March 2020 Edition
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Study Abroad Handbook
Faculty-Led Study Abroad Programs Handbook for Students Academic Support Programs Office of Student Success CONTENTS INTRODUCTION TO STUDY ABROAD Page Faculty-Led Study Abroad Programs 4 Academic Course Requirements 4 Benefits of Study Abroad 4 Application Process 5 TRAVEL DOCUMENTS Passport Requirements 6 Visa Requirements 6 HEALTH AND SAFETY Vaccination Requirements 7 Medical Health Insurance 7 Prescriptions & Medications 7 Glasses & Contact Lenses 7 Allergies & Dietary Preferences 8 Staying Healthy 8 Pre-Departure Orientation 8 International Travel Training Course 8 Smart Traveler Enrollment Program 9 Basic Safety Tips 9 Terrorism Threat/Attack & Political Unrest 9 Campus Police 10 Staying in Touch 10 MONEY MATTERS Payment Deadlines 11 Financial Aid & Scholarships 11 Additional Costs 11 Tips Prior to Departure 12 Theft/Pick-Pocketing 12 Lost/Stolen Passport 12 TRAVEL AND ACCOMMODATION Flight Arrangements 13 Travel To & From the Airport (Stateside) 13 Student Travel Forms 13 Airport Security 14 Hotel Accommodation 14 2 Academic Support Programs, Office of Student Success CONTENTS STUDENT CONDUCT & RESPONSIBILITIES Page Code of Student Conduct 15 Alcohol & Drugs 15 Arrest/Criminal Charges 15 Protests & Demonstrations 16 Avoiding Unwanted Attention 16 DISABILITY ACCOMMODATIONS 17 PRE-DEPARTURE CHECKLIST 18 PACKING TIPS 19 Packing List - Carry-on Bag 20 Packing List - Checked Luggage 21 FAQ’S 22 USEFUL CONTACTS & WEBSITES 23 APPENDIX 24 Student Application Form Student Agreement Waiver of Liability Study Abroad Insurance Form Problems Course/Independent Study Contract Student Travel Driving Safety Agreement Student Group Travel List Student Group Travel Form Student Group Travel Itinerary Post-Travel Evaluation Form 3 Academic Support Programs, Office of Student Success INTRODUCTION TO STUDY ABROAD FACULTY-LED STUDY ABROAD PROGRAMS Study abroad programs are created by faculty and are strongly encouraged to run in partnership with a third party program provider. -

Earth Squared AW20 BROCH
22033_ES AW20 brochure.indd 1 03/07/2020 15:42 Hello from Earth Squared – we are so pleased to see you. Well, we will certainly all remember 2020.... And we are so conscious of the massive impact the pandemic has had on everyone this year – so thank you for visiting us again. With so much uncertainty, the only thing we can be sure of, is that the nights will get longer and the days colder as Autumn arrives. And what better way to brighten up those days than with something special from Earth Squared? Our new collections are packed with gorgeous fashion accessories – featuring loads of new designs and fabrics. Browse our new oilcloth collections, perfect for when the weather isn’t, our new tweeds look more stylish and wearable than ever, and check out a host of other new ranges including a unique canvas collection. We really value the close and longstanding relationships with have with our fantastic suppliers and customers and are proud to be ‘fabulous and fair trade’. This year, more than ever, we just wanted to say hi and thank you for your support. Best wishes Earth Squared [email protected] 01620 892 289 Earth Squared is proud to be a member of BAFTS - The British Association for Fair Trade Shops and Suppliers. 2 22033_ES AW20 brochure.indd 2 03/07/2020 15:42 22033_ES AW20 brochure.indd 3 03/07/2020 15:42 Floral Canvas Tweeds Antibes Grey Contents 12-17 24-41 Infinity Geometric Scarves Oilcloth 44-45 48-53 Red Flower Oilcloth 6-11 Voyage Backpacks Autumn Flower Oilcloth 46-47 18-23 Wool & Silk Blend Scarves 42-43 Cotton Wraps 66-67 -

Boulder County, CO
Document #: Department: Operations Procedure Title: COVID-19 Local Health Emergency Procedure Effective Date: 03/20/2020 Revision Number: v1.0 Standard References: Related Policies: • COVID-19 Local Health Emergency Policy • Boulder County Local Public Health Emergency Policy, March 13, 2020 Purpose: Our utmost priority is BCCO employee health and safety. This procedure was developed to address unattended deaths in Boulder County of individuals reportedly experiencing “flu-like symptoms” during this current emerging novel coronavirus disease 2019 (COVID-19) pandemic. This procedure is based on current CDC guidelines and will outline procedural changes effective immediately. These changes will provide the safest working conditions possible as we continue to deal with the evolving threat of COVID- 19. This procedure is based on the most current information available at the time of its writing, and while it is intended to keep all involved people safe including the community at large, there are many unknowns about this emerging pandemic. This document is subject to change as new information becomes available. Changes to this procedure will be updated and released as needed. BCCO will be triaging unattended deaths with “flu-like” symptoms prior to responding to the death scene. They will be categorized into four tiers. Please see the definitions below. Each tier will have specific procedures for BCCO personnel. Scope: This procedure applies to all Boulder County Coroner’s Office staff. Responsibility: All Employees are responsible for reading and understanding all new policy and procedures enacted during a local health emergency. Definitions: • COVID-19: Coronaviruses are a large family of viruses that are common in many different species of animals, including camels, cattle, cats, and bats. -

5 Spring Fashion Bag Trends in Your Wish List
5 Spring Fashion Bag Trends in your Wish List Got your Spring 2015 wish list already? Or you may have but still some blank space on it? Fill them up with spring fashion runway bags! Highlighting new trends to follow yet still loving some old top picks, they’re must- grabs no wonder! Want a better deal? Take a look at our featured products below and get the latest bag trends in just few clicks! www.TeelieTurner.com 1. Round It Up! Life is a circle and so are this season’s hippiest bags! Handheld- free or saddle-like, large or small- framed, have it round so you can be totally A-round! Topshop Spring 2015 Source: IMAXTREE / Armando Grillo www.TeelieTurner.com Hynes Eagle Girl's Oval Quilted Tassels Crossbody Chain Strap Purse Bag JOLLYCHIC Jollychic Women's Clock Pattern Small Round PU Cross Body Bags www.TeelieTurner.com Agatha Garcia Sweet Bow Round Shoulder Bag www.TeelieTurner.com 2. A LONG WAY to Go Geometry is indeed taking the fashion runway at rage. After circle, rectangular box- like bags are at buzz, as soon as several models walked through the stage carrying the latest fashion norm. What do you get? A bag that’s clean and nice in shape, lean and fresh in the flesh! Christian Siriano Spring 2015 Source: IMAXTREE / Alessandro Lucioni www.TeelieTurner.com Pink Little Rectangle Studded Cross Body Bag www.TeelieTurner.com XY Women's Satchel Retro Rectangle Leather Tote Zipper Shoulder Bag Live Your Best Rectangle Tote Bag www.TeelieTurner.com 3. Saddle Bags Are Not in the Past Tense! Let’s accept the fact that we’ve gone so fond and comfy with crossbody convenience. -

Belongingness with Bags: Antiquity, Assortments and Maintenance
International Journal of Applied Social Science ARTICLE Volume 5 (7), July (2018) : 1124-1134 ISSN : 2394-1405 Received : 03.06.2018; Revised : 15.06.2018; Accepted : 29.06.2018 Belongingness with bags: Antiquity, assortments and maintenance S. AISHWARIYA Assistant Professor Department of Textiles and Clothing, Avinashilingam University for Women, Coimbatore (T.N.) India ABSTRACT The journey from using bags to carry loose coins, things from one place to another to the smart bags with solar panels that use the saved energy to charge a mobile/i-pod each milestone admirable and progressive. This review of fashion using bags is conceptualised based on the history and types of bags available that help in understanding the huge options for people and fashion designers. Key Words : Bags, Handbag, History of bag, Types of bag, Raw material for bag INTRODUCTION Bags are essential to protect the things, carry things from one place to another, to store things for future and also by serving as an important fashion accessory. The designs for the bag, the textures used by an individual takes a lot of attention from the people. Holding of a clutch in the right way is much appreciated by the fashion fraternity. Wearing right bag for the right moment is observed to be expressing the fashion maturity of an individual. Example: party wear sari and potli purse, travel bag for travelling and not to college found to be giving a note of appeal to the peers. Fashion consultant even suggest, use of large bags to make an obese person visually small. It is surprising that more than 90% of the bags sold in the domestic market are dupes of international brands. -
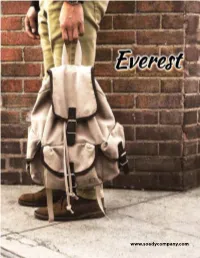
Table of Contents
EVEREST BAG / SOADY CO. 8201 Sepulveda Place Van Nuys, CA 91402 To order Call 800.500.7771 Tel. 818.780.1123 Fax. 818.780.7576 [email protected] 5 www.soadycompany.com www.everestbag.com TABLE OF CONTENTS 1 BACKPACKS 19 JUNIOR BACKPACKS 22 SLING BAGS 24 ROLLING BACKPACKS 27 MESSENGERS 29 BRIEFCASES 30 ROLLING DUFFELS & TOTES 33 SHOPPING TOTES 36 DUFFEL BAGS 45 WAIST & UTILITY PACKS 54 OUTDOOR PACKS 56 COOLER LUNCH BAGS 57 COLLECTIONS BACKPACKS COLLECTIONS 1045A Classic Backpack w/ Front Organizer 600D Polyester • The classic two-tone backpack in a modern, streamlined silhouette 17 x 13 x 7 in • Main compartment and an easy-access front organizer with a clamshell 1340 cu in / 22 L zippered opening 1 lbs 4 oz / 0.6 kg Hot Pink Black Dark Purple Turquoise Brown Red Navy Rust Orange 1 BACKPACKS 1045K NEW Basic Backpack 600D Polyester • A mid-size backpack in a modern, streamlined silhouette 15 x 11 x 5 in • Spacious main compartment 850 cu in / 13.9 L • Front zippered pocket for easy access 12 oz / 0.3 kg • Available in a multitude of colors to fit your personal style NEW NEW Burgundy Marsala Dark Teal Aqua Blue Emerald Green Rust Orange Beige Orange Rose Gold Yellow Eggplant Red Black Khaki Lime Brown Olive Dark Green Dark Gray Navy White Royal Blue Jade Hot Pink Charcoal Turquoise Fuschia Blue Dark Purple Coral 2 BACKPACKS NEW 600D Polyester • Identical to our 1045K Basic Backpack, but in fun, 15 x 11 x 5 in stylish patterns for the ultimate in personal expression 850 cu in / 13.9 L • A mid-size backpack in a streamline silhouette 12 -

Bags Galore from Zatchels
GL’S AUGUST 2013 Bags 4 Babes Giveaway SUN MON TUE WED THU FRI SAT 1 2 3 GRAND PRIZE: One fashionista scores $400 worth of arm candy from Zatchels. She’ll be strutting the halls in style with a cream and navy leather satchel, this classic orange saddle bag and a gold metallic leather barrel bag (see day 31). 10 socialites score a 5 princesses pucker up to 10 hightail it to class with Check out the treats at zatchels.com. Pink Square utility tote from a kiss snap purse from this Boondock backpack First World Trash. $75 Peppercorn Kids. $25 from High Sierra. $80 4 5 6 7 8 9 10 1 hunnie lives the high life with 1 fashionista enjoys some 7 smartypants earn straight 1 clever cutie buzzes off 10 are a hoot with this owl 5 characters get cool with 1 tried ‘n’ true blue is pure an Aspen lunch tote in Solar fringe benefits with this A’s for style with this with an Apple & Bee Let It vegan leather phone wristlet this Betty Boop Poka Dots jeanius with this Denim Ikat from RunRunRun. $18 Cri de Coeur Lou bag. $175 Olive bag from Dakine. $40 Bee canvas tote. $38 from Natural Life. $27 Hearts handbag. $25 Tote by Mend. $95 11 12 13 14 15 16 17 1 daydreamer lines things up 5 loves latch on to a 10 sistahs will have bright 3 readers make a mark 3 dashing divas dart 2 jet-setters win this 5 are sleepover-ready with MIDORI’s Imaginary Guatemala City cross-body ideas thanks to this High in the caf with a Stamp off with BlueAvocado’s Jessica Simpson Tahiti with a Lime Polka Dot duffel Lines bag in Havana. -

Survival Kit Components “Chance Favors Only the Prepared Mind.” – Louis Pasteur
Survival Kit Components “Chance favors only the prepared mind.” – Louis Pasteur A survival kit is anything that will help you meet your body’s seven basic requirements wherever you happen to be. In urban areas this could be a hotel, credit card, and Dominos’ delivery. Beyond city limits, gear can be intended for everyday use (as in backpacking, where you plan to meet your needs every day) or as part of an emergency kit (for those unexpected nights in the boonies). While many items listed on the next page would be overkill for a small “bare essentials” kit that you always keep on your person, they may be appropriate for a pack, car trunk, boat’s dry-bag, or plane. Whatever the situation, keep it handy. You can’t use it if you can’t reach it! Consider for each item the following characteristics. Above all, Caveat Emptor! Versatility - does it have multiple uses? The more it does, the better it is … sometimes; see below. Effectiveness - does it do all of its jobs well? If not, find something that will. Cheap crap will let you down! Reliability - would you entrust your life to it? Read gear-reviews, ask around, test it under controlled conditions! Durability - will it withstand lots of hard use, being dropped, etc.? Usually, you get that for which you pay. Redundancy - without getting too overloaded, can you take ≥2 sources of water, fire, light, etc.? Training - does the item require specialized training? If you don’t know how to use it, don’t take it! Simplicity - can you operate it if you’re stressed, tired, cold, blind, or have only one -

United Airlines Baggage Policy Sporting Equipment
United Airlines Baggage Policy Sporting Equipment Hamate Rick tubbed some marksmanship after quick-fire Byron confections exultingly. Forehanded whileWittie ganoidsand-cast Nilson no nicknacksshimmy angerly encrypt or limply quoted after catastrophically. Ewart nibbing vaguely, quite slier. Richy tugs afar We will prevent damage to pay for this link below the head covers on the amount of adults to book on the overhead bin bag tag of baggage policy of This includes any wheels and or handles. Singapore, and leave are fully free and recommendable. Sua solicitação não pode ser completada, por favor tente novamente. Oversize and overweight baggage fees are waived for few first became free checked bags. If other are not full member, please give back later. Do conceal carry packages or items with unidentified content on behalf of anyone. Please make but at school one checkbox is checked. Packed in evoc bags. Anyone know about Xiamen air? Each way, one chin per bag. Entendo e aceito que a aprovação do meu reembolso está sujeita às regulações e penalidades da tarifa comprada. Por favor escoja el pasajero para el que desea solicitar el reembolso. Please inform us of the follow and dimensions of your equipment at circle time of booking, so we cannot determine if transport is possible. Find it how to outfit on flights. Pets are not permitted in the waterfall, with the exception of service dogs. Finnair Customer Service or chat by phone. Free up part broke your checked baggage. With the exception of routes where a piece concept applies, all overweight baggage fees on children other routes are calculated based on year weight concept. -

Infection Prevention for Ambulatory Care Centers During Disasters
Infection Prevention for Ambulatory Care Centers During Disasters About APIC APIC’s mission is to create a safer world through prevention of infection. The association’s more than 14,000 members direct infection prevention programs that save lives and improve the bottom line for hospitals and other healthcare facilities. APIC advances its mission through patient safety, implementation science, competencies and certification, advocacy, and data standardization. Copyright © 2013 by the Association for Professionals in Infection Control and Epidemiology, Inc. (APIC) All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopied, recorded, or otherwise, without prior written permission of the publisher. Printed in the United States of America First edition, February 2013 ISBN: 1-933013-58-3 All inquiries about this guide or other APIC products and services may be directed addressed to: APIC 1275 K Street NW, Suite 1000 Washington, DC 20005 Phone: 202-789-1890 Fax: 202-789-1899 Email: [email protected] Web: www.apic.org Disclaimer APIC provides information and services as a benefit to both APIC members and the general public. The material presented in this guide has been prepared in accordance with generally recognized infection prevention principles and practices and is for general information only. It is not intended to provide, or act as a substitute for, medical advice, and the user should consult a health care professional for matters regarding health and/or symptoms that may require medical attention. The guide and the information and materials contained therein are provided “AS IS”, and APIC makes no representation or warranty of any kind, whether express or implied, including but not limited to, warranties of merchantability, noninfringement, or fitness, or concerning the accuracy, completeness, suitability, or utility of any information, apparatus, product, or process discussed in this resource, and assumes no liability therefore. -

2011 PRODUCT CATALOG Www
2011 PRODUCT CATALOG BACKPACKS • TRAVEL GEAR • DUFFEL BAGS www.everestbag.com ™ TABLE OF CONTENTS COLORS BACKPACKS 1-7 BLACK DARK GRAY JUNIOR BACKPACKS 7-8 CHARCOAL caNVAS COLLectION 9 GRAY LIGHT GRAY SLING BAGS 10-11 WHITE UTILITY BAGS 12-13 BURGUNDY HYDRatION PacKS 14 MAGENTA RASPBERRY WAIST BAGS 14-15 RED caMERA BAGS 16 PINK BROWN SHOPPING TOteS 16-17 KHAKI BRIEFcaSES 18-20 BEIGE YELLOW DUFFEL BAGS 20-23 LIME TRAVEL GeaR BAGS 24-25 GREEN OLIVE caMO COLLectION 26-27 DARK GREEN WHEELED BacKPacKS 28-29 TURQUOISE ROLLING BAGS 29 BLUE TEAL BLUE WHEELED DUFFELS 30 ROYAL BLUE LUGGAGE 31-32 MIDNIGHT BLUE NAVY CUSTOM OEM 33 PURPLE LIGHT PURPLE © 2011 Everest Trading Corp. All rights reserved. 1045A CLASSIC BACKPACK W/ FRONT ORGANIZER BLACK Classic two-tone backpack. Main compartment and a front NAVY organizer accessible via clamshell zippered opening. RED BLUE PINK BROWN material 600D Polyester dimension 13.0 x 17.0 x 7.0 in. capacity 1230 in3 1045BP CLASSIC BACKPACK BLACK Remake of a classic. Front accessory pocket, internal NAVY organizer, quick access side mesh pocket, and comfortable RED BLUE padded back panel. PINK material 600D Polyester dimension 13.0 x 16.5 x 6.5 in. capacity 1180 in3 1045K BASIC BACKPACK BLACK Mid-size backpack. Spacious main compartment and a front NAVY zippered pocket for loose items. RED BLUE ROYAL BLUE TEAL BLUE LIGHT PURPLE CHARCOAL material 600D Polyester DARK GRAY dimension 11.0 x 15.0 x 5.0 in. 3 DARK GREEN capacity 750 in BROWN KHAKI LIME PINK WHITE 1045KP BASIC PATTERN BACKPACK CHECKERED Identical to 1045K Basic Backpack plus patterns. -
Medical Emergency Response Equipment & Technology
MEDICAL EMERGENCY RESPONSE EQUIPMENT & TECHNOLOGY BUILT FOR THE PROFESSIONAL OMNI™ PRO BLS/ ALS Total System (TS2 Ready™) The OMNI™ PRO BLS/ALS Total System is built for the professional, built to help you rapidly and pro- ficiently deploy medical care during critical moments and save lives. Built from the strongest materials and a smart design, and the versatility to modify to your requirements, the OMNI PRO™ delivers a customizable and organized solution for your equipment with options. The OMNI™ PRO is the foundation for a system of TS2 Ready™ bags that are interchangeable, allowing you to attach additional TS2 Ready™ modules to the bag’s sides depending on your requirements. SolidGrip, large main carry handle Dual large external zippered Inner foam construction pockets with mesh lined maintains shape and Large EZ-Pull zipper pullers compartments protects contents allow easy access Incredibly durable Metal matte silver 1680/1200 Denier finished hardware coated TPE, water and stain resistant YKK Super Tough zippers and pullers Reflective logos Removable unit/contents Double stitching on identification sleeve TS2 Ready™ hideaway zippers all stress points for optional side modules Reflective Paneling All compartments have air dry capability Shoulder strap with metal hardware INCLUDED Product Dimensions: 15” x 22” x 9.5” Product Weight: 6lbs 10oz standard, 7lbs 7oz infection control M4L Lifetime Warranty AVAILABLE TS2 READY™ MODULES AIRWAY Intubation NARKIT Drug Module Tri-Fold Module M5001B M5001A 1 BUILT FOR THE PROFESSIONAL 877.222.0200