Modulation of the Autophagy-Lysosomal Pathway in Hepatocellular Carcinoma Using Small Molecules
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Preventive and Therapeutic Effects of Chinese Herbal Compounds Against Hepatocellular Carcinoma
molecules Review Preventive and Therapeutic Effects of Chinese Herbal Compounds against Hepatocellular Carcinoma Bing Hu 1,*, Hong-Mei An 2, Shuang-Shuang Wang 1, Jin-Jun Chen 3 and Ling Xu 1 1 Department of Oncology and Institute of Traditional Chinese Medicine in Oncology, Longhua Hospital, Shanghai University of Traditional Chinese Medicine, Shanghai 200032, China; [email protected] (S.-S.W.); [email protected] (L.X.) 2 Department of Science & Technology, Longhua Hospital, Shanghai University of Traditional Chinese Medicine, Shanghai 202032, China; [email protected] 3 Department of Plastic & Reconstructive Surgery, Shanghai Key Laboratory of Tissue Engineering, The Ninth People’s Hospital, School of Medicine, Shanghai Jiaotong University, Shanghai 200011, China; [email protected] * Correspondence: [email protected]; Tel.: +86-21-64385700 Academic Editor: Derek J. McPhee Received: 16 November 2015 ; Accepted: 20 January 2016 ; Published: 27 January 2016 Abstract: Traditional Chinese Medicines, unique biomedical and pharmaceutical resources, have been widely used for hepatocellular carcinoma (HCC) prevention and treatment. Accumulated Chinese herb-derived compounds with significant anti-cancer effects against HCC have been identified. Chinese herbal compounds are effective in preventing carcinogenesis, inhibiting cell proliferation, arresting cell cycle, inducing apoptosis, autophagy, cell senescence and anoikis, inhibiting epithelial-mesenchymal transition, metastasis and angiogenesis, regulating immune function, reversing drug -

Pharmaceutical Sciences
JOURNAL OF Pharmaceutical Sciences December 1967 volume 56, number 12 ___ Review Article __ Pharmacology and Toxicology of Toad Venom By K. K. CHEN and ALENA KOVARiKOVA CONTENTS speare made the witch throw a toad into the hell-broth. It has been long believed that han- HISTORY.. 1535 dling of toads causes warts. In a small area of CHEMICALINGREDIEXTSOF TOADPOISOX. 1536 Pharmacology of Bufadienolides. 1536 the state of Illinois, folklore has 300 references Bufagins. .... 1536 to warts of toad origin, particularly their cures (2). Bufotoxins. ... .. .. 1538 These superstitions can of course be disproved Clinical Trials... .... 1539 by laboratory experience. Houssay (3) op- Catecholamines. .. .. 1539 Epinephrine.. .. .. .. 1539 erated on 15,000 toads for endocrine studies and Norephinephrine.. .. .. .. .. 1539 we handled more than 10,000 toads for the Indolealkylamines..... 1539 collection of their poisons-with no ill effects. Noncardiotonic Sterols. .. 1540 In form of a votive animal, the toad is associated Cholesterol. ... .. .. ... .. .. 1540 with the uterus and various gynecological dis- Provitamin D. .. .. 1540 -v-Sitosterol .......... ... .. .. 1540 eases (4) in Central Europe. Bronze toads of Miscellaneous Substances.. 1540 the Perm culture of Kortheastern Russia were USE OF THE VENOMTO THE TOAD. 1540 among the archaeological findings dating from Protection from Enemies. 1540 the middle of the 1st century A.D. Significance to Behavior. 1540 ="ATURALTOLERANCETO CARDIACGLYCO- Toad medicine has been advocated all over SIDESANDAGLYCONES. 1540 the world. For many years the Chinese have RESPONSEOFOTHERTISSUESTODRUGS. 1541 used a preparation of toad venom, ch'an su, REFERENCES. 1541 for the treatment of canker sores, toothache, HISTORY sinusitis, and local inflammations (5). During the 15th century a European physician wrote a FOR CENTURIES the toad has been known to book, "De Vcnenis," in which he mentioned that produce a poisonous secretion. -

Cinobufagin, a Bufadienolide, Activates ROS-Mediated Pathways to Trigger Human Lung Cancer Cell Apoptosis in Vivo
RSC Advances View Article Online PAPER View Journal | View Issue Cinobufagin, a bufadienolide, activates ROS- mediated pathways to trigger human lung cancer Cite this: RSC Adv.,2017,7,25175 cell apoptosis in vivo† Panli Peng, ab Junhong Lv,c Changqing Cai,b Shaohuan Lin,c Enqing Zhuob and Senming Wang*a Lung cancer, as the most common malignancy worldwide, is one of the most threatening diseases for human beings. Chan Su, an ethanolic extract from skin and parotid venom glands of the Bufo bufo gargarizans Cantor, is widely used as a traditional Chinese medicine in cancer therapy. Bufadienolides are cardiotonic steroids isolated from the skin and parotid venom glands of toad Bufo bufo gargarizans Cantor with excellent anticancer activity. Unfortunately, little information about the in vivo effects and action mechanisms of bufadienolides on human lung cancer cells is available. Therefore, in this study, the anticancer activities of Cinobufagin (CnBu), bufalin (Bu) and arenobufagin (ArBu) were evaluated in Creative Commons Attribution 3.0 Unported Licence. vivo and in vitro and the underlying mechanisms were elucidated. The results showed that CnBu exhibited higher anticancer efficacy than Bu and AuBu against a panel of five lung cancer cells (A549, NCI-H460, H1299, Sk-mes-1 and Calu-3) with IC50 values ranging from 2.3–6.7 mM. Moreover, CnBu showed much higher selectivity between cancer and normal cells, as suggested by its IC50 value towards BEAS-2B human normal bronchial epithelial cells reaching 22.3 mM. CnBu also significantly inhibited the growth of A549 cells in a dose-dependent manner through anti-migration and anti-invasion. -

World Journal of Pharmaceutical Research Pradhan Et Al
World Journal of Pharmaceutical Research Pradhan et al. World Journal of Pharmaceutical SJIF ImpactResearch Factor 6.805 Volume 5, Issue 8, 426-443. Review Article ISSN 2277– 7105 ` BUFO SKIN-SECRETIONS ARE SOURCES OF PHARMACOLOGICALLY AND THERAPEUTICALLY SIGNIFICANT COMPOUNDS Dr. Bishnu Charan Pradhan*1 and Shakti Prasad Pradhan2 1Dept. of Zoology Angul Mahila Mahavidyalaya, Angul, Odisha, India. 759122. 2Dept. of Pharmacy. Utkal University, Vanivihar, Bhubaneswar, Odisha, India. ABSTRACT Article Received on 07 June 2016, Amphibians have been occupying a wide range of habitats since they Revised on 28 June 2016, evolved around 363 million-years-ago. Along with legs and lungs, skin Accepted on 18 July 2016 DOI: 10.20959/wjpr20168-6752 played an important role in survival of amphibians and made it possible for them to exploit diverse ecological conditions. Amphibian skin not only helps in avoiding desiccation but also helps in imposing *Corresponding Author Dr. Bishnu Charan defense against predators as well as pathogens. Amphibian skin Pradhan possesses wide variety of chemical compounds, which have potential Dept. of Zoology Angul significance in pharmacology and therapeutics. Toads especially those Mahila Mahavidyalaya, belonging to genus Bufo, are outstanding source of useful granular- Angul, Odisha, India. 759122. gland secretions. Compounds derived from toad skin-secretions can be used as analgesics, painkillers and as medicine against cardiac- problems, multi-drug resistant bacteria, HIV and Cancer. KEYWORDS: Bufadienolides, pharmacology, Bufo skin-secretions, toxins. INTRODUCTION Amphibians started trolling the landmasses of earth about 363 million-years-ago, with Acanthostega and Ichthyostega probably being the earliest of known amphibians (Evans[20] et al 1998). Fossil records elucidate that ancestors of modern amphibians like Frogs, Toads, Caecilians and Salamanders probably evolved about 200 million years ago during the Triassic period. -

PREPARATIVE SEPARATION and PURIFICATION of BUFADIENOLIDES from Chansu by HIGH-SPEED COUNTER-CURRENT CHROMATOGRAPHY COMBINED with PREPARATIVE HPLC
Quim. Nova, Vol. 36, No. 5, 686-690, 2013 PREPARATIVE SEPARATION AND PURIFICATION OF BUFADIENOLIDES FROM ChanSu BY HIGH-SPEED COUNTER-CURRENT CHROMATOGRAPHY COMBINED WITH PREPARATIVE HPLC Jialian Li and Yongqing Zhang College of Pharmacy, Shandong University of Traditional Chinese Medicine, Jinan, Shandong, 250355, P. R. China Yunliang Lin, Xiao Wang, Lei Fang* and Yanling Geng Artigo Shandong Analysis and Test Center, Shandong Academy of Sciences, 19 Keyuan Street, Jinan, Shandong, 250014, P. R. China Qinde Zhang Shandong College of Traditional Chinese Medicine, Laiyang, Shandong, 265200, P. R. China Recebido em 13/9/12; aceito em 6/12/12; publicado na web em 4/4/13 Eight bufadienolides were successfully isolated and purified from ChanSu by high-speed counter-current chromatography (HSCCC) combined with preparative HPLC (prep-HPLC). First, a stepwise elution mode of HSCCC with the solvent system composed of petroleum ether–ethyl acetate–methanol–water (4:6:4:6, 4:6:5:5, v/v) was employed and four bufadienolides, two partially purified fractions were obtained from 200 mg of crude extract. The partially purified fractions III and VI were then further separated by prep- HPLC, respectively, and another four bufadienolides were recovered. Their structures were confirmed by ESI-MS and 1H-NMR spectra. Keywords: high-speed counter-current chromatography; bufadienolides; preparative HPLC. INTRODUCTION pretreatment of sample and overloaded columns, caused by plentiful raw sample that could be compensated by HSCCC.13 However, few Venenum bufonis, also called ChanSu, is prepared from dried toad reports have been published on the separation and purification of secretions derived from either Bufo bufo gargarizans Cantor or Bufo bufadienolides from ChanSu by HSCCC combined with prep-HPLC. -

Toxicology Reference Laboratory
TOXICOLOGY REFERENCE LABORATORY Laboratory User Guide ROOM 708, BLOCK P PRINCESS MARGARET HOSPITAL 2-10 Princess Margaret Hospital Road Lai Chi Kok Tel: 2990 1941 Fax: 2990 1942 http://trl.home Version 6.1 Effective date: 1/July/2014 Contents Contents ..................................................................................................................................................... 2 Introduction ............................................................................................................................................... 4 Staff ............................................................................................................................................................ 5 Honorary Medical Staff .......................................................................................................................... 5 Scientific Staff ........................................................................................................................................ 5 Technical Staff ........................................................................................................................................ 5 Supportive Staff ...................................................................................................................................... 6 How to Make Laboratory Request .......................................................................................................... 7 Instruction for Referring Clinician ........................................................................................................ -
Product List Updated on 201802 Remark1: All Products Can Be Supplied from Mgs to Grams, Some of Them, up to Kgs
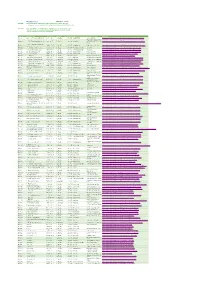
Product List Updated on 201802 Remark1: All products can be supplied from mgs to grams, some of them, up to kgs. All products are tested by HPLC-UV or/and HPLC-ELSD, purity>95%,98% or 99%. Remark2: More than 2000 natural compounds are available in this list for drug screening, many of them are our exclusive products. Most products in the list are in stock now, some of them is not in stock, but available. Catalog No English name CAS Number Formula MolWeight Type of Compound Botanical Source Web_link BP0001 1,2,3,4,6-Pentagalloylglucose 14937-32-7 C41H32O26 940.681 Polyphenols Galla chinensis http://www.phytopurify.com/12346Pentagalloylglucose-p-4024.html Swertia bimaculata (Sieb. BP0003 1,3,5,8-Tetrahydroxyxanthone 2980-32-7 C13H8O6 260.201 Xanthones et Zucc.)Hook. Thoms.ex http://www.phytopurify.com/1358Tetrahydroxyxanthone-p-4025.html Clarke 1,3,6-Tri-O-galloyl-beta-D- BP0004 18483-17-5 C H O 636.471 Polyphenols Phyllanthus emblica L. http://www.phytopurify.com/136TriOgalloylbetaDglucose-p-4894.html glucose 27 24 18 BP0005 1,3-Dicaffeoylquinic acid 30964-13-7 C25H24O12 516.455 Phenylpropanoids Inulae flos http://www.phytopurify.com/13Dicaffeoylquinicacid-p-152.html BP0006 1,5-Dicaffeoylquinic acid 19870-46-3 C25H24O12 516.455 Phenylpropanoids Inulae flos http://www.phytopurify.com/15Dicaffeoylquinicacid-p-192.html BP0011 10-deacetylbaccatin III 32981-86-5 C29H36O10 544.597 Diterpenoids Taxus chinensis http://www.phytopurify.com/10deacetylbaccatinIII-p-4026.html BP0012 10-Deacetyltaxol 78432-77-6 C45H49NO13 811.881 Diterpenoids Taxus chinensis http://www.phytopurify.com/10Deacetyltaxol-p-5353.html BP0013 10-Gingerol 23513-15-7 C21H34O4 350.499 Phenols Zingiber officinale Rose. -

Biological Activities of Nanomaterials (Bufadienolides, Peptides and Alkoloids) in the Skin of Amphibian on Gammarus Pulex L
Digest Journal of Nanomaterials and Biostructures Vol. 5, No 2, April 2010, p. 347 – 354 BIOLOGICAL ACTIVITIES OF NANOMATERIALS (BUFADIENOLIDES, PEPTIDES AND ALKOLOIDS) IN THE SKIN OF AMPHIBIAN ON GAMMARUS PULEX L. VAHDETTİN BAYAZİT* Muş Alparslan University, Faculty of Arts and Sciences, Department of Biology, 49100, Muş, Turkey, Phone The purpose of this sudy was to examine the toxic effects of bufadienolides of antimicrobial peptides and alkoloids on Gammarus pulex L.(Crustacea:Amphipoda:Gammaridae) Bufadienolides (Arenobufagin, Arenobufagin hemisuberate, Arinobufagin 3- sulfate, Bufalin, Bufalin hemisuberate, Bufoatlin 3-sulfate, Bufotalinin, Bufotalone, Cinobufagin, Cinobugagilon, Cinobufotalin, Desacetylcinobufagin, Gamabufotalin hemisuberoate, Gamabufotalin 3-sulfate, 15- hydroxybufalin, 19-hydroxybufalin, Marinobufagin, Marinoic acid, Marinosin and Resibufaginol), Amphibian peptides (Caerin 1.1, Caerin 1.9, Caerin 4.1, Dahlein 5.6, Dermaseptin, Esculentin-1ARb, Esculentin-2P, Maculatin 1.1, Magainin II, MRP, Palustrin-3AR, Ranatuerin-6, Ranatuerin-2P, Uperin 3.6, RCCP) and Alkoloids (Samandarine, Batrachotoxin, Histrionictoxin, Pumiliotoxin, Allopumiliotoxin, Homopumiliotoxin, Decahydroquinoline, Epibatidine) killed significantly the animals in the experimental groups (p< 0.01). (Received March 2, 2010; accepted April 21, 2010) Keywords: Bufadienolides,Amphibian peptides and alkoloids Gammarus pulex, 1. Introductıon Amphibian skin secretions are considered a rich source of biologically active compounds and are known to be rich in peptides, bufadienolides and alkaloids. Bufadienolides are cardioactive steroids from animals and plants that have also been reported to possess antimicrobial activities. Amphibian skin contains a remarkable spectrum of biologically active compounds, including biogenic amines, peptides, proteins, bufadienolides, tetrodotoxins and lipophilic alkaloids[1-7]. The lipophilic alkaloids include the samandarines and an incredible array of piperidine-based, pyrrolidine-based, and steroidal alkaloids. -

Arenobufagin Intercalates with DNA Leading to G Cell Cycle Arrest Via
www.impactjournals.com/oncotarget/ Oncotarget, Vol. 6, No. 33 Arenobufagin intercalates with DNA leading to G2 cell cycle arrest via ATM/ATR pathway Li-Juan Deng1,*, Qun-Long Peng1,*, Long-Hai Wang1, Jun Xu1, Jun-Shan Liu2, Ying- Jie Li1, Zhen-Jian Zhuo1, Liang-Liang Bai1, Li-Ping Hu1, Wei-Min Chen1, Wen-Cai Ye1, Dong-Mei Zhang1 1 Guangdong Province Key Laboratory of Pharmacodynamic Constituents of TCM and New Drugs Research, College of Pharmacy, Jinan University, Guangzhou 510632, P.R. China 2School of Traditional Chinese Medicine, Southern Medical University, Guangzhou 510632, P.R. China *These authors have contributed equally to this work Correspondence to: Dong-Mei Zhang, e-mail: [email protected] Wen-Cai Ye, e-mail: [email protected] Keywords: arenobufagin, DNA intercalator, DNA damage response, G2 cell cycle arrest Received: May 26, 2015 Accepted: October 02, 2015 Published: October 13, 2015 ABSTRACT Arenobufagin, a representative bufadienolide, is the major active component in the traditional Chinese medicine Chan’su. It possesses significant antineoplastic activity in vitro. Although bufadienolide has been found to disrupt the cell cycle, the underlying mechanisms of this disruption are not defined. Here, we reported that arenobufagin blocked the transition from G2 to M phase of cell cycle through inhibiting the activation of CDK1-Cyclin B1 complex; The tumor suppressor p53 contributed to sustaining arrest at the G2 phase of the cell cycle in hepatocellular carcinoma (HCC) cells. Moreover, arenobufagin caused double-strand DNA breaks (DSBs) and triggered the DNA damage response (DDR), partly via the ATM/ATR-Chk1/Chk2-Cdc25C signaling pathway. Importantly, we used a synthetic biotinylated arenobufagin-conjugated chemical probe in live cells to show that arenobufagin accumulated mainly in the nucleus. -
![Toxins of Animals) [Biological-Origin Toxins]](https://docslib.b-cdn.net/cover/0935/toxins-of-animals-biological-origin-toxins-4430935.webp)
Toxins of Animals) [Biological-Origin Toxins]
4: Zootoxins (toxins of animals) [Biological-origin toxins] Distinction should be made between poisonous animals – those with toxins in their skin or other organs and which are toxic on ingestion – and venomous animals – those with specialised structures for production and delivery of toxins (venoms) to prey species or adversaries. Halstead (1988) published a monumental review of poisonous and venomous marine animals. A world list of snake venoms and other animal toxins including bee venoms, sawfly toxins, amphibian and fish toxins has been compiled by Theakston & Kamiguti (2002). Animals acquire toxins by one of three methods (Mebs 2001): • expression of genes coding for the toxin structures • metabolic synthesis (production of secondary metabolites) • uptake, storage and sequestration of toxins produced by other organisms (microbes, plants, or other animals) References: Halstead BW (1988) Poisonous and Venomous Marine Animals of the World. 2nd revised edition. The Darwin Press Inc., Princeton, New Jersey. Mebs D (2001) Toxicity in animals. Trends in evolution? Toxicon 39:87-96. Theakston RDG , Kamiguti AS (2002) A list of animal toxins and some other natural products with biological activity. Toxicon 40:579-651. PROTOZOA (PROTISTA) - DINOFLAGELLATES See Marine Microalgal (Dinoflagellate & Diatom) Toxins ARTHROPODS - INSECTS Sawfly larval peptides Core data Common sources: Lophyrotoma interrupta (Australian cattle-poisoning sawfly larvae) Arge pullata (European birch sawfly larvae) Perreyia flavipes & P. lepida (South American sawfly larvae) Animals affected: cattle, sheep, pigs Mode of action: uncharacterised Poisoning circumstances: consumption of larvae (dead & alive) at base of trees or on pasture Main effects: acute liver necrosis Diagnosis: pathology + evidence of larval presence Therapy: nil Prevention: deny access Syndrome names: sawfly larval poisoning, sawfly poisoning Chemical structure: Lophyrotomin [L] is a linear octapeptide (Oelrichs et al. -

A Map Describing the Association Between Effective Components of Traditional Chinese Medicine and Signaling Pathways in Cancer Cells in Vitro and in Vivo
ISSN 1881-7831 Online ISSN 1881-784X DD&T Drug Discoveries & Therapeutics Volume 8, Number 4 August, 2014 www.ddtjournal.com ISSN: 1881-7831 Online ISSN: 1881-784X CODEN: DDTRBX Issues/Year: 6 Language: English Publisher: IACMHR Co., Ltd. Drug Discoveries & Therapeutics is one of a series of peer-reviewed journals of the International Research and Cooperation Association for Bio & Socio-Sciences Advancement (IRCA-BSSA) Group and is published bimonthly by the International Advancement Center for Medicine & Health Research Co., Ltd. (IACMHR Co., Ltd.) and supported by the IRCA-BSSA and Shandong University China-Japan Cooperation Center for Drug Discovery & Screening (SDU-DDSC). Drug Discoveries & Therapeutics publishes contributions in all fields of pharmaceutical and therapeutic research such as medicinal chemistry, pharmacology, pharmaceutical analysis, pharmaceutics, pharmaceutical administration, and experimental and clinical studies of effects, mechanisms, or uses of various treatments. Studies in drug-related fields such as biology, biochemistry, physiology, microbiology, and immunology are also within the scope of this journal. Drug Discoveries & Therapeutics publishes Original Articles, Brief Reports, Reviews, Policy Forum articles, Case Reports, News, and Letters on all aspects of the field of pharmaceutical research. All contributions should seek to promote international collaboration in pharmaceutical science. Editorial Board Editor-in-Chief: Xiao-Kang LI National Research Institute for Child Health and Development, Kazuhisa -

Occurrence of Marinobufotoxin and Telocinobufotoxin Homologs in the Skin of Bufo Bankorensis Borbour1) KAZUTAKE SHIMADA, YOSHI
2300 Vol. 35 (1987) Chem. Pharm. Bull. 35( 6 )2300-2304(1987), Occurrence of Marinobufotoxin and Telocinobufotoxin Homologs in the Skin of Bufo bankorensis BORBOuR1) KAZUTAKESHIMADA, YOSHIHIRO SATO, and TOSHIONAMBARA* PharmaceuticalInstitute, Tohoku University, Aobayama, Sendai 980, Japan (ReceivedNovember 13, 1986) The occurrenceof marinobufagin3-succinyl-L-arginine and 3-glutaryl-L-arginineesters, and telocinobufagin3-glutaryl-L-arginine ester, together with seven known bufogenins, in the skinof Bufo bankorensisBORBOUR, is reported. The structureswere elucidatedby degradativemeans and/ordirect comparisonwith authenticsamples. These compounds were assayed for inhibitory activitytowards guinea pig heart Na+, K+-adenosine triphosphatase. Keywords-Bufo bankorensis;toad venom; bufogenin;marinobufotoxin homolog; telo- cinobufotoxinhomolog; sodium-potassium-activated ATPase inhibition In a series of studies on toad venom,2) we characterized the cardiac steroids in the skin of Formosan toad, Bufo bankorensis BORBOUR, and assayed them for Na +-adenosine triphosphatase (Na+, K +-ATPase; EC 3.6.1.3) inhibitory activity.3) Five toads were sacrificed by freezing in dry ice, and the skins were immediately flayed off and extracted with ethanol. The ethanolic extract was concentrated in vacuo and the residue was subjected to column chromatography on silica gel. Subsequent separation of the bufogenin and bufotoxin mixture was repeatedly done by high-performance liquid chromat- ography (HPLC) on a reversed-phase column. Three new bufotoxins (5a, 5b, 10) were isolated as colorless amorphous substances, which gave negative ninhydrin and positive Sakaguchi tests. Upon hydrolysis with 6 N hydrochloric acid, arginine was produced and identified by thin-layer chromatography (TLC). When subjected to enzymic hydrolysis with a hog pancreas lipase preparation followed by methylation with diazomethane, these bufotoxins afforded bufogenin 3-hemi- carboxylate methyl esters (3a, 3b, 8).