A Thesis Entitled a Parametric Study of Physiological Changes To
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Between Ligamentous Structures in the Thoracic Spine : a finite Element Investigation
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Queensland University of Technology ePrints Archive This is the author’s version of a work that was submitted/accepted for pub- lication in the following source: Little, J. Paige & Adam, Clayton J. (2011) Effects of surgical joint desta- bilization on load sharing between ligamentous structures in the thoracic spine : a finite element investigation. Clinical Biomechanics, 26(9), pp. 895-903. This file was downloaded from: http://eprints.qut.edu.au/48159/ c Copyright 2011 Elsevier Ltd. NOTICE: this is the author’s version of a work that was accepted for publication in the journal Clinical Biomechanics. Changes resulting from the publishing process, such as peer review, editing, corrections, struc- tural formatting, and other quality control mechanisms may not be re- flected in this document. Changes may have been made to this work since it was submitted for publication. A definitive version was sub- sequently published in Clinical Biomechanics 26 (2011) 895–903, DOI: 10.1016/j.clinbiomech.2011.05.004 Notice: Changes introduced as a result of publishing processes such as copy-editing and formatting may not be reflected in this document. For a definitive version of this work, please refer to the published source: http://dx.doi.org/10.1016/j.clinbiomech.2011.05.004 *Manuscript (including title page & abstract) Effect of surgical joint destabilization on ligament load-sharing 1 Effects of surgical joint destabilization on load sharing 2 between ligamentous structures in the thoracic spine: A 3 Finite Element investigation 4 5 Authors: 6 J. -

Lyrics Words and Music by Edward Eliscu, Billy Rose and Vincent Youmans
Great Day Lyrics Words and Music by Edward Eliscu, Billy Rose and Vincent Youmans When you’re down and out Lift up your head and shout “There’s gonna be a great day!” Angels in the sky promise that by and by there’s gonna be a great day! Gabriel will warn you, Some early morn you will hear his horn. Rooty, tootin’. It’s not far away, Lift up your head and say, ”There’s gonna be a great day, great day!” When you’re down and out, Lift up your head and shout, “There’s gonna be a great day!” Angels in the sky Promise that by and by There’s gonna be a great day! Gabriel will warn you, Some early morn you will hear his horn. Rooty, tootin’. It’s not far away, Lift up your head and say, ”There’s gonna be a great day, great day!” When you’re down and out, Lift up your head and shout, “There’s gonna be a great day!” Angels in the sky say that by and by There’s gonna be a great day. Gabriel will warn you, Some early morn you will hear his horn. Rooty, tootin’, rooty tootin’, rooty tootin’, rooty tootin’. It’s not very far away, Lift your head and say, ”There’s gonna be a great day!” ”There’s gonna be a great day!” © 1929 WB Music Corp., Chappell & Co. (admin. by © Warner Chappell Music) / LSQ Music Company (admin. by Songwriters Guild of America). All rights reserved. Used by permission. Love Is Like a River Lyrics Words and Music by Suzanne Jennings and Jeff Silvey His love is like a river, runnin’ and a rollin’, Flowin’ from the lazy streams. -

Canine Thoracic Costovertebral and Costotransverse Joints Three Case Reports of Dysfunction and Manual Therapy Guidelines for A
Topics in Compan An Med 29 (2014) 1–5 Topical review Canine Thoracic Costovertebral and Costotransverse Joints: Three Case Reports of Dysfunction and Manual Therapy Guidelines for Assessment and Treatment of These Structures Laurie Edge-Hughes, BScPT, MAnimSt (Animal Physiotherapy), CAFCI, CCRTn Keywords: The costovertebral and costotransverse joints receive little attention in research. However, pain costovertebral associated with rib articulation dysfunction is reported to occur in human patients. The anatomic costotransverse structures of the canine rib joints and thoracic spine are similar to those of humans. As such, it is ribs physical therapy proposed that extrapolation from human physical therapy practice could be used for the assessment and rehabilitation treatment of the canine patient with presumed rib joint pain. This article presents 3 case studies that manual therapy demonstrate signs of rib dysfunction and successful treatment using primarily physical therapy manual techniques. General assessment and select treatment techniques are described. & 2014 Elsevier Inc. All rights reserved. The Canine Fitness Centre Ltd, Calgary, Alberta, Canada nAddress reprint requests to Laurie Edge-Hughes, BScPT, MAnimSt (Animal Physiotherapy), CAFCI, CCRT, The Canine Fitness Centre Ltd, 509—42nd Ave SE, Calgary, Alberta, Canada T2G 1Y7 E-mail: [email protected] The articular structures of the thorax comprise facet joints, the erect spine and further presented that in reviewing the literature, intervertebral disc, and costal joints. Little research has been they were unable to find mention of natural development of conducted on these joints in human or animal medicine. However, idiopathic scoliosis in quadrupeds; however, there are reports of clinical case presentations in human journals, manual therapy avian models and adolescent models in man. -
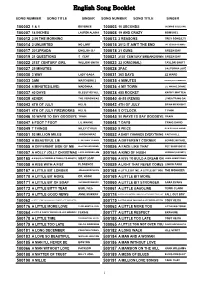
English Song Booklet
English Song Booklet SONG NUMBER SONG TITLE SINGER SONG NUMBER SONG TITLE SINGER 100002 1 & 1 BEYONCE 100003 10 SECONDS JAZMINE SULLIVAN 100007 18 INCHES LAUREN ALAINA 100008 19 AND CRAZY BOMSHEL 100012 2 IN THE MORNING 100013 2 REASONS TREY SONGZ,TI 100014 2 UNLIMITED NO LIMIT 100015 2012 IT AIN'T THE END JAY SEAN,NICKI MINAJ 100017 2012PRADA ENGLISH DJ 100018 21 GUNS GREEN DAY 100019 21 QUESTIONS 5 CENT 100021 21ST CENTURY BREAKDOWN GREEN DAY 100022 21ST CENTURY GIRL WILLOW SMITH 100023 22 (ORIGINAL) TAYLOR SWIFT 100027 25 MINUTES 100028 2PAC CALIFORNIA LOVE 100030 3 WAY LADY GAGA 100031 365 DAYS ZZ WARD 100033 3AM MATCHBOX 2 100035 4 MINUTES MADONNA,JUSTIN TIMBERLAKE 100034 4 MINUTES(LIVE) MADONNA 100036 4 MY TOWN LIL WAYNE,DRAKE 100037 40 DAYS BLESSTHEFALL 100038 455 ROCKET KATHY MATTEA 100039 4EVER THE VERONICAS 100040 4H55 (REMIX) LYNDA TRANG DAI 100043 4TH OF JULY KELIS 100042 4TH OF JULY BRIAN MCKNIGHT 100041 4TH OF JULY FIREWORKS KELIS 100044 5 O'CLOCK T PAIN 100046 50 WAYS TO SAY GOODBYE TRAIN 100045 50 WAYS TO SAY GOODBYE TRAIN 100047 6 FOOT 7 FOOT LIL WAYNE 100048 7 DAYS CRAIG DAVID 100049 7 THINGS MILEY CYRUS 100050 9 PIECE RICK ROSS,LIL WAYNE 100051 93 MILLION MILES JASON MRAZ 100052 A BABY CHANGES EVERYTHING FAITH HILL 100053 A BEAUTIFUL LIE 3 SECONDS TO MARS 100054 A DIFFERENT CORNER GEORGE MICHAEL 100055 A DIFFERENT SIDE OF ME ALLSTAR WEEKEND 100056 A FACE LIKE THAT PET SHOP BOYS 100057 A HOLLY JOLLY CHRISTMAS LADY ANTEBELLUM 500164 A KIND OF HUSH HERMAN'S HERMITS 500165 A KISS IS A TERRIBLE THING (TO WASTE) MEAT LOAF 500166 A KISS TO BUILD A DREAM ON LOUIS ARMSTRONG 100058 A KISS WITH A FIST FLORENCE 100059 A LIGHT THAT NEVER COMES LINKIN PARK 500167 A LITTLE BIT LONGER JONAS BROTHERS 500168 A LITTLE BIT ME, A LITTLE BIT YOU THE MONKEES 500170 A LITTLE BIT MORE DR. -
Read an Excerpt
Excerpt Terms & Conditions This excerpt is available to assist you in the play selection process. You may view, print and download any of our excerpts for perusal purposes. Excerpts are not intended for performance, classroom or other academic use. In any of these cases you will need to purchase playbooks via our website or by phone, fax or mail. A short excerpt is not always indicative of the entire work, and we strongly suggest reading the whole play before planning a production or ordering a cast quantity of scripts. Family Plays THE HAPPY SCARECROW Drama by I.E. Clark © Family Plays THE HAPPY SCARECROW “Thank you for The Happy Scarecrow. Never have I directed a play quite like it. The cast loved it. At District Festival we received the superior rating and everybody raved and asked, ‘Where did you get that play?’” (Marion, Va.) “My small Sunday school class has agreed to put on The Happy Scarecrow for our family night ... I have used your play a couple of times in the past and still think it is fun to do.” (Jo Smith, Faith United Methodist Church, Austin, Texas) Drama. By I.E. Clark. Cast: 6m., 5w. A mean witch dares a frilly little fairy to prove there’s such a thing as happiness. So the fairy brings a scarecrow to life and promises to make him a real man if he can find happiness. It’s a strange search, sometimes comical, sometimes sad. The scarecrow meets a variety of characters, each providing an insight into human relations as well as excellent roles for your actors and actresses. -
Angry, for the Way I Have Treated Myself
Meet Sam Literary Magazine Staff Members & Editorial/Advertising Policy Anabel Hjellen Editor-in-Chief Suben Hwang Associate Editors-in-Chief Natasha Britt Entertainment Editor Juan Gomez Chyanne Chambers Yaneli Cortes Paul Cummings Jada Jackson Shahed-Fatim Aisheh Staff Writers Kyle LoJacono Advisor Contents By Suben Hwang ........................................................................................................................................... 4 By Juan Gomez .............................................................................................................................................. 8 By Shahed-Fatim Aisheh ............................................................................................................................. 12 By Anabel Hjellen-Diaz ................................................................................................................................ 16 By Chyanne Chambers ................................................................................................................................ 22 By Jada Jackson ........................................................................................................................................... 29 By Paul Cummings ....................................................................................................................................... 38 By Natasha Britt .......................................................................................................................................... 48 By -

Friday Worship Services
WEST VIRGINIA CONFERENCE WORSHIP BOOK 2017 Annual Conference Session The Lord added daily to the community those who were being saved. (Acts 2:47) June 8-11, 2017 West Virginia Wesleyan College Sandra Steiner Ball, Residing Bishop Memorial Service Friday, June 9, 2017 ❖ 11:00 am † signifies that all are invited to stand as are able Acts 2:44-45 - All the believers were united and shared everything. They would sell pieces of property and possessions and distribute the proceeds to everyone who needed them. BELLS CALLING US TO WORSHIP GATHERING MUSIC "If You Will Only Let God Guide You" by Matt Limbaugh †GREETING Praise be to the God and Father of our Lord Jesus Christ, whose great mercy gave us new birth into a living hope by the resurrection of Jesus Christ from the dead! The inheritance to which we are born is one that nothing can destroy or spoil or wither. †LIGHTING OF THE PASCHAL CANDLE (responsive) By your cross, you destroyed the curse of the tree. By your burial, you slayed the dominion of death. By your rising, you enlightened the human race. O benefactor, Christ our God, glory to you. †OPENING PRAYER (unison) God of compassion and hope, we remember those saints who have finished their race and received their reward. As we worship you, rekindle within us the hope of the resurrection and the promise of eternal life. We know Christ’s presence abides with us in life and in death. Help us to live in constant awareness of that presence. Bless us with your Spirit, as we offer you our praise. -

Mary J Blige No More Drama Album Download Zip
1 / 5 Mary J Blige No More Drama Album Download Zip Dec 26, 2018 — Mary J. Blige Growing Pains album download ZIP 208 2007 - R&B, ... No More Drama is the fifth studio album by American R&B recording artist .... Si no Los archivos disponibles en este blog están sujetos a la ley de ... Mary J Blige Discography 320 10 Albums R B by dragan09 rar. ... Joel's first greatest hits compilation, which compiles the majority of his most ... For Tomorrow We Die 4:16 2. d384263321 Download Kendrick Lamar discography free rar zip album cds .... In addition, you can search the most popular songs, new releases, and songs from ... like to download the music more often and with something that is user friendly. ... a significant album from the past, and any record not in our archives is eligible. ... help folks like Heavy D. and Mary J. Blige get off the ground and discovered .... Скачать Mary J. Blige - No More Drama mp3 release album free and without registration. On this page you can listen to mp3 music free or download album or mp3 track to your PC, phone or tablet. ... Find music audio mp3 or zip. mp3 or zip.. Shop for Vinyl, CDs and more from Mary J. Blige at the Discogs Marketplace. ... In November 2010, Billboard Magazine ranked Blige as the most successful female ... Remix album art ... 112 616-2, Mary J. Blige - No More Drama album art .... Aug 26, 2018 — Following the commercial success of 2001's No More Drama, Blige's Love & Life came at a time in her professional and personal life where she ... -

The Most Holy Body & Blood of Christ June 18, 2017
Cardinal Blasé J. Cupich THE MOST HOLY BODY Archbishop of Chicago & BLOOD OF CHRIST Most Reverend Andrew Peter Wypych JUNE 18, 2017 Auxiliary Bishop of Chicago St. Christopher Parish Information Parish Office— 708-388-8190 4130 W. 147th Street—Midlothian, Il 60445 Fax 708-388-0072 E-Mail: [email protected] Web Site: www.stchristopherparish.com Parish Office Hours Monday—Thursday 9:00AM—7:00PM Friday 9:00AM—4:00PM Saturday 9:00AM—1:00PM Sunday 9:00AM—1:00PM Parish Staff Fr. Kris Paluch, Pastor Deacon Joseph Brady, Retired Deacon Michael Smith Denise Blackstone, Business Manager Phil & Amy Switalski, Music Ministry Directors MASS SCHEDULE John McNichols, Youth Ministry Coordinator Youth Ministry Web Site: stchristopherym.com Monday thru Saturday 8:30AM Parish Secretaries Saturday: 5:30PM (Vigil) Patricia Powers—Bulletin Editor Barbara Novick Sunday: 7:30, 9:30, 11:00AM St. Christopher School—708-385-8776 Holy Days: Check Bulletin Calendar for time 14611 S. Keeler—Midlothian, Il 60445 Fax: 708-385-8102-Web Site: www.stchrisschool.org ROSARY School E-Mail address: [email protected] The Rosary is prayed after 8:30AM Mass every morning Carol Pretkelis, Administrator Monday through Saturday. Julieanne Krahn, School Secretary EUCHARISTIC ADORATION Religious Education—708-388-4040 Monday—Saturday 7:25—8:25AM 14611 S. Keeler—Rm 21 of the School Religious Ed Web Site: www.stchrisre.com SACRAMENT OF RECONCILIATION Reconciliation Room at Front West Vestibule or by St. Christopher Ministers of Care will bring Communion appointment at the Parish Office to the hospitalized and homebound. If you, a family Saturdays: 4:00—5:00PM member or a friend is in need of a visit, please contact the Parish Office at 708-388-8190. -

4920 10 Cc D22-01 2Pac D43-01 50 Cent 4877 Abba 4574 Abba
ALDEBARAN KARAOKE Catálogo de Músicas - Por ordem de INTÉRPRETE Código INTÉRPRETE MÚSICA TRECHO DA MÚSICA 4920 10 CC I´M NOT IN LOVE I´m not in love so don´t forget it 19807 10000 MANIACS MORE THAN THIS I could feel at the time there was no way of D22-01 2PAC DEAR MAMA You are appreciated. When I was young 9033 3 DOORS DOWN HERE WITHOUT YOU A hundred days had made me older 2578 4 NON BLONDES SPACEMAN Starry night bring me down 9072 4 NON BLONDES WHAT´S UP Twenty-five years and my life is still D36-01 5 SECONDS OF SUMMER AMNESIA I drove by all the places we used to hang out D36-02 5 SECONDS OF SUMMER HEARTBREAK GIRL You called me up, it´s like a broken record D36-03 5 SECONDS OF SUMMER JET BLACK HEART Everybody´s got their demons even wide D36-04 5 SECONDS OF SUMMER SHE LOOKS SO PERFECT Simmer down, simmer down, they say we D43-01 50 CENT IN DA CLUB Go, go, go, go, shawty, it´s your birthday D54-01 A FLOCK OF SEAGULLS I RAN I walk along the avenue, I never thought I´d D35-40 A TASTE OF HONEY BOOGIE OOGIE OOGIE If you´re thinkin´ you´re too cool to boogie D22-02 A TASTE OF HONEY SUKIYAKI It´s all because of you, I´m feeling 4970 A TEENS SUPER TROUPER Super trouper beams are gonna blind me 4877 ABBA CHIQUITITA Chiquitita tell me what´s wrong 4574 ABBA DANCING QUEEN Yeah! You can dance you can jive 19333 ABBA FERNANDO Can you hear the drums Fernando D17-01 ABBA GIMME GIMME GIMME Half past twelve and I´m watching the late show D17-02 ABBA HAPPY NEW YEAR No more champagne and the fireworks 9116 ABBA I HAVE A DREAM I have a dream a song to sing… -

The Lumbosacral Dorsal Rami of the Cat
J. Anat. (1976), 122, 3, pp. 653-662 653 With 1O figures Printed in Great Britain The lumbosacral dorsal rami of the cat NIKOLAI BOGDUK Department ofAnatomy, University ofSydney, Sydney, Australia (Accepted 2 December 1975) INTRODUCTION Several reflexes involving dorsal rami have been demonstrated in the cat (Pedersen, Blunck & Gardner, 1956; Bogduk & Munro, 1973). However, there is no adequate description in the literature of the anatomy of lumbosacral dorsal rami in this animal. The present study was therefore undertaken to provide such a description, hoping thereby to facilitate the design and interpretation of our own (Bogduk & Munro, 1973) and future research on reflexes involving lumbosacral dorsal rami, including reflexes possibly relevant to the understanding of back pain in man. These nerves are described in the present study in relation to a revised nomen- clature of the muscles in the dorsal lumbar region. Such a revision (Bogduk, 1975) was necessary because of the different nomenclatures and varied interpretations in the literature. METHODS Six laboratory cats (Felis domesticus) were embalmed with 10° formalin and studied by gross dissection. In addition, confirmatory observations were made on another 16 cats in the course of surgical procedures. Lateral branches of dorsal rami were first identified during reflexion of the skin and then during the resection of iliocostalis and longissimus lumborum. These branches were subsequently traced back to their origins from the dorsal rami, a dissecting microscope being used. The medial branches of the dorsal rami were then traced through the intertransversarii mediales into multifidus. Sinuvertebral nerves were also sought. Nerve roots were detached from the spinal cord before removing it from the vertebral canal. -

The Songs and Sonets of John Donne: an Essay on Mutability
Louisiana State University LSU Digital Commons LSU Historical Dissertations and Theses Graduate School 1967 The onS gs and Sonets of John Donne: an Essay on Mutability. Barbara Ann Maynard Louisiana State University and Agricultural & Mechanical College Follow this and additional works at: https://digitalcommons.lsu.edu/gradschool_disstheses Recommended Citation Maynard, Barbara Ann, "The onS gs and Sonets of John Donne: an Essay on Mutability." (1967). LSU Historical Dissertations and Theses. 1304. https://digitalcommons.lsu.edu/gradschool_disstheses/1304 This Dissertation is brought to you for free and open access by the Graduate School at LSU Digital Commons. It has been accepted for inclusion in LSU Historical Dissertations and Theses by an authorized administrator of LSU Digital Commons. For more information, please contact [email protected]. This dissertation has been microfilmed exactly as received ^ 13,999 MAYNARD, Barbara Ann, 1935- THE SONGS AND SONETS OF JOHN DONNE: AN ESSAY ON MUTABILITY. Louisiana State University and Agricultural and Mechanical College, Ph.D., 1967 Language and Literature, general Please note: Name in vita is Barbara Kehoe Maynard. University Microfilms, Inc., Ann Arbor, Michigan THE SONGS AND SONETS OF JOHN DONNE: AN ESSAY ON MUTABILITY A Dissertation Submitted to the Graduate Faculty of the Louisiana State University and Agricultural and Mechanical College in partial fulfillment of the requirements for the degree of Doctor of Philosophy in The Department of English by Barbara Ann Maynard M.A., Louisiana State University, 1959 May, 1967 FOREWORD The number of poems included in the Songs and Sonets varies from editor to editor; accurate dating of the poems is impossible.