Mycology Summary -1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Uncommon Fungi and Related Species
Uncommon Fungi and 268 Related Species Duane R. Hospenthal SHORT VIEW SUMMARY SCEDOSPORIUM APIOSPERMUM Diagnosis FUSARIUMM SPP. (PSEUDALLESCHERIA BOYDIII) SPECIES Diagnosis is made by culture recovery from the } Definition COMPLEX infected site. } Can cause disseminated infection in } Because L. prolificanss may colonize airways, Definition immunocompromised patients. sputum cultures may not reflect infection. } Infection of the lungs, bones and joints, or } Common cause of keratitis and other eye central nervous system (CNS); may be Therapy infections in contact lens wearers and disseminated. } No effective therapy. Consider voriconazole following trauma. } Also causes mycetoma (see Chapter 261). with amphotericin B. } Skin and soft tissue infection after trauma, onychomycosis; can cause mycetoma. Epidemiology DARK-WALLED FUNGI (BIPOLARIS, } Typically occurs in the immunocompromised or EXOPHIALA, EXSEROHILUM, Epidemiology following trauma. PHIALOPHORA, OCHROCONIS, } Common plant pathogens; found in soil and } CNS infection in immunocompetent persons CURVULARIA, OTHERS) organic debris. after near drowning. Have been recovered in hospital water supplies. Definition } } Organism can be found in soil and fresh water, } This infection involves fungi that have melanin Microbiology especially stagnant or polluted. in their cell walls and may appear dark walled } The most common species infecting humans Microbiology in tissue. belong to one of three species complexes: } Scedosporium apiospermum, Scedosporium } Infection is often termed Fusarium solani, Fusarium oxysporum, or boydiii (formerly Pseudallescheria boydiii), and “phaeohyphomycosis” and typically presents Fusarium fujikuroi, although the number of Scedosporium aurantiacumm are the most as localized skin and soft tissue infections, species identified as causing infection is common species infecting humans. CNS infections, or allergic sinusitis. increasing as molecular methods of } Identification is typically made by DNA } Dark-walled fungi that cause identification have supplanted morphology. -

10-ELS-OXF Kurtzman1610423 CH002 7..20
Part II Importance of Yeasts Kurtzman 978-0-444-52149-1 00002 Kurtzman 978-0-444-52149-1 00002 Chapter 2 c0002 Yeasts Pathogenic to Humans Chester R. Cooper, Jr. regularly encounter the organisms described below. In fact, many s0010 1. INTRODUCTION TO THE MEDICALLY medical mycologists spend entire careers without direct clinical expo- IMPORTANT YEASTS sure to many of these fungi. Rather, the purpose of this review is to enlighten the non-medical mycologist as to the diversity of yeast and p0010 Prior to global emergence of the human immunodeficiency virus mold species regularly associated with human and animal disease (HIV), which is the causative agent of acquired immunodeficiency that also, at least in part, present a unicellular mode of growth in vivo. syndrome (AIDS), approximately 200 fungal pathogens were recog- The following descriptions present a concise overview of the key p0025 nized from among the more than 100,000 then-known fungal spe- biological and clinical features of these fungi. Where appropriate, refer- cies (Kwon-Chung and Bennett 1992, Rippon 1988). About 50 of ences to recent reviews of particular disease agents and their patholo- these species were regularly associated with fungal disease (myco- gies are provided. For a global perspective of fungal diseases, including sis). Since then, there has been a concurrent dramatic increase in in-depth clinical discussions of specific pathologies, diagnoses, and both the number of known fungal species and the incidence of treatments, the reader is referred to several outstanding and recently mycoses that they cause. Moreover, the spectrum of pathogenic fungi published texts (Anaissie et al. -

A Case Study on Subcutaneous Zygomycosis with Ulcer
Int.J.Curr.Microbiol.App.Sci (2013) 2(10): 448-451 ISSN: 2319-7706 Volume 2 Number 10 (2013) pp. 448-451 http://www.ijcmas.com Case report A Case Study on Subcutaneous zygomycosis with ulcer P.Hema Prakash Kumari1, M. SrinivasaRao2, S. Subbarayudu3, Y. Saritha4 and Amrutha Kar5 1,3,4,5Department of Microbiology ASRAM Medical College Eluru, A.P Pin 534004, India 2Department of Pediatrics ASRAM Medical College Eluru, A.P Pin 534004, India *Corresponding author A B S T R A C T K e y w o r d s Subcutaneous mycosis due to Basidiobolus ranarum is endemic in south Subcutaneous India. We hereby report a case of subcutaneous zygomycosis in a 6 months phycomycosis; old female child who presented with a painless, non-tender swelling Basidiobolus progressed to ulcer on the thigh. ranarum; Introduction Routine investigations were normal and x A 6 month female child was brought to ray left thigh showed soft tissue swelling. pediatric department with h/o gradually Tests for HIV negative, swabs were sent increasing painless ulcerated swelling over for bacterial and fungal culture. Bacterial the left thigh. There was history of insect culture was sterile and a 10% potassium bite 4 months ago. The swelling was hydroxide wet mount revealed broad, gradually increasing since then and irregular aseptate hyphae. Growth on progressed to ulcer formation covered by Sabouraud s dextrose agar after 3 days of eschar. incubation at 25 °C showed creamy brown, centrally heaped up, radially folded No discharge was observed. On cutaneous colonies with satellite colonies on the examination there was a single firm, well periphery (Figure 2). -

Boards' Fodder
boards’ fodder Medical Mycology By Adriana Schmidt, MD, and Natalie M. Curcio, MD, MPH. (Updated July 2015*) SUPERFICIAL ORGANISM CLINICAL HISTO/KOH TREATMENT MYCOSES* Pityriasis Malessezia furfur Hypo- or hyper-pigmented Spaghetti & meatballs: Antifungal shampoos and/or versicolor macules short hyphae + yeast PO therapy Tinea nigra Hortaea werneckii (formerly Brown-black non-scaly Branching septate hyphae Topical imidazoles or palmaris Phaeoannellomyces werneckii) macules + budding yeast allylamines Black piedra Piedraia hortae Hard firm black Dark hyphae around concretions acrospores Cut hair off, PO terbinafine, White piedra Trichosporon ovoides or inkin Soft loose white Blastoconidia, imidazoles, or triazoles (formely beigelii) concretions arthroconidia Fluorescent small Microsporum Canis KOH: spores on outside spore ectothrix: M. audouinii of the hair shaft; “Cats And Dogs M. distortum Wood’s lamp --> yellow Sometimes Fight T. schoenleinii fluorescence & Growl” M. ferrugineum+/- gypseum Large spore Trichophyton spp. (T. tonsurans in North America; T. violaceum in KOH: spores within hair Topical antifungals; PO endothrix Europe, Asia, parts of Africa). shaft antifungals for T. manuum, Tinea corporis T. rubrum > T. mentag. Majocchi’s granuloma: T. rubrum capitis, unguium T. pedis Moccasin: T. rubrum, E. floccosum. Interdigital/vesicular: T. mentag T. unguium Distal lateral, proximal and proximal white subungual: T. rubrum. White superficial: T. mentag. HIV: T. rubrum SUBQ MYCOSES** ORGANISM TRANSMISSION CLINICAL HISTO/KOH TREATMENT -

Gastrointestinal Basidiobolomycosis, a Rare and Under-Diagnosed Fungal Infection in Immunocompetent Hosts: a Review Article
IJMS Vol 40, No 2, March 2015 Review Article Gastrointestinal Basidiobolomycosis, a Rare and Under-diagnosed Fungal Infection in Immunocompetent Hosts: A Review Article Bita Geramizadeh1,2, MD; Mina Abstract 2 2 Heidari , MD; Golsa Shekarkhar , MD Gastrointestinal Basidiobolomycosis (GIB) is an unusual, rare, but emerging fungal infection in the stomach, small intestine, colon, and liver. It has been rarely reported in the English literature and most of the reported cases have been from US, Saudi Arabia, Kuwait, and Iran. In the last five years, 17 cases have been reported from one or two provinces in Iran, and it seems that it has been undiagnosed or probably unnoticed in other parts of the country. This article has Continuous In this review, we explored the English literature from 1964 Medical Education (CME) through 2013 via PubMed, Google, and Google scholar using the credit for Iranian physicians following search keywords: and paramedics. They may 1) Basidiobolomycosis earn CME credit by reading 2) Basidiobolus ranarum this article and answering the 3) Gastrointestinal Basidiobolomycosis questions on page 190. In this review, we attempted to collect all clinical, pathological, and radiological findings of the presenting patients; complemented with previous experiences regarding the treatment and prognosis of the GIB. Since 1964, only 71 cases have been reported, which will be fully described in terms of clinical presentations, methods of diagnosis and treatment as well as prognosis and follow up. Please cite this article as: Geramizadeh B, Heidari M, Shekarkhar G. Gastrointestinal Basidiobolomycosis, a Rare and Under-diagnosed Fungal Infection in Immunocompetent Hosts: A Review Article. Iran J Med Sci. -

Case Report of Subcutaneous Entomophthoromycosis with Retroperitoneal Invasion
RELATO DE CASO/CASE REPORT Revista da Sociedade Brasileira de Medicina Tropical 38(4):348-350, jul-ago, 2005 Case report of subcutaneous entomophthoromycosis with retroperitoneal invasion Relato de caso de entomoftoromicose subcutânea com invasão retroperitoneal Leonora Maciel de Souza Vianna1, 2, Marcus Vinícius Guimarães de Lacerda1 and Mário Augusto Pinto de Moraes1 ABSTRACT The authors describe a case of entomophthoromycosis in a previously healthy patient, who presented with an abscess in the right buttock. After surgical drainage it evolved into a retroperitoneal tumor. The patient improved clinically after resection of the mass and ketoconazole treatment. The histopathological analysis showed the Splendore-Hoeppli phenomenon, suggesting Basidiobolus ranarum infection, a zygomycosis generally restricted to the subcutaneous tissue, with rare gastrointestinal involvement. Key-words: Basidiobolus ranarum. Zygomycosis. Entomophthorales. Clinical features. Histopathology. Splendore-Hoeppli phenomenon. RESUMO Os autores descrevem um caso de entomoftoromicose em paciente previamente saudável, que apresentou abscesso em nádega direita, evoluindo, após drenagem cirúrgica, para tumoração retroperitoneal. Após ressecção da massa, o paciente obteve melhora clínica, em uso de cetoconazol. A análise histopatológica evidenciou fenômeno de Splendore-Hoeppli, sugerindo infecção por Basidiobolus ranarum, uma zigomicose geralmente restrita ao tecido subcutâneo, com raro comprometimento gastrintestinal. Palavras-chaves: Basidiobolus ranarum. Zigomicose. -
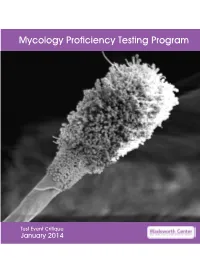
Mycology Proficiency Testing Program
Mycology Proficiency Testing Program Test Event Critique January 2014 Table of Contents Mycology Laboratory 2 Mycology Proficiency Testing Program 3 Test Specimens & Grading Policy 5 Test Analyte Master Lists 7 Performance Summary 11 Commercial Device Usage Statistics 13 Mold Descriptions 14 M-1 Stachybotrys chartarum 14 M-2 Aspergillus clavatus 18 M-3 Microsporum gypseum 22 M-4 Scopulariopsis species 26 M-5 Sporothrix schenckii species complex 30 Yeast Descriptions 34 Y-1 Cryptococcus uniguttulatus 34 Y-2 Saccharomyces cerevisiae 37 Y-3 Candida dubliniensis 40 Y-4 Candida lipolytica 43 Y-5 Cryptococcus laurentii 46 Direct Detection - Cryptococcal Antigen 49 Antifungal Susceptibility Testing - Yeast 52 Antifungal Susceptibility Testing - Mold (Educational) 54 1 Mycology Laboratory Mycology Laboratory at the Wadsworth Center, New York State Department of Health (NYSDOH) is a reference diagnostic laboratory for the fungal diseases. The laboratory services include testing for the dimorphic pathogenic fungi, unusual molds and yeasts pathogens, antifungal susceptibility testing including tests with research protocols, molecular tests including rapid identification and strain typing, outbreak and pseudo-outbreak investigations, laboratory contamination and accident investigations and related environmental surveys. The Fungal Culture Collection of the Mycology Laboratory is an important resource for high quality cultures used in the proficiency-testing program and for the in-house development and standardization of new diagnostic tests. Mycology Proficiency Testing Program provides technical expertise to NYSDOH Clinical Laboratory Evaluation Program (CLEP). The program is responsible for conducting the Clinical Laboratory Improvement Amendments (CLIA)-compliant Proficiency Testing (Mycology) for clinical laboratories in New York State. All analytes for these test events are prepared and standardized internally. -

Phylogeny of Chrysosporia Infecting Reptiles: Proposal of the New Family Nannizziopsiaceae and Five New Species
CORE Metadata, citation and similar papers at core.ac.uk Provided byPersoonia Diposit Digital 31, de Documents2013: 86–100 de la UAB www.ingentaconnect.com/content/nhn/pimj RESEARCH ARTICLE http://dx.doi.org/10.3767/003158513X669698 Phylogeny of chrysosporia infecting reptiles: proposal of the new family Nannizziopsiaceae and five new species A.M. Stchigel1, D.A. Sutton2, J.F. Cano-Lira1, F.J. Cabañes3, L. Abarca3, K. Tintelnot4, B.L. Wickes5, D. García1, J. Guarro1 Key words Abstract We have performed a phenotypic and phylogenetic study of a set of fungi, mostly of veterinary origin, morphologically similar to the Chrysosporium asexual morph of Nannizziopsis vriesii (Onygenales, Eurotiomycetidae, animal infections Eurotiomycetes, Ascomycota). The analysis of sequences of the D1-D2 domains of the 28S rDNA, including rep- ascomycetes resentatives of the different families of the Onygenales, revealed that N. vriesii and relatives form a distinct lineage Chrysosporium within that order, which is proposed as the new family Nannizziopsiaceae. The members of this family show the mycoses particular characteristic of causing skin infections in reptiles and producing hyaline, thin- and smooth-walled, small, Nannizziopsiaceae mostly sessile 1-celled conidia and colonies with a pungent skunk-like odour. The phenotypic and multigene study Nannizziopsis results, based on ribosomal ITS region, actin and β-tubulin sequences, demonstrated that some of the fungi included Onygenales in this study were different from the known species of Nannizziopsis and Chrysosporium and are described here as reptiles new. They are N. chlamydospora, N. draconii, N. arthrosporioides, N. pluriseptata and Chrysosporium longisporum. Nannizziopsis chlamydospora is distinguished by producing chlamydospores and by its ability to grow at 5 °C. -

A New Duplex PCR-Assay for the Detection and Identification of Paracoccidioides Species
Journal of Fungi Article A New Duplex PCR-Assay for the Detection and Identification of Paracoccidioides Species Breno Gonçalves Pinheiro 1 , Ana Paula Pôssa 1,2, Paula Portella Della Terra 1,2 , Jamile Ambrósio de Carvalho 1, Giannina Ricci 3, Angela Satie Nishikaku 3 , Rosane Christine Hahn 4,5, Zoilo Pires de Camargo 1,2 and Anderson Messias Rodrigues 1,2,* 1 Laboratory of Emerging Fungal Pathogens, Department of Microbiology, Immunology, and Parasitology, Discipline of Cellular Biology, Federal University of São Paulo (UNIFESP), São Paulo 04023062, Brazil; [email protected] (B.G.P.); [email protected] (A.P.P.); [email protected] (P.P.D.T.); [email protected] (J.A.d.C.); [email protected] (Z.P.d.C.) 2 Department of Medicine, Discipline of infectious Diseases, Federal University of São Paulo (UNIFESP), São Paulo 04023062, Brazil 3 Centro de Diagnóstico e Pesquisa em Biologia Molecular Dr. Ivo Ricci, São Paulo 13561020, Brazil; [email protected] (G.R.); [email protected] (A.S.N.) 4 Laboratory of Mycology/Research, Faculty of Medicine, Federal University of Mato Grosso, Cuiabá 78060900, Brazil; [email protected] 5 Júlio Muller University Hospital, Federal University of Mato Grosso, Cuiabá 78048902, Brazil * Correspondence: [email protected]; Tel.: +55-1155764551 (ext. 1540) Abstract: Paracoccidioidomycosis (PCM) is a life-threatening systemic fungal infection caused Citation: Pinheiro, B.G.; Pôssa, A.P.; by members of the Paracoccidioides brasiliensis complex and P. lutzii. Routine diagnoses of PCM Della Terra, P.P.; de Carvalho, J.A.; down to the species level using classical mycological approaches are unspecific due to overlapping Ricci, G.; Nishikaku, A.S.; Hahn, R.C.; phenotypes. -

Differences in Fungi Present in Induced Sputum Samples from Asthma
van Woerden et al. BMC Infectious Diseases 2013, 13:69 http://www.biomedcentral.com/1471-2334/13/69 RESEARCH ARTICLE Open Access Differences in fungi present in induced sputum samples from asthma patients and non-atopic controls: a community based case control study Hugo Cornelis van Woerden1*, Clive Gregory1*, Richard Brown2, Julian Roberto Marchesi2, Bastiaan Hoogendoorn1 and Ian Price Matthews1 Abstract Background: There is emerging evidence for the presence of an extensive microbiota in human lungs. It is not known whether variations in the prevalence of species of microbiota in the lungs may have aetiological significance in respiratory conditions such as asthma. The aim of the study was to undertake semi-quantitative analysis of the differences in fungal species in pooled sputum samples from asthma patients and controls. Methods: Induced sputum samples were collected in a case control study of asthma patients and control subjects drawn from the community in Wandsworth, London. Samples from both groups were pooled and then tested for eukaryotes. DNA was amplified using standard PCR techniques, followed by pyrosequencing and comparison of reads to databases of known sequences to determine in a semi-quantitative way the percentage of DNA from known species in each of the two pooled samples. Results: A total of 136 fungal species were identified in the induced sputum samples, with 90 species more common in asthma patients and 46 species more common in control subjects. Psathyrella candolleana, Malassezia pachydermatis, Termitomyces clypeatus and Grifola sordulenta showed a higher percentage of reads in the sputum of asthma patients and Eremothecium sinecaudum, Systenostrema alba, Cladosporium cladosporioides and Vanderwaltozyma polyspora showed a higher percentage of reads in the sputum of control subjects. -

Basidiobolus Omanensis Sp. Nov. Causing Angioinvasive Abdominal Basidiobolomycosis
Journal of Fungi Article Basidiobolus omanensis sp. nov. Causing Angioinvasive Abdominal Basidiobolomycosis Abdullah M. S. Al-Hatmi 1,2,3,* , Abdullah Balkhair 4, Ibrahim Al-Busaidi 4 , Marcelo Sandoval-Denis 5, Saif Al-Housni 1, Hashim Ba Taher 4, Asmaa Hamdan Al Shehhi 6, Sameer Raniga 7 , Maha Al Shaibi 8, Turkiya Al Siyabi 9, Jacques F. Meis 3,10 , G. Sybren de Hoog 3 , Ahmed Al-Rawahi 1, Zakariya Al Muharrmi 9, Ahmed Al-Harrasi 1 and Badriya Al Adawi 9,* 1 Natural & Medical Sciences Research Center, University of Nizwa, Nizwa 616, Oman; [email protected] (S.A.-H.); [email protected] (A.A.-R.); [email protected] (A.A.-H.) 2 Department of Biological Sciences & Chemistry, College of Arts and Sciences, University of Nizwa, Nizwa 616, Oman 3 Centre of Expertise in Mycology, Radboud University Medical Centre/Canisius Wilhelmina Hospital, 6532 SZ Nijmegen, The Netherlands; [email protected] (J.F.M.); [email protected] (G.S.d.H.) 4 Infectious Diseases Unit, Department of Medicine, Sultan Qaboos University Hospital, Muscat 123, Oman; [email protected] (A.B.); [email protected] (I.A.-B.); [email protected] (H.B.T.) 5 Westerdijk Fungal Biodiversity Institute, 3584 CT Utrecht, The Netherlands; [email protected] 6 Department of Pathology, Sultan Qaboos University Hospital, Muscat 123, Oman; [email protected] 7 Department of Radiology and Molecular Imaging, Sultan Qaboos University Hospital, Muscat 123, Oman; [email protected] 8 Department of Surgery, Sultan Qaboos University Hospital, Muscat -

In Vitro and in Situ ACTIVATION of the COMPLEMENT SYSTEM by the FUNGUS Lacazia Loboi
Rev. Inst. Med. trop. S. Paulo 49(2):97-101, March-April, 2007 In vitro AND in situ ACTIVATION OF THE COMPLEMENT SYSTEM BY THE FUNGUS Lacazia loboi Fátima Regina VILANI-MORENO(1), Érika MOZER(2), Ana Márcia Guedes de SENE(2), Margarete de Oliveira FERASÇOLI(2), Tânia Cristina PEREIRA(2), Márcia Garcia MIRAS(2), Gláucia Heloísa de Paula SOUZA(3) & Andréa de Faria Fernandes BELONE(3) SUMMARY Since there are no studies evaluating the participation of the complement system (CS) in Jorge Lobo’s disease and its activity on the fungus Lacazia loboi, we carried out the present investigation. Fungal cells with a viability index of 48% were obtained from the footpads of BALB/c mice and incubated with a pool of inactivated serum from patients with the mycosis or with sterile saline for 30 min at 37 oC. Next, the tubes were incubated for 2 h with a pool of noninactivated AB+ serum, inactivated serum, serum diluted in EGTA-MgCl2, and serum diluted in EDTA. The viability of L. loboi was evaluated and the fungal suspension was cytocentrifuged. The slides were submitted to immunofluorescence staining using human anti-C3 antibody. The results revealed that 98% of the fungi activated the CS by the alternative pathway and no significant difference in L. loboi viability was observed after CS activation. In parallel, frozen histological sections from 11 patients were analyzed regarding the presence of C3 and IgG by immunofluorescence staining. C3 and IgG deposits were observed in the fungal wall of 100% and 91% of the lesions evaluated, respectively. The results suggest that the CS and immunoglobulins may contribute to the defense mechanisms of the host against L.