Medical Standards and Guidelines with Categories
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

New Jersey Facts
Interlock Device Requirements, Cont’d New Jersey *New Jersey Statutes Annotated COURT IMPOSED FINES AND PENALTIES Third offense Motor Vehicle Commission Driving Under the Influence of Alcohol or Refusing the Chemical Test, Cont’d • 1-3 years installation of interlock device after restoration of Drugs (DUI) driving privilege; or Third and Subsequent Offenses • 10 year suspension of registration privileges A person who operates a motor vehicle with a blood alcohol • 10 years driving privilege suspension concentration (BAC) of 0.08% or above is considered to be • $1,000 fine Surcharges - Alcohol Violations driving under the influence. • 12 hours minimum IDRC In addition to the court imposed fines and penalties, anyone First Offense - BAC 0.08% but less than 0.10% Refusing Chemical Test in School Zone or Crossing convicted of DUI or chemical test refusal is subject to: NEW JERSEY • 3 months driving privilege suspension • an insurance surcharge of $1,000 a year for three years First Offense • $250-$400 fine ($3,000) for the first and second conviction within a • 1 to 2 years driving privilege suspension • 12-48 hours at intoxicated driver resource center (IDRC) three-year period. • $600-$1,000 fine FACTS • Maximum 30 days imprisonment • an insurance surcharge of $1,500 a year for three years • 12 hours minimum IDRC ($4,500) for a third offense within a three-year period. First Offense - BAC 0.10% or higher Second Offense • a single $100 DUI enforcement surcharge that must be • 7 months to1 year driving privilege suspension • 4 years driving privilege suspension paid to the court with the required fine upon conviction. -

Pointing Out: How Walmart Unlawfully Punishes Workers for Medical Absences
Pointing Out: How Walmart Unlawfully Punishes Workers for Medical Absences the work and family legal center June 2017 Pointing Out: How Walmart Unlawfully Punishes Workers for Medical Absences Table of Contents By Dina Bakst, Elizabeth Gedmark & Cara Suvall* Executive Summary ...........................................................................................1 Published by A Better Balance © June 2017 Introduction ..........................................................................................................3 Our Approach .......................................................................................................6 Attendance at Walmart ....................................................................................6 The Point System ........................................................................................7 the work and family legal center Excused Absences ......................................................................................8 The “Ostrich” Approach...........................................................................9 Who We Are Unrealistic Notice Requirement ..........................................................11 A Better Balance is a national legal advocacy organization dedicated to promoting fairness in the workplace. We help workers across the economic spectrum care for their families without risking their economic security. Through legislative Legal Protections ................................................................................................12 -
Some Observations on Police-Administered Tests for Intoxication L
NORTH CAROLINA LAW REVIEW Volume 45 | Number 1 Article 9 12-1-1966 Some Observations on Police-Administered Tests for Intoxication L. Poindexter Watts Follow this and additional works at: http://scholarship.law.unc.edu/nclr Part of the Law Commons Recommended Citation L. P. Watts, Some Observations on Police-Administered Tests for Intoxication, 45 N.C. L. Rev. 34 (1966). Available at: http://scholarship.law.unc.edu/nclr/vol45/iss1/9 This Article is brought to you for free and open access by Carolina Law Scholarship Repository. It has been accepted for inclusion in North Carolina Law Review by an authorized administrator of Carolina Law Scholarship Repository. For more information, please contact [email protected]. SOME OBSERVATIONS ON POLICE-ADMIN- ISTERED TESTS FOR INTOXICATION L. POINDEXTER WATTS* TABLE OF CONTENTS Introductory ............................................................ 35 I. Clinical Symptoms of Intoxication .................................. 41 A. Verbal Description of Defendanes Condition ...................... 41 B. Observation of Defendant by Others Than Arresting Officer ....... 42 C. Examination of Defendant by Physician ........................... 42 D. Use of Alcoholic Influence Report Form and Its Standardized Tests.. 44 E. Use of Visual and Sound Recordings ............................ 46 II. Chemical Tests for Intoxication ..................................... 49 A. Direct Chemical Analysis of Blood .............................. 51 B. Chemical Analysis of Urine .................................... -

The Effectiveness and Influencing Factors of a Penalty Point System In
Accident Analysis and Prevention 131 (2019) 171–179 Contents lists available at ScienceDirect Accident Analysis and Prevention journal homepage: www.elsevier.com/locate/aap The effectiveness and influencing factors of a penalty point system in China from the perspective of risky driving behaviors T ⁎ Hongming Dong, Ning Jia, Junfang Tian , Shoufeng Ma Institute of Systems Engineering, College of Management and Economics, Tianjin University, Tianjin 300072, China ARTICLE INFO ABSTRACT Keywords: Many countries have adopted penalty point systems (PPS) to deter drivers from breaking traffic laws. To in- Penalty point system vestigate the effectiveness of PPS on reducing illegal driving behavior, this study analyzed traffic violation data Penalty experience of a Chinese city in 2017. This analysis revealed that 1) risky driving behaviors (RDBs) are among the main ffi Self-E cacy causes of traffic violations and 2) almost half of the offenders with multiple violations committed the same traffic Risky driving behaviors rule violations more than once. To further explain these phenomena, a survey in another Chinese city–Tianjin–was conducted. Considering the fact that most types of RDBs will, if detected by the authorities, result in traffic violations, the present study investigated the influence of a PPS, represented by penalty ex- perience (PE), on traffic violation behaviors from the perspective of RDBs. Moreover, the impact of cognitive processes on driving behaviors via self-efficacy was considered. We found that drivers’ PE is positively associated with their RDBs and that offenders with more PE are more inclined to commit RDBs; we further observed that self-efficacy partially mediates the relationship between PE and RDBs. -

Wisconsin Motorists Handbook
Motorists’ Handbook WISCONSIN DEPARAugustTMENT 2021 OF TRANSPORTATION August 2021 CONTENTS CONTENTS PRELIMINARY INFORMATION 1 BEFORE YOU DRIVE 10 Address change 1 Plan ahead and save fuel 10 Obtain services online 1 Check the vehicle 10 Obtain information 1 Clean glass surfaces 12 Consider saving a life Adjust seat and mirrors 12 by becoming an organ donor 2 Use safety belts and child restraints 13 Absolute sobriety 2 Wisconsin Graduated Driver Licensing RULES OF THE ROAD 15 Supervised Driving Log, HS-303 2 Traffic control devices 15 This manual 2 TRAFFIC SIGNALS 16 DRIVER LICENSE 2 Requirements 3 TRAFFIC SIGNS 18 Carrying the driver license and license Warning signs 18 replacement 4 Regulatory signs 20 Out of state transfers 4 Railroad crossing warning signs 23 Construction signs 25 INSTRUCTION PERMIT 5 Guide signs 25 Restrictions of the instruction permit 6 PAVEMENT MARKINGS 26 PROBATIONARY LICENSE 6 Edge and lane lines 27 Restrictions of the probationary license 7 White lane markings 27 The skills test 7 Crosswalks and stop lines 27 KEEPING THE DRIVER LICENSE 8 Yellow lane markings 27 Point system 8 Shared center lane 28 Habitual offender 9 OTHER LANE CONTROLS 29 Occupational license 9 Reversible lanes 29 Reinstating a revoked or suspended license 9 Reserved lanes 29 Driver license renewal 9 Flex Lane 30 Motor vehicle liability insurance METERED RAMPS 31 requirement 9 How to use a ramp meter 31 COVER i CONTENTS RULES FOR DRIVING SCHOOL BUSES 44 ROUNDABOUTS 32 General information for PARKING 45 all roundabouts 32 How to park on a hill -

Special Point Examination Driver's Handbook
Special Point Examination Driver’s Handbook Pub. 248 (1-04) Table of Contents The Examination Requirement . 1 Study Guide and Sample Test Items Part 1: . 3 Part 2 Pennsylvania Safe Driving Laws and Practices. 3 : Avoiding Accidents Through Safe Driving Decisions . 10 General Examination Information . 20 How to Make Your Examination Appointment . 20 Americanʼs with Disabilities Act (ADA) . 20 Procedures for Taking the Examination . 21 Scoring of Examination Results. 21 AVISO: Para obtener este manual en Español, telefonee 1-800-932-4600 i The Examination Requirement As a driver who has been convicted of violations of Pennsylvaniaʼs Vehicle Code resulting in six or more points on your driving record, you must take and pass a written test to keep your driverʼs license. The test will have two kinds of questions. The first kind will test what you know about safe driving laws and safe driving practices. The second kind will test your judgment in making safe or unsafe driver decisions in everyday traffic situations where accidents are likely to happen. For the questions about Pennsylvaniaʼs safe driving laws and safe driving practices you will need to know: • How the point system works in Pennsylvania. • Laws and penalties for driving while under the influence of alcohol or drugs. • Effects of alcohol, drugs and medication on your driving skills. • Facts about seat belt safety. • Other key traffic safety issues. You will find all the information that you need to know and sample test questions in the Study Guide part of this Handbook. Learn the information in detail. On the test, you will be asked to answer “True” or “False” to information given in this section. -
Summary of State Speed Laws
DOT HS 810 826 August 2007 Summary of State Speed Laws Tenth Edition Current as of January 1, 2007 This document is available to the public from the National Technical Information Service, Springfield, Virginia 22161 This publication is distributed by the U.S. Department of Transportation, National Highway Traffic Safety Administration, in the interest of information exchange. The opinions, findings, and conclusions expressed in this publication are those of the author(s) and not necessarily those of the Department of Transportation or the National Highway Traffic Safety Administration. The United States Government assumes no liability for its contents or use thereof. If trade or manufacturers' names or products are mentioned, it is because they are considered essential to the object of the publication and should not be construed as an endorsement. The United States Government does not endorse products or manufacturers. TABLE OF CONTENTS Introduction ...................................................iii Missouri ......................................................138 Alabama..........................................................1 Montana ......................................................143 Alaska.............................................................5 Nebraska .....................................................150 Arizona ...........................................................9 Nevada ........................................................157 Arkansas .......................................................15 New -
Point System Regulations and Schedule
MVD–11011 REV. 02/12 New Mexico Taxation & Revenue Department, Motor Vehicle Division POINT SYSTEM REGULATIONS AND SCHEDULE Point System Statute and Regulations New Mexico Statute (Sec. 66-5-30 NMSA 1978) and Rule (18.19.5.50-57 NMAC) authorize the Department to suspend the driver’s license of an individual who has been convicted of violations of the traffic laws with such frequency as to show disrespect for those laws or has been found to be an habitually reckless or negligent driver of a motor vehicle. To provide a reasonable, objective and fair method by which the Department may determine whether an individual shows disrespect for the traffic laws of this state through frequency of conviction for violations or is habitually reckless or negligent and to promote the public safety by removing such drivers from the roads, the Department establishes a “point system” with these regulations. However, Sec. 66-7-302.2 NMSA 1978 prohibits the assignment of points for convictions for speeding on rural highways except in Bernalillo County. A “rural highway” is that part of a highway that is located at least two miles outside of the boundaries of an incorporated city, town or village. Exceptions: The point system shall apply on rural highways for vehicles weighing 12,000 pounds and more and for speeding convictions if excessive speed of the motorist cited was a factor in an accident. 18.19.5.52 NMAC - Schedule of Points for Violations Points to be assessed for conviction of violations of provisions of the Motor Vehicle Code are scheduled in Parts A through F below. -

Virginia DMV Point System for Traffic
Virginia DMV Point System For Traffic Law Riley & Wells Attorneys-At-Law | (804) 673-7111 | www.rileywellslaw.com | [email protected] Introduction To Traffic Point System For Offense Convictions Riley & Wells Attorneys-At-Law is a Virginia law firm located in the Richmond VA Metropolitan Area that focuses a significant portion of its law practice to defending clients accused of traffic violations. Traffic violation convictions can negatively affect driving privileges, the driving record and an automobile insurance policy. We consult with clients daily about how their case will be treated by the Courts, the Virginia Department of Motor Vehicles (DMV) and ultimately an automobile insurance company. The purpose of this guide is to explain how traffic violations can affect the driving record and driving privileges in the Commonwealth of Virginia. Overview Reckless Driving Moving Violations Any Virginia traffic violation that results in a conviction, even offenses that do not carry demerit points, is posted to the Virginia driving record. In Virginia, the Virginia court notifies the DMV if a motorist is convicted of a traffic violation. An allegation or the mere issuance of a Virginia Uniform Summons (the ticket) does not post to the Virginia driving record. EXAMPLE: A Virginia State Trooper issues a Virginia Uniform Summons to a motorist for reckless driving. The motorist retains a Virginia Traffic Lawyer to defend the reckless driving allegation. The attorney successfully defends the case and the allegation is eventually dismissed. The Court does not notify the DMV about the reckless driving. Thus, no reckless driving case is posted to the driving record and the automobile insurance company never finds out about the reckless driving case. -
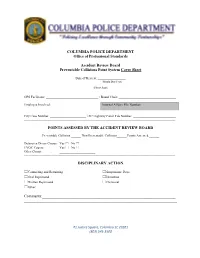
02.06B ARB Point System Guide
COLUMBIA POLICE DEPARTMENT Office of Professional Standards Accident Review Board Preventable Collisions Point System Cover Sheet Date of Review: _________________ (Month/Day/Year) (Please Print) OPS Facilitator: ________________________________ / Board Chair: ___________________________________ Employee Involved: Internal Affairs File Number: ______________________________ City Case Number: ______________________ / SC Highway Patrol File Number: __________________________ ------------------------------------------------------------------------------------------------------------------------------------------- POINTS ASSESSED BY THE ACCIDENT REVIEW BOARD Preventable Collision ______ Non-Preventable Collision______ Points Assessed:______ Defensive Driver Course: Yes ☐ No ☐ EVOC Course: Yes ☐ No ☐ Other Course: ______________________ ------------------------------------------------------------------------------------------------------------------------------------------- DISCIPLINARY ACTION ☐Counseling and Retraining ☐Suspension: Days _________________ ☐Oral Reprimand ☐Demotion ☐Written Reprimand ☐Dismissal ☐Other: ______________________ Comments:____________________________________________________________________ ______________________________________________________________________________ ______________________________________________________________________________ ______________________________________________________________________________ ______________________________________________________________________________ #1 Justice Square, -

Fostering Epilepsy Care in Europe All Rights Reserved
EPILEPSY IN THE WHO EUROPEAN REGION: Fostering Epilepsy Care in Europe All rights reserved. No part of this publication may be reproduced, stored in a database or retrieval system, or published, in any form or any way, electronically, mechanically, by print, photoprint, microfilm or any other means without prior written permission from the publisher. Address requests about publications of the ILAE/IBE/WHO Global Campaign Against Epilepsy: Global Campaign Secretariat SEIN P.O. Box 540 2130 AM Hoofddorp The Netherlands e-mail: [email protected] ISBN NR. 978-90-810076-3-4 Layout/ Printing: Paswerk Bedrijven, Cruquius, Netherlands Table of contents Foreword ................................................................................................................................................. 4 Preface ................................................................................................................................................. 5 Acknowledgements ........................................................................................................................................ 6 Tribute ................................................................................................................................................. 7 Abbreviations ................................................................................................................................................. 8 Background information on the European Region ......................................................................................... -

MVR Evaluation
MVR Evaluation Loss Control Bulletin MVR Evaluation One of the most effective fleet management tools is a driver’s Motor Vehicle Record (MVR). A MVR details an individual’s past driving history indicating violations and accidents over a specified period. Frequency is as much a concern as severity when evaluating a MVR. Equal emphasis should be placed on someone who, during the last three years, has had one minor accident and multiple speeding violations as someone who has had one major violation in the same amount of time. Recent history is the most important. A driver who had several moving violations over three years ago may be a better risk than a driver who had two violations within the last 12 months. All employees should be held to the same MVR standards. When to Order MVRs MVRs should be reviewed for each type of driver (currently employed or prior to placement) in a job with driving duties. Order MVRs in the following situations: Upon hire or placement in a driving position: It is critical to review the MVR before asking a driver to go out on the road on • your behalf. Some companies wait until the next scheduled annual review or until their agent, broker, or insurance carrier asks for an updated driver list. However, this is a risky practice. No employee should be permitted to drive on company business until a MVR check has been completed. After an accident happens or a Motorist Observation Report is received: One way to determine if there has been a • change in a driver’s behavior is to obtain a MVR following an accident or after a call-in report/complaint has been received.