Therapeutic Advances in Oncology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The TP53 Apoptotic Network Is a Primary Mediator of Resistance to BCL2 Inhibition in AML Cells
Published OnlineFirst May 2, 2019; DOI: 10.1158/2159-8290.CD-19-0125 RESEARCH ARTICLE The TP53 Apoptotic Network Is a Primary Mediator of Resistance to BCL2 Inhibition in AML Cells Tamilla Nechiporuk1,2, Stephen E. Kurtz1,2, Olga Nikolova2,3, Tingting Liu1,2, Courtney L. Jones4, Angelo D’Alessandro5, Rachel Culp-Hill5, Amanda d’Almeida1,2, Sunil K. Joshi1,2, Mara Rosenberg1,2, Cristina E. Tognon1,2,6, Alexey V. Danilov1,2, Brian J. Druker1,2,6, Bill H. Chang2,7, Shannon K. McWeeney2,8, and Jeffrey W. Tyner1,2,9 ABSTRACT To study mechanisms underlying resistance to the BCL2 inhibitor venetoclax in acute myeloid leukemia (AML), we used a genome-wide CRISPR/Cas9 screen to identify gene knockouts resulting in drug resistance. We validated TP53, BAX, and PMAIP1 as genes whose inactivation results in venetoclax resistance in AML cell lines. Resistance to venetoclax resulted from an inability to execute apoptosis driven by BAX loss, decreased expression of BCL2, and/or reliance on alternative BCL2 family members such as BCL2L1. The resistance was accompanied by changes in mitochondrial homeostasis and cellular metabolism. Evaluation of TP53 knockout cells for sensitivities to a panel of small-molecule inhibitors revealed a gain of sensitivity to TRK inhibitors. We relate these observations to patient drug responses and gene expression in the Beat AML dataset. Our results implicate TP53, the apoptotic network, and mitochondrial functionality as drivers of venetoclax response in AML and suggest strategies to overcome resistance. SIGNIFICANCE: AML is challenging to treat due to its heterogeneity, and single-agent therapies have universally failed, prompting a need for innovative drug combinations. -

Duvelisib Eliminates CLL B Cells, Impairs CLL- Supporting Cells, and Overcomes Ibrutinib Resistance in Preclinical Models
Duvelisib Eliminates CLL B Cells, Impairs CLL- Supporting Cells, and Overcomes Ibrutinib Resistance in Preclinical Models Shih-Shih Chen ( [email protected] ) Karches Center for Oncology Research, the Feinstein Institutes for Medical Research Jacqueline Barrientos Karches Center for Oncology Research, the Feinstein Institutes for Medical Research Gerardo Ferrer Josep Carreras Leukaemia Research Institute (IJC) https://orcid.org/0000-0002-4084-6815 Priyadarshini Ravichandran Karches Center for Oncology Research, the Feinstein Institutes for Medical Research Michael Ibrahim Karches Center for Oncology Research, the Feinstein Institutes for Medical Research Yasmine Kieso Karches Center for Oncology Research, the Feinstein Institutes for Medical Research Jeff Kutok Innity Pharmaceuticals Marisa Peluso Innity Pharmaceuticals, Inc Sujata Sharma Innity Pharmaceuticals, Inc David Weaver Institute of Health Sciences, Anhui University Jonathan Pachter Verastem Inc. Kanti Rai The Karches Center for Oncology Research. The Feinstein Institutes for Medical Research. Nicholas Chiorazzi Karches Center for Oncology Research, the Feinstein Institutes for Medical Research Article Keywords: chronic lymphocytic leukemia, cancer therapy, Bruton’s Tyrosine Kinase (BTKi), phosphoinositide 3-kinase (PI3Ki) Page 1/23 Posted Date: July 21st, 2021 DOI: https://doi.org/10.21203/rs.3.rs-701669/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 2/23 Abstract Inhibitors of Bruton’s Tyrosine Kinase (BTKi) and phosphoinositide 3-kinase (PI3Ki) have signicantly improved therapy of chronic lymphocytic leukemia (CLL). However, the emergence of resistance to BTKi has introduced an unmet therapeutic need. Here we demonstrate in vitro and in vivo the essential roles of PI3K-δ for CLL B-cell survival and migration and of PI3K-γ in T-cell migration and macrophage polarization; and more ecacious inhibition in CLL-cell burden by dual inhibition of PI3K-δ,γ. -

= 'NH., Diseases, Central Nerrous System M)Ury and Different Foims of Mflannnation
(12) INTERNATIONAL APPLICATION Pl;BLISHED 1. NDER THE PATENT COOPERATION TREATY (PCT) (19) World intellectual Property Organraation llIlllIlllIlIllllllllIlllllIIllIllIlllIlllllllllllIlllIllIlIlllIllIlIllIllIlIIIIIIIIIIIIIIIIIII International Bureau (10) International Publication Number (43) International Publication Date WO 2020/114892 Al 11 June 2020 (11.06.2020) W 4 P Gl I P 0 T (51) International Patent Classification: C07D 401/06 (200G 0 I) AGJK31/454 (200G 0l) C07D dt)J//4 (2006 01) A61P35/ttd (200G 0l) (21) International Application Number: PCT/EP2019/l)8 3014 (22) International Filing Date: 29 Nosember 2019 (29.11.2019) (25) Filing Language: Enghsh (26) Publication Language Enghsh (30) Priority Data: 1820972/i 1 03 December 20)8 (03 12 2018) EP (71) Applicant: MERCK PATENT GMBH IDE/DE]. Frm&(s- furter Strasse 230. 64293 DARMSTADT (DE) (72) Inventors: BUCHSTALLER, Hans-Peter. Ncc)sa&strasse G. G4347 GRIESHELVI (DE). ROHDICH, Feliru Saalbaus- tmssc 23. 64283 DARMSTADT (DE). (81) Designated States /unless i&themmse n&d&ct&md, /or e&ery hind of national protect«&n menial&le/ AF, AG, AL, AVI AO, AT. AU. AZ, BA, BB, BG, BH. B N. BR, BW, BY. BZ. CA. CH, CL, CN. CO, CR. C U, CZ. DE, DJ, DK. DM DO. DZ, EC. EE, EG. ES. FI, GB. GD. GE. GH, GM. GT. HN. HR. HU, ID, IL. IN, IR, IS. JO, JP, KE. KG, KH. KN, KP. KR. KW, KZ, LA. L C, LK. LR, LS, LU. LY. MA. MD, ME. WIG. MK. MN, MW, MX. MY. MZ. NA. NG. NI, NO. NZ. OM, PA. PE, PG. PH, PL. PT. QA, RO, RS. -

Entrectinib (Interim Monograph)
Entrectinib (interim monograph) DRUG NAME: Entrectinib SYNONYM(S): RXDX-1011, NMS-E6282 COMMON TRADE NAME(S): ROZLYTREK® CLASSIFICATION: molecular targeted therapy Special pediatric considerations are noted when applicable, otherwise adult provisions apply. MECHANISM OF ACTION: Entrectinib is an orally administered, small molecule, multi-target tyrosine kinase inhibitor which targets tropomyosin- related kinase (Trk) proteins TrkA, TrkB, and TrkC, proto-oncogene tyrosine-protein kinase ROS (ROS1) and anaplastic lymphoma kinase (ALK). TrkA, TrkB, and TrkC are receptor tyrosine kinases encoded by the neurotrophic tyrosine receptor kinase (NTRK) genes NTRK1, NTRK2, and NTRK3, respectively. Fusion proteins that include Trk, ROS1, or ALK kinase domains drive tumorigenic potential through hyperactivation of downstream signalling pathways leading to unconstrained cell proliferation. By potently inhibiting the Trk kinases, ROS1, and ALK, entrectinib inhibits downstream signalling pathways, cell proliferation and induces tumour cell apoptosis.3-5 PHARMACOKINETICS: Oral Absorption bioavailability = 55%; Tmax = 4-6 hours; Tmax delayed 2 h by high-fat, high-calorie food intake Distribution highly bound to human plasma proteins cross blood brain barrier? yes volume of distribution 551 L (entrectinib); 81.1 L (M5) plasma protein binding >99% (entrectinib and M5) Metabolism primarily metabolized by CYP 3A4 active metabolite(s) M5 inactive metabolite(s) M11 Excretion primarily via hepatic clearance urine 3.06% feces 82.9% (36% as unchanged entrectinib, 22% as M5) terminal half life 20 h (entrectinib); 40 h (M5) clearance 19.6 L/h (entrectinib); 52.4 L/h (M5) Elderly no clinically significant difference Children comparable pharmacokinetics of entrectinib and M5 in adults and children Ethnicity no clinically significant difference Adapted from standard reference3,4 unless specified otherwise. -

Tumour-Agnostic Therapy for Pancreatic Cancer and Biliary Tract Cancer
diagnostics Review Tumour-Agnostic Therapy for Pancreatic Cancer and Biliary Tract Cancer Shunsuke Kato Department of Clinical Oncology, Juntendo University Graduate School of Medicine, 2-1-1, Hongo, Bunkyo-ku, Tokyo 113-8421, Japan; [email protected]; Tel.: +81-3-5802-1543 Abstract: The prognosis of patients with solid tumours has remarkably improved with the develop- ment of molecular-targeted drugs and immune checkpoint inhibitors. However, the improvements in the prognosis of pancreatic cancer and biliary tract cancer is delayed compared to other carcinomas, and the 5-year survival rates of distal-stage disease are approximately 10 and 20%, respectively. How- ever, a comprehensive analysis of tumour cells using The Cancer Genome Atlas (TCGA) project has led to the identification of various driver mutations. Evidently, few mutations exist across organs, and basket trials targeting driver mutations regardless of the primary organ are being actively conducted. Such basket trials not only focus on the gate keeper-type oncogene mutations, such as HER2 and BRAF, but also focus on the caretaker-type tumour suppressor genes, such as BRCA1/2, mismatch repair-related genes, which cause hereditary cancer syndrome. As oncogene panel testing is a vital approach in routine practice, clinicians should devise a strategy for improved understanding of the cancer genome. Here, the gene mutation profiles of pancreatic cancer and biliary tract cancer have been outlined and the current status of tumour-agnostic therapy in these cancers has been reported. Keywords: pancreatic cancer; biliary tract cancer; targeted therapy; solid tumours; driver mutations; agonist therapy Citation: Kato, S. Tumour-Agnostic Therapy for Pancreatic Cancer and 1. -

Minutes of the CHMP Meeting 14-17 September 2020
13 January 2021 EMA/CHMP/625456/2020 Corr.1 Human Medicines Division Committee for medicinal products for human use (CHMP) Minutes for the meeting on 14-17 September 2020 Chair: Harald Enzmann – Vice-Chair: Bruno Sepodes Disclaimers Some of the information contained in these minutes is considered commercially confidential or sensitive and therefore not disclosed. With regard to intended therapeutic indications or procedure scopes listed against products, it must be noted that these may not reflect the full wording proposed by applicants and may also vary during the course of the review. Additional details on some of these procedures will be published in the CHMP meeting highlights once the procedures are finalised and start of referrals will also be available. Of note, these minutes are a working document primarily designed for CHMP members and the work the Committee undertakes. Note on access to documents Some documents mentioned in the minutes cannot be released at present following a request for access to documents within the framework of Regulation (EC) No 1049/2001 as they are subject to on- going procedures for which a final decision has not yet been adopted. They will become public when adopted or considered public according to the principles stated in the Agency policy on access to documents (EMA/127362/2006). 1 Addition of the list of participants Official address Domenico Scarlattilaan 6 ● 1083 HS Amsterdam ● The Netherlands Address for visits and deliveries Refer to www.ema.europa.eu/how-to-find-us Send us a question Go to www.ema.europa.eu/contact Telephone +31 (0)88 781 6000 An agency of the European Union © European Medicines Agency, 2020. -

Proteomics and Drug Repurposing in CLL Towards Precision Medicine
cancers Review Proteomics and Drug Repurposing in CLL towards Precision Medicine Dimitra Mavridou 1,2,3, Konstantina Psatha 1,2,3,4,* and Michalis Aivaliotis 1,2,3,4,* 1 Laboratory of Biochemistry, School of Medicine, Faculty of Health Sciences, Aristotle University of Thessaloniki, GR-54124 Thessaloniki, Greece; [email protected] 2 Functional Proteomics and Systems Biology (FunPATh)—Center for Interdisciplinary Research and Innovation (CIRI-AUTH), GR-57001 Thessaloniki, Greece 3 Basic and Translational Research Unit, Special Unit for Biomedical Research and Education, School of Medicine, Aristotle University of Thessaloniki, GR-54124 Thessaloniki, Greece 4 Institute of Molecular Biology and Biotechnology, Foundation of Research and Technology, GR-70013 Heraklion, Greece * Correspondence: [email protected] (K.P.); [email protected] (M.A.) Simple Summary: Despite continued efforts, the current status of knowledge in CLL molecular pathobiology, diagnosis, prognosis and treatment remains elusive and imprecise. Proteomics ap- proaches combined with advanced bioinformatics and drug repurposing promise to shed light on the complex proteome heterogeneity of CLL patients and mitigate, improve, or even eliminate the knowledge stagnation. In relation to this concept, this review presents a brief overview of all the available proteomics and drug repurposing studies in CLL and suggests the way such studies can be exploited to find effective therapeutic options combined with drug repurposing strategies to adopt and accost a more “precision medicine” spectrum. Citation: Mavridou, D.; Psatha, K.; Abstract: CLL is a hematological malignancy considered as the most frequent lymphoproliferative Aivaliotis, M. Proteomics and Drug disease in the western world. It is characterized by high molecular heterogeneity and despite the Repurposing in CLL towards available therapeutic options, there are many patient subgroups showing the insufficient effectiveness Precision Medicine. -
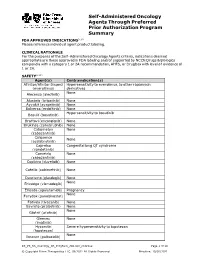
PRIOR AUTHORIZATION CRITERIA for APPROVAL Initial Evaluation Target Agent(S) Will Be Approved When ONE of the Following Is Met: 1
Self-Administered Oncology Agents Through Preferred Prior Authorization Program Summary FDA APPROVED INDICATIONS3-104 Please reference individual agent product labeling. CLINICAL RATIONALE For the purposes of the Self -Administered Oncology Agents criteria, indications deemed appropriate are those approved in FDA labeling and/or supported by NCCN Drugs & Biologics compendia with a category 1 or 2A recommendation, AHFS, or DrugDex with level of evidence of 1 or 2A. SAFETY3-104 Agent(s) Contraindication(s) Afinitor/Afinitor Disperz Hypersensitivity to everolimus, to other rapamycin (everolimus) derivatives None Alecensa (alectinib) Alunbrig (brigatinib) None Ayvakit (avapritinib) None Balversa (erdafitinib) None Hypersensitivity to bosutinib Bosulif (bosutinib) Braftovi (encorafenib) None Brukinsa (zanubrutinib) None Cabometyx None (cabozantinib) Calquence None (acalabrutinib) Caprelsa Congenital long QT syndrome (vandetanib) Cometriq None (cabozantinib) Copiktra (duvelisib) None Cotellic (cobimetinib) None Daurismo (glasdegib) None None Erivedge (vismodegib) Erleada (apalutamide) Pregnancy None Farydak (panobinostat) Fotivda (tivozanib) None Gavreto (pralsetinib) None None Gilotrif (afatinib) Gleevec None (imatinib) Hycamtin Severe hypersensitivity to topotecan (topotecan) None Ibrance (palbociclib) KS_PS_SA_Oncology_PA_ProgSum_AR1020_r0821v2 Page 1 of 19 © Copyright Prime Therapeutics LLC. 08/2021 All Rights Reserved Effective: 10/01/2021 Agent(s) Contraindication(s) None Iclusig (ponatinib) Idhifa (enasidenib) None Imbruvica (ibrutinib) -

1 Activity of the Second Generation BTK Inhibitor Acalabrutinib In
Activity of the Second Generation BTK Inhibitor Acalabrutinib in Canine and Human B-cell Non-Hodgkin Lymphoma Dissertation Presented in Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in the Graduate School of The Ohio State University By Bonnie Kate Harrington Graduate Program in Comparative and Veterinary Medicine The Ohio State University 2018 Dissertation Committee John C. Byrd, M.D., Advisor Amy J. Johnson, Ph.D. Krista La Perle, D.V.M., Ph.D. William C. Kisseberth, D.V.M., Ph.D. 1 Copyrighted by Bonnie Kate Harrington 2018 2 Abstract Acalabrutinib (ACP-196) is a second-generation inhibitor of Bruton’s Tyrosine Kinase (BTK) with increased target selectivity and potency compared to ibrutinib. In these studies, we evaluated acalabrutinib in spontaneously occurring canine lymphoma, a model of B-cell malignancy reported to be similar to human diffuse large B-cell lymphoma (DLBCL), as well as primary human chronic lymphocytic leukemia (CLL) cells. We demonstrated that acalabrutinib potently inhibited BTK activity and downstream B-cell receptor (BCR) effectors in CLBL1, a canine B-cell lymphoma cell line, primary canine lymphoma cells, and primary CLL cells. Compared to ibrutinib, acalabrutinib is a more specific inhibitor and lacked off-target effects on the T-cell and NK cell kinase IL-2 inducible T-cell kinase (ITK) and epidermal growth factor receptor (EGFR). Accordingly, acalabrutinib did not antagonize antibody dependent cell cytotoxicity mediated by NK cells. Finally, acalabrutinib inhibited proliferation and viability in CLBL1 cells and primary CLL cells and abrogated chemotactic migration in primary CLL cells. To support our in vitro findings, we conducted a clinical trial using companion dogs with spontaneously occurring B-cell lymphoma. -

07052020 MR ASCO20 Curtain Raiser
Media Release New data at the ASCO20 Virtual Scientific Program reflects Roche’s commitment to accelerating progress in cancer care First clinical data from tiragolumab, Roche’s novel anti-TIGIT cancer immunotherapy, in combination with Tecentriq® (atezolizumab) in patients with PD-L1-positive metastatic non- small cell lung cancer (NSCLC) Updated overall survival data for Alecensa® (alectinib), in people living with anaplastic lymphoma kinase (ALK)-positive metastatic NSCLC Key highlights to be shared on Roche’s ASCO virtual newsroom, 29 May 2020, 08:00 CEST Basel, 7 May 2020 - Roche (SIX: RO, ROG; OTCQX: RHHBY) today announced that new data from clinical trials of 19 approved and investigational medicines across 21 cancer types, will be presented at the ASCO20 Virtual Scientific Program organised by the American Society of Clinical Oncology (ASCO), which will be held 29-31 May, 2020. A total of 120 abstracts that include a Roche medicine will be presented at this year's meeting. "At ASCO, we will present new data from many investigational and approved medicines across our broad oncology portfolio," said Levi Garraway, M.D., Ph.D., Roche's Chief Medical Officer and Head of Global Product Development. “These efforts exemplify our long-standing commitment to improving outcomes for people with cancer, even during these unprecedented times. By integrating our medicines and diagnostics together with advanced insights and novel platforms, Roche is uniquely positioned to deliver the healthcare solutions of the future." Together with its partners, Roche is pioneering a comprehensive approach to cancer care, combining new diagnostics and treatments with innovative, integrated data and access solutions for approved medicines that will both personalise and transform the outcomes of people affected by this deadly disease. -

A Novel Mechanism of Crizotinib Resistance in a ROS1+ NSCLC Patient 11 April 2016
A novel mechanism of crizotinib resistance in a ROS1+ NSCLC patient 11 April 2016 Molecular analysis of a tumor biopsy from a proto- fusion gene in the crizotinib resistant tumor samples oncogene 1 receptor tyrosine kinase positive compared to the pretreatment tumor samples by (ROS1+) patient with acquired crizotinib resistance DNA sequencing or FISH analysis. SNaPshot revealed a novel mutation in the v-kit Hardy analysis of the crizotinib resistant tumor identified a Zuckerman 4 feline sarcoma viral oncogene novel mutation in the KIT gene encoding the amino homolog receptor tyrosine kinase (KIT) that can acid substitution, pD816G. The drug ponatinib, a potentially be targeted by KIT inhibitors. KIT tyrosine kinase inhibitor, demonstrated inhibition of KITD816G kinase activity. Further, in Chromosomal rearrangements of the gene ROS1+ cells expressing KITD816G the addition of encoding ROS1 in approximately 1-2% of non- ponatinib resensitized cells to crizotinib. small cell lung cancers (NSCLC). Treatment of ROS1+ patients with crizotinib, a small-molecule The authors comment that, "Although our results tyrosine kinase inhibitor, often results in durable demonstrate that ponatinib can overcome KIT- tumor regression. However, despite initial mediated resistance in vitro, it remains unknown treatment success patients typically develop whether ponatinib can overcome this or other KIT resistance to crizotinib and disease progression activating mutations in patients. Detection of KIT inevitably ensues. Understanding the mechanism mutations may allow enrollment of patients with of resistance to crizotinib and identifying new ROS1+ cancer (or other oncogenes), onto clinical targets for therapy will help guide patient trials of KIT inhibitors, however it is likely that dual treatment. -
Management of Multiple Myeloma: the Changing Paradigm
Management of Multiple Myeloma: The Changing Paradigm Relapsed/Refractory Disease Jeffrey A. Zonder, MD Karmanos Cancer Institute Objectives • Discuss use of standard myeloma therapies when used as therapy after relapse • Consider patient and disease factors which might impact therapy decisions. • Describe off-label options for patients who are not protocol candidates. Line ≠ Line ≠ Line ≠ … POLICE LINE – DO NOT CROSS POLICE LINE – DO NOT CROSS POLICE LINE – DO NOT CROSS POLICE LINE – DO NOT CROSS POLI LINE – DO NOT Define “Line” • A pre-defined course of therapy utilizing agents either simultaneously or sequentially – Len/Dex – Len/Dex ASCT – Vel/Dex ASCT Len/Dex – VDT-PACE ASCT TD ASCT VPT-PACE LD • Pts who have had the same # of “lines” of Rx may have had vastly different amounts of Rx What Is Relapsed/Refractory Disease? • Relapsed: recurrence after a response to therapy • Refractory: progression despite ongoing therapy What Do We Know About the Pt’s Myeloma? • What prior therapy has been used? • How well did it work? • Did the myeloma progress on active therapy? • High-risk cytogenetics/FISH/GEP? What Do We Know About the Patient? • Age • Other medical problems – Diabetes – Blood Clots • Lasting side effects from past therapies – Peripheral Neuropathy • Personal preferences and values Choosing Therapy for Relapsed/Refractory Myeloma Proteasome IMiDs Anthracyclines Alkylators Steroids HDACs Antibodies Inhibitors Thalidomide Bortezomib Doxil Melphalan Dex Panobinostat Elotuzumab Lenalidomide Carfilzomib Cytoxan Pred Vorinostat