Defense Health Programs
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

1 ACADEMIC CURRICULUM VITA Jenny Grace Alderden 10 S 2000 E
ACADEMIC CURRICULUM VITA Jenny Grace Alderden 10 S 2000 E Salt Lake City, UT 84112 [email protected] A. EDUCATION Year Degree Institution (Area of Study / Specialization) 2017 PhD University of Utah College of Nursing 2015 Graduate Certificate University of Utah College of Nursing (Teaching Nursing) 2009 MN University of Washington College of Nursing 2001 BSN University of Illinois at Chicago College of Nursing Licensure / Certification 2003– present Critical Care Nurse Specialist, American Association of Critical Care Nurses 2010– present Critical Care Registered Nurse, American Association of Critical Care Nurses Current Registered Nurse, Idaho: N-38675 Current Advanced practice registered nurse (APRN), Idaho: CNS78 B. EMPLOYMENT / PROFESSIONAL EXPERIENCE Dates Position and Institution 07/2019– present Assistant Professor, University of Utah College of Nursing 09/2009—03/2021 Critical Care Nurse Specialist, St. Luke’s Health System 05/2017–07/2019 Assistant Professor, Boise State University School of Nursing 05/2017–07/2019 Adjunct Assistant Professor, University of Utah College of Nursing 06/2009–present Critical Care Nurse Specialist, St. Luke’s Medical Center 09/2009–01/2011 Clinical Instructor/Adjunct Faculty, Boise State University School of Nursing 05/2007–05/2009 Staff Nurse and Charge Nurse, Critical Care Unit, Harrison Medical Center 2007–2009 Captain, 446 Aeromedical Staging Squadron, United States Air Force Reserve 2006–2007 Helicopter Flight Nurse & Shock Trauma Platoon Head Nurse, U.S. Navy Nurse Corps, Al Anbar, Iraq 2005–2006 Team Member, Fixed-Wing Air Transport, Critical Care Air Transport Team, Okinawa, Japan 2005–2006 Lead Nurse, Training/Education, Naval Hospital, Critical Care Unit, Okinawa, Japan 2005–2006 Charge Nurse and Relief Division Officer, Naval Hospital, Critical Care Unit, Okinawa, Japan 2003–2005 Staff Nurse and Charge Nurse, Naval Medical Center, Critical Care Unit, San Diego, CA 2001–2002 Staff Nurse and Charge Nurse, Naval Medical Center, Medical–Surgical Unit, San Diego, CA 1 C. -
What Nurses Need to Know About Informatics, Social Media and Security! – Page 6
FALL 2017 VOLUME 14 {NO1} EDITION 40 www.ncbon.com NURSING BBULLETINULLETIN What Nurses Need to Know about Informatics, Social Media and Security! – page 6 Publication of the North Carolina State Board of Nursing . FALL. 2017 . BULLETIN. N NC BOARD OF NURSING Nursing Bulletin is the official C publication of the North Table of Carolina Board of Nursing. Office Location CONTENTS 4516 Lake Boone Trail Raleigh, NC 27607 VOLUME 14 {NO 1} EDITION 40 Mailing Address P.O. Box 2129 6 What Nurses Need to Know about Raleigh, NC 27602 Informatics, Social Media, and Security! Telephone (919) 782-3211 Substance Use Disorder: Fax 12 (919) 781-9461 Timely Information for Your Practice Website www.ncbon.com 14 Updated Legislation Provides Benefit to Active Duty Office Hours Military & Spouses 8 a.m. to 5 p.m., Monday through Friday 15 NCBON Staff Nationally & Regionally Recognized Board Chair Pat Campbell The Enhanced Nurse Licensure Compact (eNLC): Chief Executive Officer 16 Julia L. George, RN, MSN, FRE Unlocking Access to Nursing Care Across the Nation Editor David Kalbacker 20 Role of the Registered Nurse in North Carolina— Managing Editor Is It Limited? Elizabeth Langdon Mission Statement 26 NCBON Nurse Gateway—Update Your Information The mission of the North Carolina Board of Nursing is to protect the public by regulating the 27 Tribute to Duke Life Flight Team practice of nursing. 28 CE Opportunities 2018 Advertisements contained herein are not necessarily endorsed by the North Carolina Board of 29 Nomination Form Nursing. The publisher reserves the right to accept or reject advertise- ments for the Nursing Bulletin. -

Responses of Flight Nurses to Catastrophic Events Gene L
Grand Valley State University ScholarWorks@GVSU Masters Theses Graduate Research and Creative Practice 8-2004 Responses of Flight Nurses to Catastrophic Events Gene L. Olsen Grand Valley State University Follow this and additional works at: http://scholarworks.gvsu.edu/theses Part of the Nursing Commons Recommended Citation Olsen, Gene L., "Responses of Flight Nurses to Catastrophic Events" (2004). Masters Theses. 544. http://scholarworks.gvsu.edu/theses/544 This Thesis is brought to you for free and open access by the Graduate Research and Creative Practice at ScholarWorks@GVSU. It has been accepted for inclusion in Masters Theses by an authorized administrator of ScholarWorks@GVSU. For more information, please contact [email protected]. RESPONSES OF FLIGHT NURSES TO CATASTROPHIC EVENTS By Gene L. Olsen A THESIS Submitted to Grand Valley State University In partial fulfillment of the requirements for the Degree of MASTER OF SCIENCE INlSHLfRlSINCI Kirkhof College of Nursing 2004 Thesis Committee Members Linda D. Scott, PhD, RN Andrea C. Bostrom, PhD, APRN, BC Mark J. Greenwood, DO, JD, FACEP Reproduced with permission of the copyright owner. Further reproduction prohibited without permission. RESPONSES ()FI?IJ[C}E[I'lSnjqRJSIïS TO (:ATjtSTltOPHK:ITVEIfrS (jo ie L,. ()lser^ ISSÜST, Itf4,<:3FItFT,]3A/IT-]P August, 2004 Reproduced with permission of the copyright owner. Further reproduction prohibited without permission. ABSTRACT itiüsi'CMstsiiS ()Fi^Li(jïiTr]snLni!SE:s ix) (i/iT^ALST^RjcwpirrczisT/iasri's By GeneL. Olsen, BSN, RN, CFRN, EMT-P The purpose of this study was to examine for the presence of symptoms associated with post-traumatic stress disorder (PTSD) in a sample of flight nurses. -

Nursing in the Military the Profession of Alleviating the Suffering Of
Nursing in the Military The profession of alleviating the suffering of wounded and dying soldiers is as old as warfare itself. Our modern definition of nursing however started with Florence Nightingale on October 21, 1854 during the Crimean War when Nightingale together with she and a contingent of 38 volunteer women were dispatched to Turkey to the aid of wounded British soldiers. Nightingale¶s work later inspired nurses in the American Civil War, during which time, more than 5,000 women served as nurses on the battlefronts. With their contribution, they and their service helped to pave the way for women in professional medicine after the war. The history of women in the military began with the U.S. Army Nurse Corps in 1901. Duty Military nurses perform all the duties of a traditional nurse both during but are times of war and peace. They are also usually entrusted with a wider range of responsibilities than nurses in a civilian environment. In fact, a military nurse can be classified as active duty, reserve, or hired as a civilian employee. The tour of duty for an active or reserve nurse serving in the military requires a long-term commitment. It is common for military nurses to be sent abroad or into service at a combat hospital. Conversely, for civilian employees, the length of time depends on the contract. Ideally, active and reserve duty nurses in the military require experience in critical care, operating room, and trauma. Most are registered nurses with a Bachelor of Science in Nursing degree and enter into service as officers. -

The Value of Evidence-Based Practice in Military Nursing
MILITARY MEDICINE, 185, S2:4, 2020 The Value of Evidence-Based Practice in Military Nursing COL Melissa Hoffman, ANC* ; CAPT Debra Roy, NC, USN† ; Col Deedra Zabokrtsky, USAF, NC‡ ; Col Jennifer Hatzfeld, USAF, NC§ In an unpredictable and complex global environment where lished literature for the best evidence, working with a team our military force must remain globally engaged and adaptive, to synthesize the literature, and implementing a policy or maintaining the readiness of the force is essential. Within practice change based on the evidence. These are not skills the military health system (MHS), the focus is on quality that are unique to the military but are an important part of Downloaded from https://academic.oup.com/milmed/article/185/Supplement_2/4/5835926 by guest on 27 September 2021 health care for our beneficiaries, lower cost, and clinical nursing practice. Nurses with advanced nursing degrees have skills sustainment.1 Those goals support our overall mission an additional 11 competencies that reflect their additional of generating a readily deployable force with a supporting responsibility to provide evidence-based care and the ability medical force ready to deliver health care anywhere and at any to independently evaluate and synthesize evidence.6 time. Evidence-based practice (EBP) provides an important Regardless of educational level, improvement of clinical tool for our health care professionals to maintain a readiness knowledge and processes through EBP is a daily occurrence focus, develop and maintain clinical skills, and provide care across military health care and is led by clinical staff nurses, that is relevant to both the military and civilian health care clinical nurse specialists, nurse scientists, and many other communities. -

JOB DESCRIPTION: Air Crew / Flight Crew Flight Nurse
JOB DESCRIPTION: Air Crew / Flight Crew Flight Nurse A Career as a MedEvac flight nurse Introduction The Flight Nurse functions as a member of the critical care transport team and is responsible for the care of critically ill or injured patients transported by the STAT MedEvac system by supporting and upholding the mission, goals, and objectives at all times. As the Flight Nurse your responsibilities will include patient care incorporating assessment, stabilization, and intervention techniques consistent with standards and protocols approved by the Medical Director. You will also be expected to execute independent judgment in order to deliver appropriate care that is consistent with the clinical protocols, when contact with a medical command physician is not possible. Duties: Responsible for advanced emergency and critical care patient management during air and ground transport of the critically ill or injured patient from the scene or outlying sites to participating secondary and tertiary care institutions. Provides intensive care monitoring, critical care intervention and advanced surgical skill procedures to critically ill and injured patients that include neonates through geriatric age groups. This includes the management of high-risk obstetrical, medical, surgical, respiratory and cardiovascular patients. The specialized training of the Flight Nurse Specialist allows for the provision of care to critically ill and injured patients through the use of ventilatory support, continuous cardiac and hemodynamic monitoring, including intra-aortic balloon and other cardiac assist devices. Airway management and surgical skill intervention includes cricothyroidotomy, needle chest decompression, chest tube insertion, femoral line insertion and/or cut downs and various intubation techniques. Required Qualifications: Licensed to practice professional nursing. -

18-08 Flight Nurse.Xlsx
TRADITIONAL GUARD OFFICER VACANCY ANNOUNCEMENT NEW YORK AIR NATIONAL GUARD ANNOUNCEMENT NO: 18-24 AIR NATIONAL GUARD BASE 109th Airlift Wing DATE: 27-Aug-18 Stratton Air National Guard Base Scotia, New York 12302-9752 CLOSING DATE: 26-Oct-18 UNIT: AFSC: 46F3 139th Aeromedical Evacuation Squadron Stratton ANGB POSITION TITLE: Flight Nurse Scotia, NY 12302-9752 MAX AVAILABLE GRADE: AREA OF CONSIDERATION: Nationwide Maj. / O-4 All applicants may apply who meet the basic qualifications for this New commissioning Opportunity position and who are eligible for membership in the NYANG. SPECIALTY SUMMARY Provides professional medical-surgical nursing care within scope of practice, established standards of care and federal/ state law. Provides comprehensive nursing care for patients during aeromedical evacuation (AE) flights. Coordinates with and makes recommendations to staff agencies concerning clinical care requirements and medical supplies and equipment required for patient care, AE policies, plans and programs. Supports clinical and operational research activities. DUTIES AND RESPONSIBILITIES Member of the AE crew. Functions as the senior medical member to lead both clinical and aircrew operations of the AE crew during intra-theater, and inter-theater flights. Collaborates with appropriate agencies and personnel to ensure appropriate clinical hand- offs, patient care, planning, and mission success. Directs medical specialty teams (i.e. Critical Care Air Transport, Tactical Critical Care Evacuation, Lung) in the inflight environment. Plans and prepares for AE missions. Coordinates clinical operations with operational aircrew during mission pre-planning. Prepares patient positioning plan to facilitate patient enplaning, nursing care, comfort, and safety. Evaluates individual patient's in- flight needs and requests appropriate medications, supplies, and equipment. -

Nursing Leaders in the Military Serving As Faculty
The Voice for Nursing Education Nursing Leaders in the Military Serving as Faculty A Toolkit For Nurse Faculty/Staff Preparing Military Nurse Officers For An Effective Second Career Into Nursing Education September 2018 Authors Myrna L. Armstrong, EdD, RN, ANEF, FAAN Nursing Consultant and Professor Emerita Texas Tech University Health Sciences Center Colonel (R), ANC [email protected] Patricia Allen, EdD, RN, CNE, ANEF, FAAN Professor and Director, Nursing Education Track Distinguished University Professor Texas Tech University Health Sciences Center [email protected] Donna Lake, PhD, RN, NEA-BC Clinical Associate Professor East Carolina University College of Nursing Colonel, USAF NC (R) [email protected] The authors of this toolkit, titled A Toolkit for Nurse Faculty Preparing Military Nurse Officers for an Effective Second Career in Nursing Education, extend permission to the National League for Nursing (NLN) to post it on the NLN website. The authors also acknowledge this document will be open access; the intent is for users to adapt the toolkit for use in a variety of academ- ic and practice institutions. Users are asked to include in the citation of the source that the document was retrieved on the NLN website. This publication is dedicated to all of the men and women who have served in the United States military providing care to America’s sons and daughters. Toolkit Objectives Upon completion of this toolkit, the nurse educator will be able to: › Describe military nurse competencies transferable to the nurse educator role. › Recognize cultural differences between the Military Nurse Officer (MNO) and the academic nurse educator. -

The Challenges and Psychological Impact of Delivering Nursing Care Within a War Zone
The Challenges and Psychological Impact of Delivering Nursing Care within a War Zone Item Type Article Authors Finnegan, Alan; Lauder, William; McKenna, Hugh Citation Finnegan, A., Lauder, W., & McKenna, H. (2016). The challenges and psychological impact of delivering nursing care within a war zone. Nursing Outlook, DOI 10.1016/j.outlook.2016.05.005 Publisher Elsevier Journal Nursing Outlook Download date 24/09/2021 15:01:39 Link to Item http://hdl.handle.net/10034/617614 The Challenges and Psychological Impact of Delivering Nursing Care within a War Zone Abstract Background. Between 2001 and 2014, British military nurses served in Afghanistan caring for both Service personnel and local nationals of all ages. However, there have been few research studies assessing the psychological impact of delivering nursing care in a War Zone hospital. Purpose. To explore the challenges and psychological stressors facing military nurses in undertaking their operational role. Method. A Constructivist Grounded Theory was utilised. Semi-structured interviews were conducted with 18 British Armed Forces nurses at Camp Bastion Hospital, Afghanistan, in June – July 2013. Discussion. Military nurses faced prolonged periods of caring for seriously injured poly trauma casualties of all ages, and there were associated distressing psychological effects and prolonged periods of adjustment on returning home. Caring for children was a particular concern. The factors that caused stress, both on deployment and returning home, along with measures to address these issues such as time for rest and exercise, can change rapidly in response to the dynamic flux in clinical intensity common within the deployable environment. Conclusion. Clinical training, a good command structure, the requirement for rest, recuperation, exercise and diet were important in reducing psychological stress within a War Zone. -

Countries Where Anesthesia Is Administered by Nurses Lt Col MAURA S
Countries where anesthesia is administered by nurses Lt Col MAURA S. McAULIFFE, CRNA, PhD Rockville, Maryland BEVERLEY HENRY, RN, PhD, FAAN Chicago, Illinois Introduction Nurse anesthetists make significant In many countries anesthesia is administered pri- contributionsto healthcare worldwide. A marily by nurses. Yet few, including many in nurs- little known fact is that, in many countries ing, are aware of the major contribution to health of the world, nearly all anesthesiais that nurses, functioning as anesthetists, make. Even provided by nurses. This international some history books overlook nurses in anesthesia, survey, in five languages, was done to provide and little has been written about the education, information about nurse anesthesiacare practice, and legal regulation of nurse anesthetists delivered in countries in the regions of the worldwide. world designated by the World Health Two significant occurrences provided the im- Organization. petus for this study. First, in 1978, the World PhaseI, reported here, of a three-phase Health Organization (WHO) proclaimed its goal project, determined that nurses administer of health for all by the year 2000, in which nurses anesthesia in at least 107 of the world's nearly are viewed as major contributors and anesthesia as 200 countries. They administeranesthesia in an essential service. Second, the idea for an inter- developed, developing, and least developed national professional organization took root countries, as well as in all regions of the through which nurse anesthetists from all coun- world. A goal of disseminatingdata in this tries could collaborate, culminating, in 1989, in article is to further validate these 1992-1994 the formation of the International Federation of study findings. -

Air Ambulance Nurses As Expert Supplement to Local Emergency Services Torben Wisborg, MD, Phd,1-3 and Bjørn Bjerkan, Bsc, CRNA2,3
ORIGINAL RESEARCH Air Ambulance Nurses as Expert Supplement to Local Emergency Services Torben Wisborg, MD, PhD,1-3 and Bjørn Bjerkan, BSc, CRNA2,3 Abstract 2 Objective: Flight nurses in the Norwegian National Air well-developed national air ambulance service. The Ambulance Service are specialist nurse anesthetists or intensive Norwegian National Air Ambulance Service has ambulance care nursing specialists. For air ambulance bases far from hospitals, helicopters and dedicated ambulance fixed-wing aircraft dis- tributed over the country, with most fixed-wing aircraft in the these nurses present otherwise unavailable competencies. This northern part where the population density is low. The infra- study reports a 6-year experience with flight nurse participation in structure in Northern Norway was developed through the local emergencies beyond the transportation phase. 1970s by establishing a number of short runway air fields to Methods: The fixed-wing air ambulance base in Alta, Northern enable communications, including patient transport, which Norway (20,000 inhabitants), with 2 aircraft and 2 on-call teams previously was performed by boats and seaplanes. is 150 km by road from the nearest hospital. We did a prospec- In the northernmost part of Norway (Finnmark County), the tive registration of all emergency nonflight missions near the community of Alta is the most inhabited area with approximately air ambulance base from January 1, 2005, to December 31, 20,000 residents (Fig. 1). This population is 150 km by road 2010. from the nearest hospital. The primary health care service in Alta Results: The 217 completed missions corresponded to 3 missions has developed a unique model of a decentralized, advanced per month, half during daytime. -
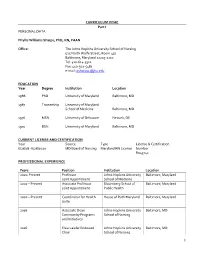
CURRICULUM VITAE Part I PERSONAL DATA Phyllis Williams
CURRICULUM VITAE Part I PERSONAL DATA Phyllis Williams Sharps, PhD, RN, FAAN Office: The Johns Hopkins University School of Nursing 525 North Wolfe Street, Room 437 Baltimore, Maryland 21205-2110 Tel: 410-614-5312 Fax: 410-502-5481 e-mail: [email protected] EDUCATION Year Degree Institution Location 1988 PhD University of Maryland Baltimore, MD 1987 Traineeship University of Maryland School of Medicine Baltimore, MD 1976 MSN University of Delaware Newark, DE 1970 BSN University of Maryland Baltimore, MD CURRENT LICENSE AND CERTIFICATION Year Source Type License & Certification 6/28/18 -6/28/2020 MD Board of Nursing Maryland RN License Number R043742 PROFESSIONAL EXPERIENCE Years Position Institution Location 2020-Present Professor Johns Hopkins University Baltimore, Maryland Joint Appointment School of Medicine 2002 – Present Associate Professor Bloomberg School of Baltimore, Maryland Joint Appointment Public Health 2002 – Present Coordinator for Health House of Ruth Maryland Baltimore, Maryland Suite 2016 Associate Dean Johns Hopkins University Baltimore, MD Community Programs School of Nursing and Initiatives 2016 Elsie Lawler Endowed Johns Hopkins University Baltimore, MD Chair School of Nursing 1 2011 Associate Dean Johns Hopkins University Baltimore, MD Community and Global School of Nursing Programs 2007- 2011 Department Chair Johns Hopkins University Baltimore, MD School of Nursing 2007 Professor Johns Hopkins University Baltimore, MD School of Nursing 2001 – 2007 Associate Professor Johns Hopkins University Baltimore, Maryland School of Nursing 2002-2006 Director, Master’s Johns Hopkins University Baltimore, MD Program School of Nursing 2000 – 2001 Director George Washington Washington, D.C. University, School of Public Health & Health Services 1998 – 2000 Associate Research George Washington Washington, D.C.