A Sense of Purpose What It Means to Be a Nurse Volume 2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
2012 Edition
2012 Edition Cleveland State Community College ENGLISH DEPARTMENT Editor: Julie Fulbright Assistant Editor: Heather Cline Liner Front cover photography by: Amanda Guffey Graphic Design and Production: CSCC Marketing Department Printer: Dockins Graphics, Cleveland, Tenn. Copyright: 2012 Cleveland State Community College www.clevelandstatecc.edu All Rights Reserved Funding for this publication provided under Title I of the Carl D. Perkins Career and Technical Education Act of 2006. CSCC HUM/12095/04092012 - Cleveland State Community College is an AA/ EEO employer and does not discriminate on the basis of race, color, national origin, sex, disability or age in its program and activities. The following department has been designated to handle inquiries regarding the non-discrimination policies: Human Resources P.O. Box 3570 Cleveland, TN 37320-3570 [email protected] Table of Contents Written By Title Photo/Drawing By: Page Frankie Conar After the Storm Julie Fulbright 5 Brittney Glover Weep for Me James Loyless 6 Leaves of the Sea Amanda Guffey 7 Stormy Fisher Mother 8 Savannah Tioaquen I Am the Wind Brandon Perry 9 Tracey Thompson Rose Amanda Guffey 10 Mirror Mirror Megan Payne 11 Tonya Arsenault Siblings Marchelle Wear 12-13 We Can’t Go Back in Time Kimberley Stewart 14-15 Angel Jadoobirsingh Spying Angel Jadoobirsingh 16 My Pay Angel Crawford 17 Cody Thrift Through Solemn Eyes Misti Stoika 18 I Had a Dream I Died Alonzo Bell 19-20 The Hero Tonya Arsenault 21-22 Nicholas Johnson Such Is Life Angel Jadoobirsingh 23 Turn the Lights Out 24 The Window by the Tree Marchelle Wear 25 Chet Guthrie Christmas on the Battlefield Amanda Guffey 26-29 Sweet Kalan Tonya Arsenault 30-34 The 23rd Psalm Marchelle Wear 35-37 Letters through the Fence Marchelle Wear 38-42 Grandfather’s Axe Marchelle Wear 43-44 Her Beauty Daniel Stokes 45 In the Eyes of a Dreamer Megan Payne 46 Rise o’ Rise Dear Wall Street 47 The Old Man Michael Espinoza 48 A Night of Passion Shanna Calfee 49-50 Table of Contents - Cont’d. -

TTTC Full Text
The Things They Carried By Tim O’Brien The Things They Carried First Lieutenant Jimmy Cross carried letters from a girl named Martha, a junior at Mount Sebastian College in New Jersey. They were not love letters, but Lieutenant Cross was hoping, so he kept them folded in plastic at the bottom of his rucksack. In the late afternoon, after a day's march, he would dig his foxhole, wash his hands under a canteen, unwrap the letters, hold them with the tips of his fingers, and spend the last hour of light pretending. He would imagine romantic camping trips into the White Mountains in New Hampshire. He would sometimes taste the envelope flaps, knowing her tongue had been there. More than anything, he wanted Martha to love him as he loved her, but the letters were mostly chatty, elusive on the matter of love. She was a virgin, he was almost sure. She was an English major at Mount Sebastian, and she wrote beautifully about her professors and roommates and midterm exams, about her respect for Chaucer and her great affection for Virginia Woolf. She often quoted lines of poetry; she never mentioned the war, except to say, Jimmy, take care of yourself. The letters weighed 10 ounces. They were signed Love, Martha, but Lieutenant Cross understood that Love was only a way of signing and did not mean what he sometimes pretended it meant. At dusk, he would carefully return the letters to his rucksack. Slowly, a bit distracted, he would get up and move among his men, checking the perimeter, then at full dark he would return to his hole and watch the night and wonder if Martha was a virgin. -

Les Mis, Lyrics
LES MISERABLES Herbert Kretzmer (DISC ONE) ACT ONE 1. PROLOGUE (WORK SONG) CHAIN GANG Look down, look down Don't look 'em in the eye Look down, look down You're here until you die. The sun is strong It's hot as hell below Look down, look down There's twenty years to go. I've done no wrong Sweet Jesus, hear my prayer Look down, look down Sweet Jesus doesn't care I know she'll wait I know that she'll be true Look down, look down They've all forgotten you When I get free You won't see me 'Ere for dust Look down, look down Don't look 'em in the eye. !! Les Miserables!!Page 2 How long, 0 Lord, Before you let me die? Look down, look down You'll always be a slave Look down, look down, You're standing in your grave. JAVERT Now bring me prisoner 24601 Your time is up And your parole's begun You know what that means, VALJEAN Yes, it means I'm free. JAVERT No! It means You get Your yellow ticket-of-leave You are a thief. VALJEAN I stole a loaf of bread. JAVERT You robbed a house. VALJEAN I broke a window pane. My sister's child was close to death And we were starving. !! Les Miserables!!Page 3 JAVERT You will starve again Unless you learn the meaning of the law. VALJEAN I know the meaning of those 19 years A slave of the law. JAVERT Five years for what you did The rest because you tried to run Yes, 24601. -

The UK Top 200 Most Requested Songs in 2017 This List Is Compiled Based on Over 2 Million Song Requests Made Using the DJ Event Planner Song Request System
The UK Top 200 Most Requested Songs In 2017 This list is compiled based on over 2 million song requests made using the DJ Event Planner song request system. Rank Song Song Title 1 Mark Ronson feat. Bruno Mars Uptown Funk 2 Killers Mr. Brightside 3 Whitney Houston I Wanna Dance With Somebody (Who Loves Me) 4 Pharrell Williams Happy 5 Bon Jovi Livin' On A Prayer 6 Kings Of Leon Sex On Fire 7 Bryan Adams Summer Of '69 8 Justin Timberlake Can't Stop The Feeling! 9 ABBA Dancing Queen 10 Black Eyed Peas I Gotta Feeling 11 Bruno Mars Marry You 12 Walk The Moon Shut Up And Dance 13 Dexys Midnight Runners Come On Eileen 14 Taylor Swift Shake It Off 15 Queen Don't Stop Me Now 16 Rihanna feat. Calvin Harris We Found Love 17 Journey Don't Stop Believin' 18 Ed Sheeran Shape Of You 19 Beyonce Single Ladies (Put A Ring On It) 20 Ed Sheeran Thinking Out Loud 21 DJ Casper Cha Cha Slide 22 Beyonce feat. Jay-Z Crazy In Love 23 Oasis Wonderwall 24 Wham! Wake Me Up Before You Go-Go 25 B-52's Love Shack 26 John Travolta & Olivia Newton-John Grease Megamix 27 Foundations Build Me Up Buttercup 28 Maroon 5 Moves Like Jagger 29 Los Del Rio Macarena 30 Van Morrison Brown Eyed Girl 31 Guns N' Roses Sweet Child O' Mine 32 Toploader Dancing In The Moonlight 33 Arctic Monkeys I Bet You Look Good On The Dancefloor 34 Mark Ronson feat. Amy Winehouse Valerie 35 House Of Pain Jump Around 36 Stevie Wonder Superstition 37 Village People Y.M.C.A. -

The Cathedral of the Diocese of Manchester the Most Reverend
Saint Joseph Cathedral The Cathedral of the Diocese of Manchester The Most Reverend Peter A. Libasci Tenth Bishop of Manchester Clergy August 22, 2021 Very Reverend Jason Y. Jalbert Rector and Pastor TwentyFirst Sunday in Ordinary Time Reverend Eric T. Delisle Pastor Saint Hedwig Weekend Mass: Reverend Deacon Karl T. Cooper Saturday 4:00 PM Permanent Deacon Sunday 8:30 AM, 10:30 AM, Pastoral and Office Staff 6:00 PM Kelly Bender Director of Faith Formation Weekday Mass: Eric J. Bermani MondayFriday (Chapel) 7:00 AM Director of Music First Friday (Chapel) 12:10 PM Karol Carroll Bookkeeper Saturday (Cathedral) 8:00 AM Stacey Donovan Holy Days as announced Administrative Assistant Judy LabbeHuard Confessions: Director of Communications & MondayFriday (Chapel) Parish Support 7:308:00 AM Saturday (Cathedral) In Residence 7:308:00 AMand 2:303:30 PM Most Reverend Francis J. Christian Auxiliary Bishop Emeritus 145 Lowell Street Monsignor C. Peter Dumont Manchester, New Hampshire 03104 Reverend Elson Kattookaran M.S. www.stjosephcathedralnh.org Chaplain Catholic Medical Center Telephone: 6036226404 Reverend Jeffrey Statz Pastor St. Francis of Assisi Rectory Office Hours: MondayThursday 9:00 a.m.2:00 p.m. Follow us on Facebook: Cathedral of Saint Joseph, Manchester, New Hampshire SǂNJǏǕ JǐǔdžǑlj CǂǕljdžDžǓǂǍ, MǂǏDŽljdžǔǕdžǓ, NH From the Desk of Father Jason Dear Friends, Prayer to Saint Monica This week the Church celebrates the feast days of a mother Under the weight of my heartful burden, I turn to you, dear and her son. On Friday the 27th we honor St. Monica and on Saint Monica and request your assistance and intercession. -

Partyman by Title
Partyman by Title #1 Crush (SCK) (Musical) Sound Of Music - Garbage - (Musical) Sound Of Music (SF) (I Called Her) Tennessee (PH) (Parody) Unknown (Doo Wop) - Tim Dugger - That Thing (UKN) 007 (Shanty Town) (MRE) Alan Jackson (Who Says) You - Can't Have It All (CB) Desmond Decker & The Aces - Blue Oyster Cult (Don't Fear) The - '03 Bonnie & Clyde (MM) Reaper (DK) Jay-Z & Beyonce - Bon Jovi (You Want To) Make A - '03 Bonnie And Clyde (THM) Memory (THM) Jay-Z Ft. Beyonce Knowles - Bryan Adams (Everything I Do) I - 1 2 3 (TZ) Do It For You (SCK) (Spanish) El Simbolo - Carpenters (They Long To Be) - 1 Thing (THM) Close To You (DK) Amerie - Celine Dion (If There Was) Any - Other Way (SCK) 1, 2 Step (SCK) Cher (This Is) A Song For The - Ciara & Missy Elliott - Lonely (THM) 1, 2, 3, 4 (I Love You) (CB) Clarence 'Frogman' Henry (I - Plain White T's - Don't Know Why) But I Do (MM) 1, 2, 3, 4, Sumpin' New (SF) Cutting Crew (I Just) Died In - Coolio - Your Arms (SCK) 1,000 Faces (CB) Dierks Bentley -I Hold On (Ask) - Randy Montana - Dolly Parton- Together You And I - (CB) 1+1 (CB) Elvis Presley (Now & Then) - Beyonce' - There's A Fool Such As I (SF) 10 Days Late (SCK) Elvis Presley (You're So Square) - Third Eye Blind - Baby I Don't Care (SCK) 100 Kilos De Barro (TZ) Gloriana (Kissed You) Good - (Spanish) Enrique Guzman - Night (PH) 100 Years (THM) Human League (Keep Feeling) - Five For Fighting - Fascination (SCK) 100% Pure Love (NT) Johnny Cash (Ghost) Riders In - The Sky (SCK) Crystal Waters - K.D. -

4920 10 Cc D22-01 2Pac D43-01 50 Cent 4877 Abba 4574 Abba
ALDEBARAN KARAOKE Catálogo de Músicas - Por ordem de INTÉRPRETE Código INTÉRPRETE MÚSICA TRECHO DA MÚSICA 4920 10 CC I´M NOT IN LOVE I´m not in love so don´t forget it 19807 10000 MANIACS MORE THAN THIS I could feel at the time there was no way of D22-01 2PAC DEAR MAMA You are appreciated. When I was young 9033 3 DOORS DOWN HERE WITHOUT YOU A hundred days had made me older 2578 4 NON BLONDES SPACEMAN Starry night bring me down 9072 4 NON BLONDES WHAT´S UP Twenty-five years and my life is still D36-01 5 SECONDS OF SUMMER AMNESIA I drove by all the places we used to hang out D36-02 5 SECONDS OF SUMMER HEARTBREAK GIRL You called me up, it´s like a broken record D36-03 5 SECONDS OF SUMMER JET BLACK HEART Everybody´s got their demons even wide D36-04 5 SECONDS OF SUMMER SHE LOOKS SO PERFECT Simmer down, simmer down, they say we D43-01 50 CENT IN DA CLUB Go, go, go, go, shawty, it´s your birthday D54-01 A FLOCK OF SEAGULLS I RAN I walk along the avenue, I never thought I´d D35-40 A TASTE OF HONEY BOOGIE OOGIE OOGIE If you´re thinkin´ you´re too cool to boogie D22-02 A TASTE OF HONEY SUKIYAKI It´s all because of you, I´m feeling 4970 A TEENS SUPER TROUPER Super trouper beams are gonna blind me 4877 ABBA CHIQUITITA Chiquitita tell me what´s wrong 4574 ABBA DANCING QUEEN Yeah! You can dance you can jive 19333 ABBA FERNANDO Can you hear the drums Fernando D17-01 ABBA GIMME GIMME GIMME Half past twelve and I´m watching the late show D17-02 ABBA HAPPY NEW YEAR No more champagne and the fireworks 9116 ABBA I HAVE A DREAM I have a dream a song to sing… -

Karaoke Mietsystem Songlist
Karaoke Mietsystem Songlist Ein Karaokesystem der Firma Showtronic Solutions AG in Zusammenarbeit mit Karafun. Karaoke-Katalog Update vom: 13/10/2020 Singen Sie online auf www.karafun.de Gesamter Katalog TOP 50 Shallow - A Star is Born Take Me Home, Country Roads - John Denver Skandal im Sperrbezirk - Spider Murphy Gang Griechischer Wein - Udo Jürgens Verdammt, Ich Lieb' Dich - Matthias Reim Dancing Queen - ABBA Dance Monkey - Tones and I Breaking Free - High School Musical In The Ghetto - Elvis Presley Angels - Robbie Williams Hulapalu - Andreas Gabalier Someone Like You - Adele 99 Luftballons - Nena Tage wie diese - Die Toten Hosen Ring of Fire - Johnny Cash Lemon Tree - Fool's Garden Ohne Dich (schlaf' ich heut' nacht nicht ein) - You Are the Reason - Calum Scott Perfect - Ed Sheeran Münchener Freiheit Stand by Me - Ben E. King Im Wagen Vor Mir - Henry Valentino And Uschi Let It Go - Idina Menzel Can You Feel The Love Tonight - The Lion King Atemlos durch die Nacht - Helene Fischer Roller - Apache 207 Someone You Loved - Lewis Capaldi I Want It That Way - Backstreet Boys Über Sieben Brücken Musst Du Gehn - Peter Maffay Summer Of '69 - Bryan Adams Cordula grün - Die Draufgänger Tequila - The Champs ...Baby One More Time - Britney Spears All of Me - John Legend Barbie Girl - Aqua Chasing Cars - Snow Patrol My Way - Frank Sinatra Hallelujah - Alexandra Burke Aber Bitte Mit Sahne - Udo Jürgens Bohemian Rhapsody - Queen Wannabe - Spice Girls Schrei nach Liebe - Die Ärzte Can't Help Falling In Love - Elvis Presley Country Roads - Hermes House Band Westerland - Die Ärzte Warum hast du nicht nein gesagt - Roland Kaiser Ich war noch niemals in New York - Ich War Noch Marmor, Stein Und Eisen Bricht - Drafi Deutscher Zombie - The Cranberries Niemals In New York Ich wollte nie erwachsen sein (Nessajas Lied) - Don't Stop Believing - Journey EXPLICIT Kann Texte enthalten, die nicht für Kinder und Jugendliche geeignet sind. -

Wycliffe Gordon at GRU
World-renownedtrombonist Practiceby Jim Garvey makes Wycliffehas reached Gordon the pinnacle ofand music now success he is Perfect with the sharing his expertise music department at GRU. HOW DO YOU GET TO GRU’S MAXWELL THEATRE? PRACTICE, PRACTICE, PRACTICE. At least that’s how Wycliffe Gordon, the best jazz trombonist in the world, got there. After years of teaching at Juilliard and the Manhattan School of Music, touring the world with Wynton Marsalis and the Lincoln Center Jazz Orchestra, performing with symphony orchestras, recording, com- posing, arranging, giving workshops, lectures and master classes, Gordon was finally offered the job he’s been preparing for all these years: artist-in-residence in GRU’s Department of Music. “I’ve come full circle, teaching at a university in my own town after teaching all over the world,” Gordon says. “I’m from here. My high school, Butler High School, is here. My mom lives here. Coming to GRU is Jazz trombonist and composer Wycliffe Gordon performs on stage at like icing on the cake.” u Davidson Fine Arts School in 2008. 32 • Augusta April 2015 April 2015 Augusta • 33 “...a full, powerful tone, slurring then slippingsliding and growling BUT TRADING IN NEW YORK CITY FOR HEPHZIBAH? His fame is never on display. With his round, boyish face and twinkling eyes, “I had a place in New York for 15 “During his solo, Gordon locked in Currier, an opera singer who has sung he’s more playful imp than musical phenom. Still phenom is what he is. years. I’ve had enough pretty much. -
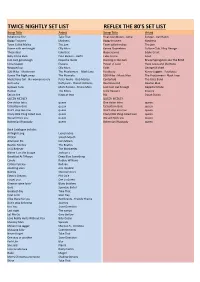
Twice Nightly Set List Reflex the 80'S Set List
TWICE NIGHTLY SET LIST REFLEX THE 80'S SET LIST Song Title Artist Song Title Artist Relight my Fire Take That Final countdown - Jump Europe - Van Halen Baggy Trousers Madness Baggy trousers Madness Town Called Malice The jam Town called malice The jam Dance with me tonight Olly Murs Karma Chameleon Culture Club / Boy George These days take that Hope Joanna Eddie Grant Baby Come Back Pato Banton - UB40 Take on me A-HA Just cant get enough Depeche mode Dancing in the dark Bruice Springstein aka The BOSS Little respect Erasure Power of Love Huey Lewis and the News Wrapped up Olly Murs Faith George Michael 500 Miles - Music man The Proclaimers - Black Lace Footloose Kenny Loggins - Footloose Dance The Night away The Mavricks 500 Miles - Music Man The Proclaimers - Black Lace Mysterious Girl - No woman no cry Peter Andre - Bob Marley Centerfold The Giles Band Get Lucky Daft punk - Pharell Williams Real Gone Kid Deacon Blue Uptown Funk Mark Ronson - Bruno Mars Just Cant Get Enough Depeche Mode Human The Killers Little Respect Erasure Sex on fire Kings of leon Rio Duran Duran QUEEN MEDLEY QUEEN MEDLEY One vision Intro queen One vision Intro queen fat bottom Girls queen fat bottom Girls queen Don’t stop me now queen Don’t stop me now queen Crazy little thing called love queen Crazy little thing called love queen We will Rock you queen We will Rock you queen Bohemian Rhapsody queen Bohemian Rhapsody queen Back Catalogue include; All Night Long Lionel richie All Star Smash Mouth American Pie Don Mclain Beatles Medley The Beatles Im A Believer The -

JSU Writing Project Anthology
JACKSONVILLE STATE UNIVERSITY WRITING PROJECT ANTHOLOGY SUMMER1992 J A C K S O N V I L L E S T A T E U N I V E R S I T Y 11 W R I T I N G P R O J E C T A N T H O L O G Y S U M M E R 1 9 9 2 Jacksonville State University i ! Jacksonville, Alabama ' ' DIRECTOR Lisa McLean Williams English Department ,I I, Jacksonville State University i ASSISTANT DIRECTOR G. Kenneth Guthrie English Department Jacksonville State University I I I I DEDICATION The teacher-fellows of the Jacksonville State University Writing Project, 1992, hereby dedicate this anthology to Judy Ramsey and her staff, Maria Amado, Debbie Kipp and Kim Howard, who persistently and patiently made our words real. I i ( ! I ' I Foreword I Eighteen strangers, we came together during the hot, humid days of Summer 1992. We met, laughed, cried, learned, taught, and wrote, and wrote, and wrote, and wrote, and wrote. Between June 29 and July 30, as participants in the fifth I i annual JSU Writing Project Summer Institute, we found l ! enthusiasm, friendship, inspiration, and rejuvenation. From those five weeks emerged a sense of love for our profession I i and respect for our colleagues. Eighteen friends, we said good-bye, having shared a part of ourselves with each other and those who will read this anthology. CONTEN'rs Dedication Foreword 1992 Teacher Fellows 1 Schedule ... 4 Demonstration Summaries 5 Writing by Participants Patricia Bates 12 Willie Charley 20 Cristy Colvin. -

At Last”—Etta James (1961) Added to the National Registry: 2008 Essay by Cary O’Dell
“At Last”—Etta James (1961) Added to the National Registry: 2008 Essay by Cary O’Dell Etta James Original label Original LP Etta James’s legendary 1961 recording of “At Last” was one of her first releases for the Chess/Argo recording label after beginning her career with the Modern label. The change in companies also marked a change in James’s career. She recounted in her 1995 autobiography, “Rage to Survive”: I was no longer a teenager. I was twenty-two and sophisticated. Or at least I wanted to be sophisticated. So when Harvey [Fuqua, formerly of the Moonglows, and then James’s boyfriend] got out his “Book of One Hundred Standards” and began playing through old songs, I got excited. I saw in that music the mysterious life that my mother had led when I was a little girl, the life I secretly dreamed of living myself. I wanted to escape into a world of glamour and grace and easy sin. “At Last” was the first one to hit big…. Because of the way I phrased it, some people started calling me a jazz singer. And it was a change. Before her switch to Chess, James (born Jamesetta Hawkins in 1938) had primarily scored as a recording artist with what she would later call “quickie teenage rockin’, humping and bumping ditties.” Indeed, her oeuvre up to that time had been marked with such titles as “Dance With Me, Henry” (her breakthrough), “All I Could Do Was Cry,” and “My Dearest Darling.” And though “At Last” (from James’s album of the same name) was also about an endearing love, James’s soulful approach certainly bespoke of a more mature singer fully coming into her own.