Chhattisgarh – O
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Naya Raipur Development Plan 20312031
Naya Raipur Development Plan 20312031 Naya Raipur Development Authority NAYA RAIPUR DEVELOPMENT PLAN-2031 PLANNING TEAM NAYA RAIPUR DEVELOPMENT AUTHORITY Shri P. Joy Oommen (I.A.S.) Chairman Shri S.S. Bajaj (I.F.S.) Chief Executive Officer & Director T & CP Shri A.K. Dubey , General Manager (Finance) Shri P.C. Jain, Manager (Finance) Shri S.K. Shrivastava , General Manager (PWD) Shri. S.K.Nag, Manager (PWD) Shri K.P. Bajpai , Building Officer & Town Planner Shri. G.C.Nahata, Deputy Manager ( Land) Shri J.C. Singhal , Dy. G.M. (Public Relation) Shri.V.R. Meshram, Asst. Manager (Land) Shri J.P. Sharma ,Manager (Env) & Dy.M.(R) OFFICERS ASSOCIATED WITH NRDA (EARLIER CADA) AND DIRECTORATE TOWN AND COUNTRY PLANNING ,RAIPUR, IN EARLY STAGES OF PLAN Shri.Vivek Dhand, I.A.S, Chairman Shri.M.K.Gupta, Dy.G.M.(Planning) Shri. Sanjay Shukla, I.F.S, Chief Executive Officer Shri.P.Nihalani, Nazul Officer & D.M (Land) Shri. B.K.Sinha, I.F.S. Chief Executive Officer & Director T & CP Shri. Alok Tiwari, Manager (Environnent) Shri. K.C.Yadav, I.F.S. Chief Executive Officer Shri. Akhilesh Shukla, Data Entry Operator Shri. Anil Tuteja, Chief Executive Officer Shri. Vineet Nair, T & CP OTHER OFFICIAL ASSOCIATED WITH NRDA Shri Rajkumar Mudaliar Shri G.P.Sharma. Shri. B.L.Nishad Shri R.S. Tiwari Shri.Manoj Joshi Shri. K.K.Singaur Shri.Pradeep Thambi Shri S.L. Dhruwanshi Shri.P.D.Yoshen Shri.Mani Ram Dhruw Shri. N.L.Sahu Shri.Navneet Kotwaliwale CITY AND INDUSTRIAL DEVELOPMENT CORPORATION (CIDCO), NAVI MUMBAI Shri N. -

Exploration Strategy for Hot Springs Associated with Gondwana Coalfields in India
Proceedings World Geothermal Congress 2010 Bali, Indonesia, 25-29 April 2010 Exploration Strategy for Hot Springs Associated with Gondwana Coalfields in India P.B. Sarolkar Geological Survey of India, Seminary Hills, Nagpur [email protected] Keywords: Strategy, Gondwana Coalfield, Geothermal, 2. GONDWANA BASINS IN INDIA Hotsprings The Gondwana basins of Peninsular India are restricted to the eastern and central parts of country and are dispersed in ABSTRACT linear belts along major river valleys, including the Damodar The Gondwana coalfields in India are a warehouse of fossil Koel, Son-Mahanadi, Narmada (Satpura area) and Pranhita- fuel energy sources. The coal bearing formations are Godavari basins. The present day basins are likely to be the deposited in deep subsiding basinal structures confined to faulted and eroded remnants of past ones (Dy. Director half-grabens. The Talchir, Barakar, Barren Measures and General, 2007). The Gondwana Coalfields in India are Raniganj formations were deposited in this subsiding basin scattered in the states of West Bengal, Jharkhand, Bihar, with basement rocks separated by faulted margins. The Chhattisgarh, Madhya Pradesh, Maharashtra and Andhra contact of Gondwana rocks with the basement is marked by Pradesh. The important coal fields are shown in Figure 1. faulted margins, while the downthrown side represents a basin of deposition where a huge pile of sediments were All these coalfields have basements with faulted margins, deposited. The cumulative thickness of the sedimentary pile along which Gondwana sedimentation took place. The in the basins varies from 1200 m to 3000 m, depending on Gondwana supergroup of formations hosts coal, coal bed the Gondwana formations deposited. -

Annexure-V State/Circle Wise List of Post Offices Modernised/Upgraded
State/Circle wise list of Post Offices modernised/upgraded for Automatic Teller Machine (ATM) Annexure-V Sl No. State/UT Circle Office Regional Office Divisional Office Name of Operational Post Office ATMs Pin 1 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA PRAKASAM Addanki SO 523201 2 Andhra Pradesh ANDHRA PRADESH KURNOOL KURNOOL Adoni H.O 518301 3 Andhra Pradesh ANDHRA PRADESH VISAKHAPATNAM AMALAPURAM Amalapuram H.O 533201 4 Andhra Pradesh ANDHRA PRADESH KURNOOL ANANTAPUR Anantapur H.O 515001 5 Andhra Pradesh ANDHRA PRADESH Vijayawada Machilipatnam Avanigadda H.O 521121 6 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA TENALI Bapatla H.O 522101 7 Andhra Pradesh ANDHRA PRADESH Vijayawada Bhimavaram Bhimavaram H.O 534201 8 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA VIJAYAWADA Buckinghampet H.O 520002 9 Andhra Pradesh ANDHRA PRADESH KURNOOL TIRUPATI Chandragiri H.O 517101 10 Andhra Pradesh ANDHRA PRADESH Vijayawada Prakasam Chirala H.O 523155 11 Andhra Pradesh ANDHRA PRADESH KURNOOL CHITTOOR Chittoor H.O 517001 12 Andhra Pradesh ANDHRA PRADESH KURNOOL CUDDAPAH Cuddapah H.O 516001 13 Andhra Pradesh ANDHRA PRADESH VISAKHAPATNAM VISAKHAPATNAM Dabagardens S.O 530020 14 Andhra Pradesh ANDHRA PRADESH KURNOOL HINDUPUR Dharmavaram H.O 515671 15 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA ELURU Eluru H.O 534001 16 Andhra Pradesh ANDHRA PRADESH Vijayawada Gudivada Gudivada H.O 521301 17 Andhra Pradesh ANDHRA PRADESH Vijayawada Gudur Gudur H.O 524101 18 Andhra Pradesh ANDHRA PRADESH KURNOOL ANANTAPUR Guntakal H.O 515801 19 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA -
Common Service Center List
CSC Profile Details Report as on 15-07-2015 SNo CSC ID District Name Block Name Village/CSC name Pincode Location VLE Name Address Line 1 Address Line 2 Address Line 3 E-mail Id Contact No 1 CG010100101 Durg Balod Karahibhadar 491227 Karahibhadar LALIT KUMAR SAHU vill post Karahibhadar block dist balod chhattisgarh [email protected] 8827309989 VILL & POST : NIPANI ,TAH : 2 CG010100102 Durg Balod Nipani 491227 Nipani MURLIDHAR C/O RAHUL COMUNICATION BALOD DISTRICT BALOD [email protected] 9424137413 3 CG010100103 Durg Balod Baghmara 491226 Baghmara KESHAL KUMAR SAHU Baghmara BLOCK-BALOD DURG C.G. [email protected] 9406116499 VILL & POST : JAGANNATHPUR ,TAH : 4 CG010100105 Durg Balod JAGANNATHPUR 491226 JAGANNATHPUR HEMANT KUMAR THAKUR JAGANNATHPUR C/O NIKHIL COMPUTER BALOD [email protected] 9479051538 5 CG010100106 Durg Balod Jhalmala 491226 Jhalmala SMT PRITI DESHMUKH VILL & POST : JHALMALA TAH : BALOD DIST:BALOD [email protected] 9406208255 6 CG010100107 Durg Balod LATABOD LATABOD DEKESHWAR PRASAD SAHU LATABOD [email protected] 9301172853 7 CG010100108 Durg Balod Piparchhedi 491226 PIPERCHEDI REKHA SAO Piparchhedi Block: Balod District:Balod [email protected] 9907125793 VILL & POST : JAGANNATHPUR JAGANNATHPUR.CSC@AISEC 8 CG010100109 Durg Balod SANKARAJ 491226 SANKARAJ HEMANT KUMAR THAKUR C/O NIKHIL COMPUTER ,TAH : BALOD DIST: BALOD TCSC.COM 9893483408 9 CG010100110 Durg Balod Bhediya Nawagaon 491226 Bhediya Nawagaon HULSI SAHU VILL & POST : BHEDIYA NAWAGAON BLOCK : BALOD DIST:BALOD [email protected] 9179037807 10 CG010100111 -

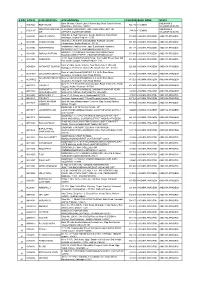
Roll No. G.T. M.O. % G.T. M.O. % G.T. M.O. % 1 2 3 4 5
G.E.M. Utkrist School Raipur C.G. (AG-3) Roll No. EDUCATI EXPERIENC FATHER/HUSBAND CATOR C.G. Total Marit Eligible / REASON OF S.NO. Ragistration No NAME POST DOB ADDRESS CONTACT NO. ON E OF REMARK Exp NAME AGY DOMICILE 12TH GRADUATION PG Marks Not Eligible INELIGIBLITY MEDIUM G.T. M.O. % G.T. M.O. % G.T. M.O. % MONTH 1 2 3 4 5 6 8 9 10 11 12 18 19 20 21 22 23 24 25 26 27 28 28 29 30 31 VILLAGE PALAUD TEKARI C.V. RAMAN PGDCA 1 SAG(03) 0117 150001 TORAN LAL TEJRAM DHIWAR GEN. ASST. GR. 3 05.02.1996 7987840730 YES HINDI 500 374 74.80 204 17.0 46.92 Eligible ABHANPUR RAIPUR (74.00) L.I.G. 989 SEC 6 BEHIND S.B.P. MALECHCHH RAM GURUGHASI DAS 2 SAG(03) 0126 150002 GWALA RAM YADAV OBC ASST. GR. 3 08.07.1982 SCHOOL HOUSING BOARD 9977475716 YES HINDI 450 265 58.89 180 15.0 38.56 Eligible YADAV PGDCA (60) COLONY SADDU RAIPUR AMATALAB RAMKU8ND BAGICHA STENO 25 W MATS UNI 3 SAG(03) 0359 150003 ASST. GR. 3 66.44 132 11.0 37.58 Eligible MANOJ KUMAR SAHU RAMADHAR SAHU OBC 07.02.1984 PARA RAIPUR 7000615875 YES HINDI 450 299 PGDCA (60) EMPIRIAL HEIGHTS HOUSING IGNOU NEW DELHI 4 SAG(03) 0241 150004 YUVRAJ KUMAR SAHU RADHU SAHU OBC ASST. GR. 3 24.04.1991 7000235149 YES HINDI 500 382 76.40 84 7.0 37.56 Eligible BOARD KABIR NAGAR RAIPUR DCA (73) CV RAMAN MUKESH SINGH RANKRISHNA SINGH WARD NO 03 BAIRAGI UNIVERSITY MSC IT 5 SAG(03) 0175 150005 GEN. -

About Chhattisgarh
About Chhattisgarh Map Chhatisgarh state and districts (Stand 2007) At the time of separation from Madhya Pradesh, Chhattisgarh originally had 16 districts. Two new districts: Bijapur and Narayanpur were carved out on May 11, 2007[1] and nine new districts on Jan 1, 2012. The new districts have been created by carving out the existing districts to facilitate more targeted, focused and closer administration. These districts have been named Sukma, Kondagaon, Balod, Bemetara, Baloda Bazar, Gariaband, Mungeli, Surajpur and Balrampur[2] Contents [hide] 1 Background 2 Administrative history 3 Districts of Chhattisgarh 4 References 5 External links Background[edit] A district of an Indian state is an administrative geographical unit, headed by a district magistrate or a deputy commissioner, an officer belonging to the Indian Administrative Service. The district magistrate or the deputy commissioner is assisted by a number of officials belonging to different wings of the administrative services of the state. A superintendent of Police, an officer belonging to Indian Police Service is entrusted with the responsibility of maintaining law and order and related issues. Administrative history Before Indian independence, present-day Chhattisgarh state was divided between the Central Provinces and Berar, a province of British India, and a number of princely states in the north, south, and east, which were part of the Eastern States Agency. The British province encompassed the central portion of the state, and was made up of three districts, Raipur, Bilaspur, and Durg, which made up the Chhattisgarh Division of the Central Provinces. Durg District was created in 1906 out of the eastern portion of Raipur District. -

Afr High Court of Chhattisgarh, Bilaspur
1 AFR HIGH COURT OF CHHATTISGARH, BILASPUR WPC No. 523 of 2016 Smt. Santosh Devi Agrawal W/o Shri Vimal Agrawal, Aged About 60 Years R/o Village Urla, Abhanpur, Tehsil Abhanpur, District Raipur (Chhattisgarh) --- Petitioner Versus 1. Union Of India, Through Secretary Of Ministry Of Road, Transport & Highways Government Of India, New Delhi 2. National Highway Authority Of India, Through Its Project Director, National Highway No. 43 ( N.R.R- 30), Raipur Dhamtari Section ( By- Pass), District Raipur (Chhattisgarh) 3. State Of Chhattisgarh, Through Secretary, Revenue Department, Mantralaya, Mahanadi Bhawan, Capital Complex, Naya Raipur, District Raipur (Chhattisgarh) 4. The Collector, Raipur, District Raipur (Chhattisgarh) 5. Competent Authority-Cum- Sub Divisional Officer, ( Revenue And Land Acquisition Officer), Arang/ Abhanpur, District Raipur (Chhattisgarh) ---- Respondents And WPC No. 570 Of 2016 1. Neeraj Agrawal S/o Shri Vimal Agrawal, Aged About 39 Years R/o Village Urla, Abhanpur, Tehsil Abhanpur, District Raipur, (Chhattisgarh) 2. Nitin Agrawal, S/o Shri Vimal Agrawal, Aged About 35 Years R/o Village Urla, Abhanpur, Tehsil Abhanpur, District Raipur, (Chhattisgarh)- Petitioners Vs 1. Union Of India, Through Secretary Of Ministry Of Road, Transport & Highways Government Of India, New Delhi 2. National Highway Authority Of India, Through Its Project Director, National Highway No. 43 ( N.R.R.- 30), Raipur- Dhamtari Section ( By Pass), District Raipur, (Chhattisgarh) 3. State Of Chhattisgarh, Through Secretary, Revenue Department, Mantralaya, Mahanadi Bhawan, Capital Complex, Naya Raipur, District Raipur, (Chhattisgarh) 4. The Collector, Raipur, District Raipur, (Chhattisgarh) 5. Competent Authority-Cum- Sub Divisional Officer, ( Revenue And Land 2 Acquisition Officer), Arang/ Abhanpur, District Raipur, (Chhattisgarh) ---- Respondents And WPC No. -
S No Atm Id Atm Location Atm Address Pincode Bank
S NO ATM ID ATM LOCATION ATM ADDRESS PINCODE BANK ZONE STATE Bank Of India, Church Lane, Phoenix Bay, Near Carmel School, ANDAMAN & ACE9022 PORT BLAIR 744 101 CHENNAI 1 Ward No.6, Port Blair - 744101 NICOBAR ISLANDS DOLYGUNJ,PORTBL ATR ROAD, PHARGOAN, DOLYGUNJ POST,OPP TO ANDAMAN & CCE8137 744103 CHENNAI 2 AIR AIRPORT, SOUTH ANDAMAN NICOBAR ISLANDS Shop No :2, Near Sai Xerox, Beside Medinova, Rajiv Road, AAX8001 ANANTHAPURA 515 001 ANDHRA PRADESH ANDHRA PRADESH 3 Anathapur, Andhra Pradesh - 5155 Shop No 2, Ammanna Setty Building, Kothavur Junction, ACV8001 CHODAVARAM 531 036 ANDHRA PRADESH ANDHRA PRADESH 4 Chodavaram, Andhra Pradesh - 53136 kiranashop 5 road junction ,opp. Sudarshana mandiram, ACV8002 NARSIPATNAM 531 116 ANDHRA PRADESH ANDHRA PRADESH 5 Narsipatnam 531116 visakhapatnam (dist)-531116 DO.NO 11-183,GOPALA PATNAM, MAIN ROAD NEAR ACV8003 GOPALA PATNAM 530 047 ANDHRA PRADESH ANDHRA PRADESH 6 NOOKALAMMA TEMPLE, VISAKHAPATNAM-530047 4-493, Near Bharat Petroliam Pump, Koti Reddy Street, Near Old ACY8001 CUDDAPPA 516 001 ANDHRA PRADESH ANDHRA PRADESH 7 Bus stand Cudappa, Andhra Pradesh- 5161 Bank of India, Guntur Branch, Door No.5-25-521, Main Rd, AGN9001 KOTHAPET GUNTUR 522 001 ANDHRA PRADESH ANDHRA PRADESH Kothapeta, P.B.No.66, Guntur (P), Dist.Guntur, AP - 522001. 8 Bank of India Branch,DOOR NO. 9-8-64,Sri Ram Nivas, AGW8001 GAJUWAKA BRANCH 530 026 ANDHRA PRADESH ANDHRA PRADESH 9 Gajuwaka, Anakapalle Main Road-530026 GAJUWAKA BRANCH Bank of India Branch,DOOR NO. 9-8-64,Sri Ram Nivas, AGW9002 530 026 ANDHRA PRADESH ANDHRA PRADESH -

State Urban Development Agency Indravati Bhavan, Nava
RFP for Engagement of Consultant for conducting Internal/ Pre-audit, Statutory compliance and Management reporting in all 165 ULBs of Chhattisgarh State. RFP No./9/SUDA/IA/2020/1328/3369 Request for Proposal Dated- 21/12/2020 “RFP for Engagement of Consultant for conducting Internal/ Pre-audit, Statutory compliance and Management reporting in all 165 ULBs of Chhattisgarh State.” State Urban Development Agency Indravati Bhavan, Nava Raipur Atal Nagar, Chhattisgarh Page 1 of 127 RFP for Engagement of Consultant for conducting Internal/ Pre-audit, Statutory compliance and Management reporting in all 165 ULBs of Chhattisgarh State. TABLE OF CONTENTS Disclaimer .............................................................................................................................................................................6 Quick Information Data Sheet ......................................................................................................................................8 Section 2: Background and details of project ...................................................................................................... 10 Section 3: Schedule of RFP and instructions to bidder ................................................................................... 11 Section 4: Process of Bidding ..................................................................................................................................... 32 Section 5 General Terms of Condition .................................................................................................................. -

Brief Industrial Profile of Surguja District
lR;eso t;rs Government of India Ministry of MSME Brief Industrial Profile of Surguja District Carried out by MSME-Development Institute, Raipur (Ministry of MSME, Govt. of India,) Phone :- 0771- 2427719 /2422312 Fax: 0771 - 2422312 e-mail: [email protected] Web- www.msmediraipur.gov.in Contents S. No. Topic Page No. 1. General Characteristics of the District 1 1.1 Location & Geographical Area 1 1.2 Topography 1 1.3 Availability of Minerals. 2 1.4 Forest 2 1.5 Administrative set up 3 2. District at a glance 3 2.1 Existing Status of Industrial Area in the District Surguja 6 3. Industrial Scenario Of Surguja 6 3.1 Industry at a Glance 6 3.2 Year Wise Trend Of Units Registered 7 3.3 Details Of Existing Micro & Small Enterprises & Artisan Units In The 8 District 3.4 Large Scale Industries / Public Sector undertakings 8 3.5 Major Exportable Item 8 3.6 Growth Trend 9 3.7 Vendorisation / Ancillarisation of the Industry 9 3.8 Medium Scale Enterprises 9 3.8.1 List of the units in Surguja & near by Area 9 3.8.2 Major Exportable Item 9 3.9 Service Enterprises 9 3.9.1 Potentials areas for service industry 9 3.10 Potential for new MSMEs 10 4. Existing Clusters of Micro & Small Enterprise 10 4.1 Detail Of Major Clusters 10 4.1.1 Manufacturing Sector 10 4.1.2 Service Sector 10 4.2 Details of Identified cluster 10 5. General issues raised by industry association during the course of 11 meeting 6 Prospects of training Programmes during 2012-13 11 7. -
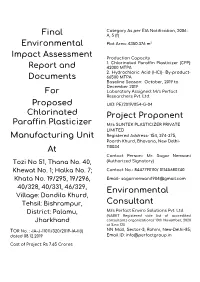
Final Environmental Impact Assessment Report and Documents
Category As per EIA Notification, 2006 : Final A, 5 (f) Plot Area: 4350.376 m2 Environmental Impact Assessment Production Capacity 1. Chlorinated Paraffin Plasticizer (CPP): Report and 42000 MTPA 2. Hydrochloric Acid (HCl)- By-product- Documents 66500 MTPA Baseline Season: October, 2019 to December 2019 For Laboratory Assigned: M/s Perfact Researchers Pvt. Ltd. Proposed UID: PE/2019/054-G-04 Chlorinated Project Proponent Paraffin Plasticizer M/s SUNTEK PLASTICIZER PRIVATE LIMITED Manufacturing Unit Registered Address- 154, 374-375, Poorth Khurd, Bhavana, New Delhi- At 110034 Contact Person- Mr. Sagar Nenwani Tozi No 51, Thana No. 40, (Authorized Signatory) Khewat No. 1; Halka No. 7; Contact No.- 8447790110/ 01145680740 Khata No. 19/295, 19/296, Email- [email protected] 40/328, 40/331, 46/329, Environmental Village: Dandila Khurd, Tehsil: Bishrampur, Consultant District: Palamu, M/s Perfact Enviro Solutions Pvt. Ltd. (NABET Registered vide list of accredited Jharkhand consultants organizations/ 10th November, 2020 at S.no 120 TOR No. : -IA-J-11011/320/2019-IA-II(I) NN Mall, Sector-3, Rohini, New-Delhi-85; dated 08.12.2019 Email ID: [email protected] Cost of Project: Rs 7.65 Crores Suntek Plasticizer Pvt Ltd Works: Khasra No. 19/295, 296, Garhwa Road, Rehla, Dandila Khurd, Near Grasim Industries Ltd. Distt. Palamu, Jharkhand - 822124 SUNTEK CIN: U24290DL2019PTC356272 GROUP GST: 20ABCCS7737C1Z0 E-mail: [email protected] Mob:84477901100 Commitment Letter from Project Proponent Towhomsoever it may concern 1, Nenwani S/o Sagar of Vinod Kumar Nenwai of M/s Suntek Plasticizer Private Limited., Authorized Signatory, for the project"Proposed Chlorinated Paraffin Plasticizer Manufacturing Unit" at Tozi No 51: Thana No. -

Chhattisgarh State Road Sector Development Project (Phase - II)
Resettlement Planning Document Short Resettlement Plan – Abhanpur-Rajim Road Document Stage: Final Project Number: 36005 September 2007 INDIA: Chhattisgarh State Road Sector Development Project (Phase - II) Prepared by Public Works Department, Government of Chhattisgarh for the Asian Development Bank (ADB) The short resettlement plan is a document of the borrower. The views expressed herein do not necessarily represent those of ADB’s Board of Directors, Management, or staff, and may be preliminary in nature. India: Chhattisgarh State Roads Sector Development Project SHORT RESETTLEMENT PLAN Abhanpur-Rajim Road Subproject Public Works Department Government of Chhattisgarh September 2007 Short Resettlement Plan Abhanpur-Rajim Road SHORT RESETTELMENT PLAN TABLE OF CONTENTS List of Abbreviations…………………………………………………….. 2 Executive Summary …………………………………………………….. 3 Section A: Description of the Project……………………………………............. 6 Section B: Objectives of the Short Resettlement Plan………………………….. 6 Section C: Scope of Land Acquisition & Resettlement…………………………. 6 Section D: Socio-economic Profile of the Affected 7 Households………………. Section E: Gender Impacts …………………………………………………………. 8 Section F: Resettlement Principles & Policy Framework………………………. 8 Section G: Stakeholder Participation & Disclosure of the Resettlement Plan 9 Section H: Implementation Arrangements ………….……………………………. 10 Section I: Grievance Redressal …………………………………………………… 11 Section J: Compensation …………………………………………………………… 12 Section K: Budget……………………………………………………………………… 12 Section L: Implementation