West Virginia Nurse
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Listed the Senate and House Education Committees Below Because That’S the Two We Most Often Deal With
Here is a link to the House roster where you will find contact information for House members: http://www.wvlegislature.gov/house/roster.cfm Here is a link to the Senate roster where you will find contact information for Senate members: https://www.wvlegislature.gov/senate1/roster.cfm Please make sure you are familiar with your local legislators as well as those in leadership positions. The new directory is available on the legislative site. I listed the Senate and House Education Committees below because that’s the two we most often deal with. WEST VIRGINIA STATE SENATE LEADERSHIP SENATE PRESIDENT— CRAIG P. BLAIR PREIDENT PRO TEMPORE – DONNA BOLEY MAJORITY LEADER – TOM TAKUBO MAJORITY WHIP – RYAN W. WELD MINORITY LEADER – STEPHEN BALDWIN MINORITY WHIP – MICHAEL WOELFEL SENATE EDUCATION COMMITTEE Patricia Rucker - Chair Robert Karnes - Vice Chair Azinger, Beach, Boley, Clements, Grady, Plymale, Roberts, Romano, Stollings, Tarr, Trump, Unger SENATE FINANCE Eric Tarr - Chair Dave Sypolt - Vice Chair Baldwin, Boley, Clements, Hamilton, Ihlenfeld, Jeffries, Maroney, Martin, Nelson, Plymale, Roberts, Stollings, Swope, Takubo, Unger SENATE DISTRICT - 01 William Ihlenfeld (D - Ohio) Ryan Weld (R - Brooke) SENATE DISTRICT - 02 Michael Maroney (R - Marshall) Charles Clements (R - Wetzel) SENATE DISTRICT - 03 Donna Boley (R - Pleasants) Michael Azinger (R - Wood) SENATE DISTRICT - 04 Amy Grady (R - Mason) Eric Tarr (R - Putnam) SENATE DISTRICT - 05 Robert Plymale (D - Wayne) Michael Woelfel (D - Cabell) SENATE DISTRICT - 06 Chandler Swope (R - Mercer) -

West Virginia Broadband Enhance Council 2020 Annual Report
2020 West Virginia Broadband Enhancement Council 2020 ANNUAL REPORT TO THE WEST VIRGINIA LEGISLATURE Table of Contents 1. Executive Summary ............................................................................................................................... 1 2. Existing, Continuing and New Initiatives ............................................................................................... 2 3. Broadband Mapping ............................................................................................................................. 4 Key Components of the Interactive Mapping System .................................................................. 4 Broadband Advertised Speed Ranges Interactive Map ................................................................ 5 Broadband Development Hub ...................................................................................................... 6 Public Wi-Fi Map ........................................................................................................................... 6 Public Project Development ......................................................................................................... 7 Speed Tiers by County ................................................................................................................... 8 Speed Tiers Statewide ................................................................................................................... 8 Providers Statewide ..................................................................................................................... -

2019-2020 PAC Contributions
2019-2020 Election Cycle Contributions State Candidate or Committee Name Party -District Total Amount ALABAMA Sen. Candidate Thomas Tuberville R $5,000 Rep. Candidate Jerry Carl R-01 $2,500 Rep. Michael Rogers R-03 $1,500 Rep. Gary Palmer R-06 $1,500 Rep. Terri Sewell D-07 $10,000 ALASKA Sen. Dan Sullivan R $3,800 Rep. Donald Young R-At-Large $7,500 ARIZONA Sen. Martha McSally R $10,000 Rep. Andy Biggs R-05 $5,000 Rep. David Schweikert R-06 $6,500 ARKANSAS Sen. Thomas Cotton R $7,500 Rep. Rick Crawford R-01 $2,500 Rep. French Hill R-02 $9,000 Rep. Steve Womack R-03 $2,500 Rep. Bruce Westerman R-04 $7,500 St. Sen. Ben Hester R-01 $750 St. Sen. Jim Hendren R-02 $750 St. Sen. Lance Eads R-07 $750 St. Sen. Milton Hickey R-11 $1,500 St. Sen. Bruce Maloch D-12 $750 St. Sen. Alan Clark R-13 $750 St. Sen. Breanne Davis R-16 $500 St. Sen. John Cooper R-21 $750 St. Sen. David Wallace R-22 $500 St. Sen. Ronald Caldwell R-23 $750 St. Sen. Stephanie Flowers D-25 $750 St. Sen. Eddie Cheatham D-26 $750 St. Sen. Trent Garner R-27 $750 St. Sen. Ricky Hill R-29 $500 St. Sen. Jane English R-34 $1,500 St. Rep. Lane Jean R-02 $500 St. Rep. Danny Watson R-03 $500 St. Rep. DeAnn Vaught R-04 $500 St. Rep. David Fielding D-05 $500 St. Rep. Matthew Shepherd R-06 $1,000 St. -

Current Office Holders
Federal Name Party Office Term Next Election Joe Biden Democrat U.S President 4 Years 2024 Kamala Harris Democrat U.S. Vice President 4 Years 2024 Joe Manchin Democratic U.S. Senate 6 Years 2024 Shelley Moore Capito Republican U.S. Senate 6 Years 2026 David McKinley Republican U.S House, District 1 2 Years 2022 Alexander Mooney Republican U.S. House, District 2 2 Years 2022 Carol Miller Republican U.S. House, District 3 2 Years 2022 State Name Party Office Term Next Election Jim Justice Republican Governor 4 Years 2024 Mac Warner Republican West Virginia Secretary of State 4 Years 2024 John "JB" McCuskey Republican West Virginia State Auditor 4 Years 2024 Riley Moore Republican West Virginia State Treasurer 4 Years 2024 Patrick Morrisey Republican Attorney General of West Virginia 4 Years 2024 Kent Leonhardt Republican West Virginia Commissioner of Agriculture 4 Years 2024 West Virginia State Senate Name Party District Next election Ryan W. Weld Republican 1 2024 William Ihlenfeld Democrat 1 2022 Mike Maroney Republican 2 2024 Charles Clements Republican 2 2022 Donna J. Boley Republican 3 2024 Mike Azinger Republican 3 2022 Amy Grady Republican 4 2024 Eric J. Tarr Republican 4 2022 Robert H. Plymale Democrat 5 2024 Mike Woelfel Democrat 5 2022 Chandler Swope Republican 6 2024 Mark R Maynard Republican 6 2022 Rupie Phillips Republican 7 2024 Ron Stollings Democrat 7 2022 Glenn Jeffries Democrat 8 2024 Richard Lindsay Democrat 8 2022 David Stover Republican 9 2024 Rollan A. Roberts Republican 9 2022 Jack Woodrum Republican 10 2024 Stephen Baldwin Democrat 10 2022 Robert Karnes Republican 11 2024 Bill Hamilton Republican 11 2022 Patrick Martin Republican 12 2024 Mike Romano Democrat 12 2022 Mike Caputo Democrat 13 2024 Robert D. -

West Virginia Nurse
WEST VIRGINIA NURSE “Nurses working together for a healthy West Virginia” The official publication of the West Virginia Nurses Association Quarterly publication direct mailed to approximately 38,000 RNs & LPNs in West Virginia. October, November, December 2018 Volume 21 • No. 4 State Elections are Coming Right Up! Joyce Wilson, APRN, FNP-BC / • There are 67 House districts, with 1 to 5 delegates Inside: Chair, West Virginia Nurses PAC per district The West Virginia Nurses Political Action Committee • Length of term for delegates is two years, meaning President’s Message ......... 2 (WVN-PAC) has been hard at work as the November 6, all the seats are up for election right now 2018, election approaches. WVN-PAC is nonpartisan and • There are 17 Senate districts Conferences and Meetings ... 3 does not endorse based on party affiliation. Instead, • Each Senate district has two senators, serving we focus on which candidates will best work for the staggered four-year terms New Nurse Entrepreneur Mountain State’s nurses. • This means half of the Senate is up for reelection After an exhaustive and exhausting review currently Course Launches • There are 34 senators total (= 2 x 17) October 2018 ............. 6 process, we are happy to present our list of candidate endorsements. Our work included reviewing about 100 If you want to check on your voter registration, we Call for Nominations candidate questionnaires, seeking recommendations have a link for that! https://services.sos.wv.gov/Elections/ from many nurse leaders at the Senate and House of Voter/AmIRegisteredToVote to WVNA Board ............ 6 Delegates district levels, analyzing the voting records of each incumbent, meeting in person with many Need to contact your county clerk? Emerging Nurse candidates and allies of WVNA, conducting phone https://sos.wv.gov/elections/Pages/ Leader Updates ........... -

2021 State Legislator Pledge Signers
I pledge that, as a member of the state legislature, I will cosponsor, vote for, and defend the resolution applying for an Article V convention for the sole purpose of enacting term limits on Congress. The U.S. Term Limits Article V Pledge Signers 2021 State Legislators 1250 Connecticut Ave NW Suite 200 ALABAMA S022 David Livingston H073 Karen Mathiak Washington, D.C. 20036 Successfully passed a term S028 Kate Brophy McGee H097 Bonnie Rich (202) 261-3532 limits only resolution. H098 David Clark termlimits.org CALIFORNIA H103 Timothy Barr ALASKA H048 Blanca Rubio H104 Chuck Efstration H030 Ron Gillham H105 Donna McLeod COLORADO H110 Clint Crowe ARKANSAS H016 Andres Pico H119 Marcus Wiedower H024 Bruce Cozart H022 Margo Herzl H131 Beth Camp H042 Mark Perry H039 Mark Baisley H141 Dale Washburn H071 Joe Cloud H048 Tonya Van Beber H147 Heath Clark H049 Michael Lynch H151 Gerald Greene ARIZONA H060 Ron Hanks H157 Bill Werkheiser H001 Noel Campbell H062 Donald Valdez H161 Bill Hitchens H001 Judy Burges H063 Dan Woog H162 Carl Gilliard H001 Quang Nguyen H064 Richard Holtorf H164 Ron Stephens H002 Andrea Dalessandro S001 Jerry Sonnenberg H166 Jesse Petrea H002 Daniel Hernandez S010 Larry Liston H176 James Burchett H003 Alma Hernandez S023 Barbara Kirkmeyer H177 Dexter Sharper H005 Leo Biasiucci H179 Don Hogan H006 Walter Blackman CONNECTICUT S008 Russ Goodman H007 Arlando Teller H132 Brian Farnen S013 Carden Summers H008 David Cook H149 Kimberly Fiorello S017 Brian Strickland H011 Mark Finchem S021 Brandon Beach H012 Travis Grantham FLORIDA S027 Greg Dolezal H014 Gail Griffin Successfully passed a term S030 Mike Dugan H015 Steve Kaiser limits only resolution. -

West Virginians for Life PAC Endorsed Pro-Life Candidates - GENERAL 2018
West Virginians for Life PAC Endorsed Pro-Life Candidates - GENERAL 2018 US Senate - Patrick Morrisey (R) Dist. 2 - Becky Uhlly (R) Dist. 24 - Jordan Bridges (R) Dist. 44 - Dana Lynch (D) Dist. 3 - Dalton Haas (R) Ralph Rodighiero (D) Dist. 45 - Carl R. “Robbie” Martin (R) US House - Dist 1 - David McKinley (R) Erikka Storch (R) Dist. 25 - Tony Paynter (R) Dist. 46 - Patrick Martin (R) Dist 2 - Alex Mooney (R) Dist. 4 - Charlie Reynolds (R) Dist. 26 - David Cox (R) Dist. 47 - Chris Phillips (R) Dist 3 - Carol Miller (R) Dist. 5 - Phillip Wiley (R) Dist. 27 - Joe Ellington (R) Dist. 48 - Danny Hamrick (R) Supreme Court (Div. 1) - Tim Armstead Dist. 6 - David Kelly (R) Eric Porterfield (R) Ben Queen (R) (Div. 2) - Evan Jenkins Dist. 7 - Jason Harshbarger (R) John Shott (R) Terry Waxman (R) Dist. 8 - Bill Anderson (R) Dist. 28 - Roy Cooper (R) Robert “Rob” Garcia (D) 13th Judicial Circuit - Dan Greear Dist. 9 - Ray Hollen (R) Jeffrey Pack (R) Dist. 49 - Amy Summers (R) WV State Senate Dist. 10 - Tom Azinger (R) Dist. 29 - Ricky Moye (D) Dist. 50 - Phil Mallow (R) Dist. 1 - Ryan Ferns (R) Vernon Criss (R) Dist. 31 - Christopher Toney (R) Guy Ward (R) Dist. 2 - Charles Clements (R) John Kelly (R) Dist. 32 - Tom Fast (R) Dist. 51 - Cindy Frich (R) Dist. 3 - Mike Azinger (R) Dist. 11 - Martin “Rick” Atkinson (R) Austin Haynes (R) Roger Shuttlesworth (R) Dist. 4 - Eric Tarr (R) Dist. 12 - Steve Westfall (R) Kayla Kessinger (R) Joe Statler (R) Dist. 5 - Mike Woelfel (D) Dist. -

West Virginia Nurse
WEST VIRGINIA NURSE “Nurses working together for a healthy West Virginia” The official publication of the West Virginia Nurses Association Quarterly publication distributed to approximately 19,600 RNs & LPNs in West Virginia. October, November, December 2020 Volume 21 • No. 4 PRESIDENT’S MESSAGE Inside: Dear WV Nurse Colleagues, • We have helped long-term care facilities and In my 35 years of nursing, clinics obtain much-needed PPE. We have also Executive Director’s Message .. 2 I can honestly say that I have helped connect them to places that could never worked during a time safely clean PPE for reuse. such as this: a time when so • We’ve continued the discussion of staffing Conferences and Meetings ... 3 many people are suffering, safety and making our plans for the upcoming and things are changing so legislative session. Corrections ................ 3 fast. It seems that every day there are new regulations, The Zoom meetings we have been having with the guidelines, and treatments WV Association of School Nurses (WVASN) have been 2020 Elections Are for fighting COVID-19 and we particularly eye-opening. As I write this, school is all are experiencing anxiety Joyce Wilson opening in a week. During a normal school year, the Coming Soon .......... 4-5 and fatigue. school nurses’ job is demanding – including making There are some things that never change, care plans for students with chronic illness and Three Risk Areas Nurses Face in however. The weather is cooling, the leaves are keeping all students up to date with immunizations turning, and the boots-on-the-ground nurses are and yearly check-ups. -
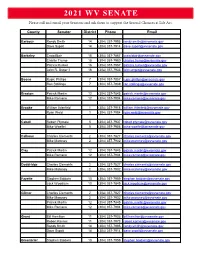
2021 WV SENATE Please Call and Email Your Senators and Ask Them to Support the Second Chances at Life Act
2021 WV SENATE Please call and email your Senators and ask them to support the Second Chances at Life Act. Please call and email your Senators and ask them to support the Second Chances at Life Act. County Senator District Phone Email Barbour Randy Smith 14 (304) 357-7995 [email protected] Dave Sypolt 14 (304) 357-7914 [email protected] Berkeley Craig Blair 15 (304) 357-7867 [email protected] Charlie Trump 15 (304) 357-7980 [email protected] Patrica Rucker 16 (304) 357-7957 [email protected] John R. Unger II 16 (304) 357-7933 [email protected] Boone Rupie Phillips 7 (304) 357-7857 [email protected] Ron Stollings 7 (304) 357-7939 [email protected] Braxton Patrick Martin 12 (304) 357-7845 [email protected] Mike Romano 12 (304) 357-7904 [email protected] Brooke William Ihlenfeld 1 (304) 357-7918 [email protected] Ryan Weld 1 (304) 357-7984 [email protected] Cabell Robert Plymale 5 (304) 357-7937 [email protected] Mike Woelfel 5 (304) 357-7956 [email protected] Calhoun Charles Clements 2 (304) 357-7827 [email protected] Mike Maroney 2 (304) 357-7902 [email protected] Clay Patrick Martin 12 (304) 357-7845 [email protected] Mike Romano 12 (304) 357-7904 [email protected] Doddridge Charles Clements 2 (304) 357-7827 [email protected] Mike Maroney 2 (304) 357-7902 [email protected] Fayette Stephen Baldwin 10 (304) 357-7959 [email protected] Jack Woodrum 10 (304) -
In This Issue S.B. 673: Location of Civil Actions for A
IN THIS ISSUE LB 2021–06 March 22, 2021 Call Senators Today CONTACT SENATORS TODAY TO SUPPORT S.B. 673, on S.B. 673 CONSTRUCTION VENUE BILL CAWV members are asked to call Senators TODAY, MARCH 22, to Today Last Day for encourage them to vote YES on S.B. 673. The bill is on the agenda for Senate Judiciary Committee at 3:00 p.m. today. Bill Introduction The bill was developed by the CAWV Legislative Committee to mandate that West Virginia is the location where construction must be resolved if a List of Bills Introduced Last Week party to a West Virginia construction contract breaches that contract. Virginia, Ohio and Pennsylvania have legislation that voids any language in a boilerplate contract that forces in state firms to resolve any disputes in the state where the project owner resides, thereby requiring the contractor or subcontractor to hire out of state counsel. Below is a fact sheet on S.B. 673 detailing the purpose of the bill and why legislators should vote YES. Members can relate instances where they have either had to resolve a dispute in another state or decided not to take action due to the cost involved with litigating the claim in another state. At the end of this week’s Legislative Bulletin is a list of Senators and their contact information. PLEASE TRY TO CONTACT SENATORS BY 1:00 P.M. TODAY, MARCH 22. S.B. 673: LOCATION OF CIVIL ACTIONS FOR A CONSTRUCTION PROJECT IN WEST VIRGINIA FACT SHEET ◼ Many construction professionals are used to seeing venue and choice-of-law provisions in construction contracts. -

WVMA Endorses Legislative, Supreme Court Candidates
Contact: Rebecca McPhail, WVMA President Phone: (304) 767-5189 // Email: [email protected] FOR IMMEDIATE RELEASE October 2, 2018 WVMA Endorses Legislative, Supreme Court Candidates CHARLESTON, W.Va. ─ The West Virginia Manufacturers Association has endorsed a bipartisan list of 70 candidates for legislative office and made endorsements in races for the West Virginia Supreme Court of Appeals. Regarding the legislative races, the mix of incumbents and new candidate endorsements represents those whose political philosophy is aligned with the best interests of West Virginia’s manufacturers, said WMVA President Rebecca McPhail. “Regardless of party affiliation, our endorsements reflect the results detailed in our AssembleWV legislative scorecard and how candidates responded to our survey,” McPhail explained. “WVMA members have unique policy needs that are not always the same as other segments of the business community. I encourage candidates to reach out to us for a conversation about our needs regardless of whether they earned our endorsement.” AssembleWV, a political advocacy organization affiliated with the West Virginia Manufacturers Association (WVMA), scored members of the 83rd Legislature for their actions on several pieces of legislation during the 2017 and 2018 legislative sessions. As the scorecard explains, the bills used to measure legislator performance were weighted based on their importance to manufacturers, regardless of whether the bills passed. Scores ranged from 100 percent down to 17.6 percent. All lawmakers can access the scorecard and are encouraged to contact the WVMA with questions. For the Supreme Court endorsements, the WVMA endorsed candidates its members believe will be most faithful to the West Virginia Constitution, will avoid judicial activism and will restore integrity and public trust in the state’s highest court, McPhail said. -

2021 Wv House Photo
West VirgiNia House of Delegates RepublicaNs Joshua JoNathaN PiNsoN JohNNie Geoff Foster HiggiNbotham (13) (13) Wamsley (14) (15) Mark Zatezalo Pat McGeehaN Erikka Storch Charlie David Kelly (1) (1) (3) ReyNolds (4) (6) TreNtoN BarNhart Bill ANdersoN ShaNNoN Kimes (7) (8) (9) DaNiel JohN VerNoN Criss Roger CoNley LiNville (16) MaNdt (16) (10) (10) Matthew EvaN Worrell Josh Booth (19) Mark DeaN JohN Kelly Rohrbach (17) (18) (21) (10) Joe Jeffries Zack MayNard Josh HolsteiN Margitta JordaN Bridges Riley KeatoN Steve Westfall (22) (22) (23) Mazzocchi (24) (24) (11) (12) Updated 2-9-2021 West VirgiNia House of Delegates RepublicaNs Moore Capito Larry Pack Chris Pritt DiaNNa Graves DaNa Ferrell (35) (35) (36) (38) (39) ToNy PayNter Marty Gearheart Joe ElliNgtoN Doug Smith Roy Cooper (25) (27) (27) (27) (28) Joe Jeffries (22) Jeffrey Pack BraNdoN Steele Christopher ToNey (28) (29) (31) Tom Fast (32) DeaN Jeffries Heather Tully Barry Bruce Todd LoNgaNacre AustiN HayNes (40) (41) (42) (42) (32) Ty Nestor Caleb HaNNa Carl MartiN Adam Kayla KessiNger Roger HaNshaw (43) (44) (45) Burkhammer (46) (32) (33) Updated 2-9-2021 West VirgiNia House of Delegates RepublicaNs BryaN Ward Gary G. Howell Ruth RowaN George Miller (55) (56) (57) (58) Chris Phillips DaNNy Hamrick Laura Kimble BeN QueeN Clay Riley (47) (48) (48) (48) (48) Amy Summers Phil Mallow Guy Ward (49) (50) (50) Joe Statler (51) KeN Reed DoN Forsht JasoN Barrett Chuck Horst (59) (60) (61) (62) Terri Sypolt (52) JohN Hardy Eric Householder WayNe Clark Paul EspiNosa (63) (64) (65) (66) Buck JeNNiNgs JohN Hott (53) (54) Updated 2-9-2021 West VirgiNia House of Delegates Democrats BreNt Boggs Doug Skaff Kayla YouNg Jim Barach Larry Rowe (34) (35) (35) (36) (36) Phillip Diserio ShawN Fluharty Lisa Zukoff (2) (3) (4) Dave Pethtel SeaN HorNbuckle Chad Lovejoy (5) (16) (17) Ric Griffith (19) Mike PushkiN Cody ThompsoN Joey Garcia NathaN BrowN (37) (43) (50) (20) Barbara EvaN HaNseN DaNielle JohN Willlams JohN Doyle Fleischauer (51) Walker (51) Ed EvaNs Mick Bates (51) (51) (67) (26) (30) Updated 2-9-2021.