unusual Presentation10.5005/jp-journals-10032-1056 of Congenital Absence of Cervix CASE REPORT Successful Uterovaginal Anastomosis in an Unusual Presentation of Congenital Absence of Cervix 1Nusrat Mahmud, 2Naushaba Tarannum Mahtab, 3TA Chowdhury, 4Anjan Kumar Deb ABSTRACT Source of support: Nil Cervical agenesis or dysgenesis (fragmentation, fibrous cord Conflict of interest: None and obstruction) is an extremely rare congenital anomaly. Conser vative surgical approach to these patients involves uterovaginal anastomosis, cervical canalization and cervical INTRODUCTION reconstruction. In failed conservative surgery, total hysterec- Primary amenorrhea is defined as absence of menstrua- tomy is the treatment of choice. We report what we believe to be the first successful end-to-end uterovaginal anastomosis of tion by the age of 14 years in the absence of secondary an unusual case of congenital cervical agenesis. A 25-year- sex characteristics or the absence of periods by the age of old female presented complaining of primary amenorrhea 16 years regardless of appearance of secondary sex and primary subfertility for the same duration. At laparoscopy, complete separation between the cervix and the body of the charac ters. In our last study, a series of total 108 cases uterus was found and hanging from surrounding supports. of primary amenorrhea were reviewed. It was found Both ovaries and fallopian tubes were anatomically positioned. that 69.4% were due Müllerian dysgenesis, 19.4% due to There was another muscular tissue of 2 cm in diameter at the gonadal dysgenesis, 2.7% male pseudohermaphroditism pouch of Douglas which was attached with lateral pelvic wall 13 by transverse cervical ligament. -

Septate Uterus As Congenital Uterine Anomaly: a Case Report
em & yst Se S xu e a v l i t D c i s u o Reproductive System & Sexual Moghadam et al., Reprod Syst Sex Disord 2014, 3:4 d r o d r e p r e DOI: 10.4172/2161-038X.1000141 s R ISSN: 2161-038X Disorders: Current Research Case Report Open Access Septate Uterus as Congenital Uterine Anomaly: A Case Report Abas Heidari Moghadam1,2, Zahra Jozi1, Shapoor Dahaz1 and DarioushBijan Nejad1* 1Department of Anatomical Sciences, Faculty of Medicine, Ahvaz Jundishapour University of Medical Sciences (AJUMS), Ahvaz, Iran 2Diagnostic Imaging Center of Ahvaz Oil Grand Hospital, Ahvaz, Iran *Correspondingauthor: Darioush Bijan Nejad, Assistant Professor, Department of Anatomical Sciences, Faculty of Medicine, Ahvaz Jundishapour University of Medical Sciences (AJUMS), Ahvaz, Iran, Tel: +98 918 343 4253; Fax: +98 611 333 6380; E-mail:[email protected] Received: June 14, 2014; Accepted: August 01, 2014; Published: August 08, 2014 Copyright: © 2013 Moghadam AH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Abnormal fusion of Mullerian duct in embryonic life is the origin of variety of malformations which may alter the reproductive outcome of the patients. Septate uterus is caused by incomplete resorption of the Mullerian duct during embryogenesis. Here, we report a case of septate uterus that was initially diagnosed by ultrasound scan and confirmed by Magnetic Resonance Imaging (MRI) technique. Keywords: Septate uterus; Mullarian ducts; Ultrasound; MRI Case Report A 29 year old lady came to the imaging diagnostic center of Ahvaz Introduction Oil Grand Hospital. -
Hamilton Radiologu Nuchal Translucencey
PATIENT INFORMATION Advice regarding your 12 week scan Nuchal Translucency HAMILTON RADIOLOGY MEDICAL IMAGING SPECIALISTS YOU’RE IN SAFE HANDS A Few Facts . • The vast majority of babies are born normal. • All women, whatever their age, have a small risk of delivering a baby with physical and/or intellectual impairment. • In some cases the impairment is due to a chromosome abnormality such as Downs Syndrome (Trisomy 21). • The programme will only accept foetuses with a crown rump length between 4.5 and 8.3cm ie within the 11+2 days – 13 weeks 6 days period. Optimal time for this scan is 12–13 weeks. • The scan gives an estimate of the risk for Downs Syndrome. To know for sure whether or not the foetus has a chromosomal abnormality, an invasive test is needed (chorionic villus sampling or amniocentesis). • However, invasive tests carry a small risk of causing miscarriage (1%). • The early scan allows detection of some, but not all, physical defects. A further scan at 19–20 weeks is recommended. Risk for Downs Syndrome The table to the right shows how the chance of having a baby with Downs Syndrome increases with age. The First Trimester Scan At the 12 week scan we confi rm that the foetus is alive and we assess the gestational age by measuring the crown-rump length. We can look for major physical defects, measure nuchal translucency thickness and calculate your baby’s chance of Downs Syndrome based on the scan fi ndings and your age. Occasionally the foetus is not well seen on the abdominal scan and it may be necessary to perform a transvaginal scan. -

Monoamniotic Twins: What Should Be the Optimal Antenatal Management?
Monoamniotic Twins: What Should Be the Optimal Antenatal Management? Ashis K. Sau1, Kate Langford1, Catherine Elliott1, Lin L. Su2, and Darryl J. Maxwell1 1Fetal Medicine Unit, St.Thomas’ Hospital, London, UK 2National University Hospital, Singapore onoamniotic twinning is a rare event with an incidence of London with a high proportion of socially deprived and M1% of all monozygotic twins and associated with a high black, Asian or mixed race peoples. Management protocols fetal morbidity and mortality. Confident early diagnosis is possi- ble, but optimal management is not yet established. This article employed were those of early detection of chorionicity and presents the experience of a single centre in managing all amnionicity, 2-weekly serial ultrasound surveillance and monoamniotic twins diagnosed during 1994–2000. Seven pairs early delivery by elective cesarean section at around 32 of monoamniotic twins were identified for analysis. All were weeks gestation. From 1997, a formal twin ultrasound sur- managed in accord with a unit protocol that involved early diag- veillance clinic was established and first trimester nuchal nosis, serial ultrasound examination and elective early delivery. In four cases, the detection of monoamnionicity was made translucency screening was performed. The same fetal med- during a first trimester nuchal scan. Discordance for structural icine consultant had clinical input into the management of abnormality was found in three cases where the co-twin was all cases. A summary of the cases can be seen in Table 1. normal. Cord entanglement was detected antenatally in four cases. Two pairs of twins died before 20 weeks. One of these Case 1 had early onset twin–twin transfusion syndrome. -

Female Infertility: Ultrasound and Hysterosalpoingography
s z Available online at http://www.journalcra.com INTERNATIONAL JOURNAL OF CURRENT RESEARCH International Journal of Current Research Vol. 11, Issue, 01, pp.745-754, January, 2019 DOI: https://doi.org/10.24941/ijcr.34061.01.2019 ISSN: 0975-833X RESEARCH ARTICLE FEMALE INFERTILITY: ULTRASOUND AND HYSTEROSALPOINGOGRAPHY 1*Dr. Muna Mahmood Daood, 2Dr. Khawla Natheer Hameed Al Tawel and 3 Dr. Noor Al _Huda Abd Jarjees 1Radiologist Specialist, Ibin Al Atheer hospital, Mosul, Iraq 2Lecturer Radiologist Specialist, Institue of radiology, Mosul, Iraq 3Radiologist Specialist, Ibin Al Atheer Hospital, Mosu, Iraq ARTICLE INFO ABSTRACT Article History: The causes of female infertility are multifactorial and necessitate comprehensive evaluation including Received 09th October, 2018 physical examination, hormonal testing, and imaging. Given the associated psychological and Received in revised form th financial stress that imaging can cause, infertility patients benefit from a structured and streamlined 26 November, 2018 evaluation. The goal of such a work up is to evaluate the uterus, endometrium, and fallopian tubes for Accepted 04th December, 2018 anomalies or abnormalities potentially preventing normal conception. Published online 31st January, 2019 Key Words: WHO: World Health Organization, HSG, Hysterosalpingography, US: Ultrasound PID: pelvic Inflammatory Disease, IV: Intravenous. OHSS: Ovarian Hyper Stimulation Syndrome. Copyright © 2019, Muna Mahmood Daood et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Citation: Dr. Muna Mahmood Daood, Dr. Khawla Natheer Hameed Al Tawel and Dr. Noor Al _Huda Abd Jarjees. 2019. “Female infertility: ultrasound and hysterosalpoingography”, International Journal of Current Research, 11, (01), 745-754. -

Screening for Trisomy 21 in Denmark; Evaluation of the Current and Possible Future Strategies
Faculty of Health Sciences University of Copenhagen Screening for trisomy 21 in Denmark; Evaluation of the current and possible future strategies PhD thesis Charlotte Kvist Ekelund Academic supervisors Ann Tabor, professor, DMSc, Department of Fetal Medicine, Rigshospitalet, University of Copenhagen Olav Bjørn Petersen, PhD, consultant, Department of Obstetrics, Aarhus University Hospital Ida Vogel, DMSc, Head of Department of Clinical Genetics, Aarhus University Hospital Evaluation committee Katja Bilardo, Professor, Head Fetal Medicine Unit, Department of Obstetrics & Gynaecology, University Medical Center Groningen, The Netherlands Michael Christiansen, Head of Molecular Diagnostics, Statens Serum Institute, Copenhagen Lone Krebs, DMSc, Associate professor, consultant, Department of Gynecology and Obstetrics, Holbæk Sygehus, University of Copenhagen The PhD defence will take place Friday the 13th of April 2012, Auditorium B, Teilum, Rigshospitalet, Copenhagen. Acknowledgement This thesis was made possible by help from a number of fantastic supervisors and colleagues. First and foremost, I owe my deepest thanks to Professor Ann Tabor. Thank you for sharing your interest and knowledge in first trimester screening with me, for your professional and personal guidance, for always having time and for showing your confidence in me from the very beginning of the project. Your constructive and focused attitude is admirable and to me you have been an extremely inspiring mentor within all aspects of life. I am greatly indebted to Olav Bjørn Petersen, MD, PhD, one of the most enthusiastic and optimistic persons I know. Your positive attitude, support and encouragement have really helped me through the challenging phases of the project. And my sincere thanks to Ida Vogel, MD, DMSc for taking part in the project, for everything you taught me many years ago and for still being there. -

Antenatal Care: Timetable
Antenatal care: timetable NICE issued guidelines on routine care for the healthy pregnant woman in March 2008. They recommend: 10 antenatal visits in the first pregnancy if uncomplicated 7 antenatal visits in subsequent pregnancies if uncomplicated women do not need to be seen by a consultant if the pregnancy is uncomplicated Gestation Purpose of visit 8 - 12 weeks (ideally < 10 Booking visit weeks) general information e.g. diet, alcohol, smoking, folic acid, vitamin D, antenatal classes BP, urine dipstick, check BMI Booking bloods/urine FBC, blood group, rhesus status, red cell alloantibodies, haemoglobinopathies hepatitis B, syphilis, rubella HIV test is offered to all women urine culture to detect asymptomatic bacteriuria 10 - 13 weeks Early scan to confirm dates, exclude multiple pregnancy 11 - 13+6 weeks Down's syndrome screening including nuchal scan 16 weeks Information on the anomaly and the blood results. If Hb < 11 g/dl consider iron Routine care: BP and urine dipstick 18 - 20+6 weeks Anomaly scan 25 weeks (only if primip) Routine care: BP, urine dipstick, symphysis-fundal height (SFH) 28 weeks Routine care: BP, urine dipstick, SFH Second screen for anaemia and atypical red cell alloantibodies. If Hb < 10.5 g/dl consider iron First dose of anti-D prophylaxis to rhesus negative women 31 weeks (only if primip) Routine care as above 34 weeks Routine care as above Second dose of anti-D prophylaxis to rhesus negative women Information on labour and birth plan 36 weeks Routine care as above Check presentation - offer external cephalic version if indicated Information on breast feeding, vitamin K, 'baby-blues' 38 weeks Routine care as above 40 weeks (only if primip) Routine care as above Discussion about options for prolonged pregnancy 41 weeks Routine care as above Discuss labour plans and possibility of induction 1 Prescribing in pregnant patients Very few drugs are known to be completely safe in pregnancy. -

Bad Moon Rising
BAD MOON RISING DB NIELSEN LAURIE STARKEY MICHAEL ANDERLE BRIXBAXTER PUBLISHING CONTENTS Description Chapter 1 Chapter 2 Chapter 3 Chapter 4 Chapter 5 Chapter 6 Chapter 7 Chapter 8 Chapter 9 Chapter 10 Chapter 11 Chapter 12 Chapter 13 Chapter 14 Chapter 15 Chapter 16 Chapter 17 Chapter 18 Chapter 19 Chapter 20 Chapter 21 Chapter 22 Chapter 23 Chapter 24 Chapter 25 Chapter 26 Chapter 27 Chapter 28 Chapter 29 Continue the Saga Author Note About Seven Sons About The Author Copyright DESCRIPTION First rule of Hunting: Never Hunt Alone… Unless you happen to be the trueborn daughter the original vampire and creator of their species. Almost a thousand years have passed since her turning, but her blood rage has only increased, fueling her need to deliver vengeance against the Druids who callously took her beloved mortal sister’s life and cursed hers. Chosen to receive Kayne’s gift of immortality, Aislinn has spent centuries searching for justice, while avoiding the politics and intrigues of the London Coven and its ruthless ruler, Julius. But in a world where blood is power, there are those who will do anything and stop at nothing to possess it. Is Aislinn prepared for what is coming? A Bad Moon is rising… CHAPTER 1 urning into a narrow alley, the darkness grew thicker around Aislinn, and T the cold bit just a touch deeper and sharper with every step. The dull, brown-brick Georgian buildings pressed heavily in, creating only an arrowhead of inky, velvet sky overhead. Most of the factories looked abandoned after the working day was done, windows grimy behind heavy iron bars. -

Management of Reproductive Tract Anomalies
The Journal of Obstetrics and Gynecology of India (May–June 2017) 67(3):162–167 DOI 10.1007/s13224-017-1001-8 INVITED MINI REVIEW Management of Reproductive Tract Anomalies 1 1 Garima Kachhawa • Alka Kriplani Received: 29 March 2017 / Accepted: 21 April 2017 / Published online: 2 May 2017 Ó Federation of Obstetric & Gynecological Societies of India 2017 About the Author Dr. Garima Kachhawa is a consultant Obstetrician and Gynaecologist in Delhi since over 15 years; at present, she is working as faculty at the premiere institute of India, prestigious All India Institute of Medical Sciences, New Delhi. She has several publications in various national and international journals to her credit. She has been awarded various national awards, including Dr. Siuli Rudra Sinha Prize by FOGSI and AV Gandhi award for best research in endocrinology. Her field of interest is endoscopy and reproductive and adolescent endocrinology. She has served as the Joint Secretary of FOGSI in 2016–2017. Abstract Reproductive tract malformations are rare in problems depend on the anatomic distortions, which may general population but are commonly encountered in range from congenital absence of the vagina to complex women with infertility and recurrent pregnancy loss. defects in the lateral and vertical fusion of the Mu¨llerian Obstructive anomalies present around menarche causing duct system. Identification of symptoms and timely diag- extreme pain and adversely affecting the life of the young nosis are an important key to the management of these women. The clinical signs, symptoms and reproductive defects. Although MRI being gold standard in delineating uterine anatomy, recent advances in imaging technology, specifically 3-dimensional ultrasound, achieve accurate Dr. -
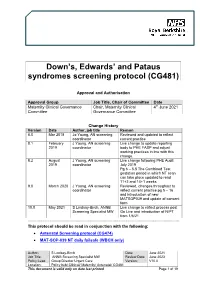
Downs, Edwards & Pataus Screening Protocol (CG481)
Down’s, Edwards’ and Pataus syndromes screening protocol (CG481) Approval and Authorisation Approval Group Job Title, Chair of Committee Date Maternity Clinical Governance Chair, Maternity Clinical 4th June 2021 Committee Governance Committee Change History Version Date Author, job title Reason 8.0 Mar 2018 Jo Young, AN screening Reviewed and updated to reflect coordinator current practice 8.1 February J Young, AN screening Live change to update reporting 2019 coordinator body to PHE FASP and adjust working practices in line with this change. 8.2 August J Young, AN screening Live change following PHE Audit 2019 coordinator July 2019 Pg 6 – 5.5 The Combined Test gestation period in which NT scan can take place updated to read 11+2 and 14+1 weeks 9.0 March 2020 J Young, AN screening Reviewed, changes throughout to coordinator reflect current practice pg 5 – 16 and introduction of new MATSOP039 and update of consent form 10.0 May 2021 S Lindsay-Birch, ANNB Live change to reflect process post Screening Specialist MW Go Live and introduction of NIPT from 1/6/21 ................................................................................................................................................................... This protocol should be read in conjunction with the following: • Antenatal Screening protocol (CG474) • MAT-SOP-039 NT daily failsafe (WBCH only) Author: S Lindsay-Birch Date: June 2021 Job Title: ANNB Screening Specialist MW Review Date: June 2023 Policy Lead: Group Director Urgent Care Version: V10.0 Location: Policy hub/ Clinical/ Maternity/ Antenatal/ CG481 This document is valid only on date last printed Page 1 of 19 Maternity guidelines – Downs, Edwards & Pataus syndromes screening protocol (CG481) June 2021 Contents 1.0 Purpose ............................................................. -

Midwifery & Women's Health Nurse Practitioner Certification Review
MIDWIFERY & WOMEN’S HEALTH NURSE PRACTITIONER CERTIFICATION REVIEW GUIDE Second Edition Edited by Beth M. Kelsey, EdD, WHNP-BC Assistant Professor School of Nursing Ball State University Muncie, Indiana Board of Directors National Association of Nurse Practitioners in Women’s Health (NPWH) Washington, DC 74172_FMXx_ttlpg.indd 1 7/30/10 2:53 PM World Headquarters Jones & Bartlett Learning Jones & Bartlett Learning Jones and Bartlett Learning 40 Tall Pine Drive Canada International Sudbury, MA 01776 6339 Ormindale Way Barb House, Barb Mews 978-443-5000 Mississauga, Ontario L5V 1J2 London W6 7PA [email protected] Canada United Kingdom www.jblearning.com Jones & Bartlett Learning books and products are available through most bookstores and online booksellers. To contact Jones & Bartlett Learning directly, call 800-832-0034, fax 978-443-8000, or visit our website, www.jblearning.com. Substantial discounts on bulk quantities of Jones & Bartlett Learning publications are available to corporations, professional associations, and other qualified organizations. For details and specific discount information, contact the special sales department at Jones & Bartlett Learning via the above contact information or send an email to [email protected]. Copyright © 2011 by Jones & Bartlett Learning, LLC All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without written permission from the copyright owner. The authors, editor, and publisher have made every effort to provide accurate information. However, they are not responsible for errors, omissions, or for any outcomes related to the use of the contents of this book and take no responsibility for the use of the products and procedures described. -

The Effect of Progesterone Use in the First Trimester on Fetal Nuchal Translucency
Original Investigation 29 The effect of progesterone use in the first trimester on fetal nuchal translucency Müberra Namlı Kalem1, Ziya Kalem2, Batuhan Bakırarar3, Ali Ergün1, Timur Gürgan2 1Clinic of Obstetrics and Gynecology, Liv Hospital, Ankara, Turkey 2Gürgan Clinic IVF and Women Health Center, Ankara, Turkey 3Department of Biostatistic, Ankara University School of Medicine, Ankara, Turkey Abstract Objective: To evaluate the possible association between progesterone use in the first trimester of pregnancy and fetal nuchal translucency (NT). Material and Methods: This is an observational case-control study, which was conducted with patients who underwent nuchal scans between March 2015 and February 2016 and consequently delivered live and healthy babies. The study group was composed of assisted reproductive technology pregnancies and used intravaginal progesterone 180 mg/day until gestational week 12. The control group comprised pregnant women who became pregnant spontaneously without using any progesterone preparation in the first trimester. Results: One hundred sixty-four (57.5%) of 285 patients were in the control group and 121 (42.5%) were in the progesterone group. Age, bodyweight, gravidity, and parity number of previous births and abortus, gestational week, crown-rump lengths, free β-human chorionic gonadotropin, pregnancy-associated plasma protein A, and NT values of the progesterone and control groups were recorded and we investigated whether there was a statistically significant difference between the two groups in terms of these parameters; maternal weight was found to be higher in the progesterone group than in the control group and the difference between the groups was statistically significant (p=0.019 and p=0.025).