Death by Strangulation – Dr. Dean Hawley
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Heat Stroke Heat Exhaustion
Environmental Injuries Co lin G. Ka ide, MD , FACEP, FAAEM, UHM Associate Professor of Emergency Medicine Board-Certified Specialist in Hyperbaric Medicine Specialist in Wound Care The Ohio State University Wexner Medical Center The Most Dangerous Drug Combination… Accidental Testosterone Hypothermia and Alcohol! The most likely victims… Photo: Ralf Roletschek 1 Definition of Blizzard Hypothermia of Subnormal T° when the body is unable to generate sufficient heat to sustain normal functions Core Temperature < 95°F 1979 (35°C) Most Important Temperatures Thermoregulation 95°F (35° C) Hyper/Goofy The body uses a Poikilothermic shell to maintain a Homeothermic core 90°F (32°C) Shivering Stops Maintains core T° w/in 1.8°F(1°C) 80°F (26. 5°C) Vfib, Coma Hypothalamus Skin 65°F (18°C) Asystole Constant T° 96.896.8-- 100.4° F 2 Thermoregulation The 2 most important factors Only 3 Causes! Shivering (10x increase) Decreased Heat Production Initiated by low skin temperature Increased Heat Loss Warming the skin can abolish Impaired Thermoregulation shivering! Peripheral vasoconstriction Sequesters heat Predisposing Predisposing Factors Factors Decreased Production Increased Loss –Endocrine problems Radiation Evaporation • Thyroid Conduction* • Adrenal Axis Convection** –Malnutrition *Depends on conducting material **Depends on wind velocity –Neuromuscular disease 3 Predisposing Systemic Responses CNS Factors T°< 90°F (34°C) Impaired Regulation Hyperactivity, excitability, recklessness CNS injury T°< 80°F (27°C) Hypothalamic injuries Loss of voluntary -

Analysis of Accidents and Sickness of Divers and Scuba Divers at the Training Centre for Divesr and Scuba Divers of the Polish Army
POLISH HYPERBARIC RESEARCH 2(71)2020 Journal of Polish Hyperbaric Medicine and Technology Society ANALYSIS OF ACCIDENTS AND SICKNESS OF DIVERS AND SCUBA DIVERS AT THE TRAINING CENTRE FOR DIVESR AND SCUBA DIVERS OF THE POLISH ARMY Władysław Wolański Polish Army Diver and Diver Training Centre, Naval Psychological Laboratory, Gdynia, Poland ARTICLE INFO PolHypRes 2020 Vol. 71 Issue 2 pp. 75 – 78 ISSN: 1734-7009 eISSN: 2084-0535 DOI: 10.2478/phr-2020-0013 Pages: 14, figures: 0, tables: 0 page www of the periodical: www.phr.net.pl Publisher Polish Hyperbaric Medicine and Technology Society 2020 Vol. 71 Issue 2 INTRODUCTION The first group of diseases occurs as a result of mechanical action directly on the body of the diver. Among The prerequisite for the prevention of diving- them are: ear and paranasal sinus barotrauma, pulmonary related sicknesses and accidents is strict compliance with barotrauma, crushing. both technical and medical regulations during diving In the second group we most often encounter the training and work [3,4]. consequences of the toxic effects of gaseous components of A very important issue is good knowledge of the air on the human body. This group includes decompression work of a diver and the anticipation of possible dangers by sickness, oxygen poisoning, nitrogen poisoning, CO2 the personnel participating in the dive [1]. The Military poisoning, carbon monoxide (CO) poisoning. Maritime Medical Committee (WKML) determines When analysing the causes of diving sicknesses whether or not an individual is healthy enough to dive, and accidents at the Diver and Scuba Diver Training Centre granting those who meet the required standards a medical of the Polish Army, certain groups of additional factors certificate that is valid for one year [1,2]. -

Dysbarism - Barotrauma
DYSBARISM - BAROTRAUMA Introduction Dysbarism is the term given to medical complications of exposure to gases at higher than normal atmospheric pressure. It includes barotrauma, decompression illness and nitrogen narcosis. Barotrauma occurs as a consequence of excessive expansion or contraction of gas within enclosed body cavities. Barotrauma principally affects the: 1. Lungs (most importantly): Lung barotrauma may result in: ● Gas embolism ● Pneumomediastinum ● Pneumothorax. 2. Eyes 3. Middle / Inner ear 4. Sinuses 5. Teeth / mandible 6. GIT (rarely) Any illness that develops during or post div.ing must be considered to be diving- related until proven otherwise. Any patient with neurological symptoms in particular needs urgent referral to a specialist in hyperbaric medicine. See also separate document on Dysbarism - Decompression Illness (in Environmental folder). Terminology The term dysbarism encompasses: ● Decompression illness And ● Barotrauma And ● Nitrogen narcosis Decompression illness (DCI) includes: 1. Decompression sickness (DCS) (or in lay terms, the “bends”): ● Type I DCS: ♥ Involves the joints or skin only ● Type II DCS: ♥ Involves all other pain, neurological injury, vestibular and pulmonary symptoms. 2. Arterial gas embolism (AGE): ● Due to pulmonary barotrauma releasing air into the circulation. Epidemiology Diving is generally a safe undertaking. Serious decompression incidents occur approximately only in 1 in 10,000 dives. However, because of high participation rates, there are about 200 - 300 cases of significant decompression illness requiring treatment in Australia each year. It is estimated that 10 times this number of divers experience less severe illness after diving. Physics Boyle’s Law: The air pressure at sea level is 1 atmosphere absolute (ATA). Alternative units used for 1 ATA include: ● 101.3 kPa (SI units) ● 1.013 Bar ● 10 meters of sea water (MSW) ● 760 mm of mercury (mm Hg) ● 14.7 pounds per square inch (PSI) For every 10 meters a diver descends in seawater, the pressure increases by 1 ATA. -

Pulmonary Barotrauma During Hypoxia in a Diver While Underwater
POLISH HYPERBARIC RESEARCH 2(71)2020 Journal of Polish Hyperbaric Medicine and Technology Society PULMONARY BAROTRAUMA DURING HYPOXIA IN A DIVER WHILE UNDERWATER Brunon Kierznikowicz, Władysław Wolański, Romuald Olszański Institute of Maritime and Tropical Medicine of the Military Medical Academy, Gdynia, Poland ABSTRACT The article describes a diver performing a dive at small depths in a dry suit, breathing from a single-stage apparatus placed on his back. As a result of training deficiencies, the diver began breathing from inside the suit, which led to hypoxia and subsequent uncontrolled ascent. Upon returning to the surface, the diver developed neurological symptoms based on which a diagnosis of pulmonary barotrauma was made. The diver was successfully treated with therapeutic recompression-decompression. Keywords: diving, accident, hypoxia, pulmonary barotrauma. ARTICLE INFO PolHypRes 2020 Vol. 71 Issue 2 pp. 45 – 50 ISSN: 1734-7009 eISSN: 2084-0535 Casuistic (case description) article DOI: 10.2478/phr-2020-0009 Pages: 6, figures: 0, tables: 1 Originally published in the Naval Health Service Yearbook 1977-1978 page www of the periodical: www.phr.net.pl Acceptance for print in PHR: 27.10.2019 r. Publisher Polish Hyperbaric Medicine and Technology Society 2020 Vol. 71 Issue 2 INTRODUCTION that he suddenly experienced an "impact" from an increased amount of air flowing into his lungs during In recent years, we can observe a continuous inhalation. Fearing a lung injury, he immediately pulled the dynamic development of diving technology. At the same mouthpiece out of his mouth and started breathing air time, the spectrum of works carried out by scuba divers for from inside the suit for about 2 minutes. -

The Neuropsychological Sequelae of Attempted Hanging
546 Journal ofNeurology, Neurosurgery, and Psychiatry 1991;54:546-548 SHORT REPORT J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.54.6.546 on 1 June 1991. Downloaded from The neuropsychological sequelae of attempted hanging Alice A Medalia, Arnold E Merriam, John H Ehrenreich Abstract by paranoid delusions, thought blocking and Only one report on the neuropsycho- suspiciousness. At that time he had a gross logical sequelae of attempted hanging impairment in recent memory. Psychological exists in the English language. Two cases testing carried out three weeks after the hang- of attempted hanging with subsequent ing found severe memory deficits on the recall isolated memory deficits are reported. portion of the Bender Gestalt Test, a measure Possible mechanisms for induction of of nonverbal memory. IQ testing revealed a this amnesia are discussed. In these two sharp drop in intelligence from the prehang- cases it is most likely that circulatory ing level (Performance IQ = 82; Verbal IQ = disturbance produced by the ligatures 80; Full Scale IQ = 80). A neurological caused ischaemic hippocampal damage, examination three months after the hanging which in turn led to amnesia. was unremarkable except for the memory impairment. Contrast CT was normal. Seven- Every year approximately 4000 people in the teen months after the hanging his psychosis United States commit suicide by hanging.' had remitted and mental status was remark- While no precise figures are available, it is safe able only for persistent memory deficits. to assume that additional thousands Neuropsychological testing performed two unsuccessfully attempt suicide by this years after the hanging when he was non- method. -
CPAP Titration AHI (Events/Hour) 49.8 51 ODI 33.0 45.8 CAI 1.6 48 Minimum Spo2 % 72 85
GENERAL SESSION MATERIALS Sunday, June 4, 2017 © American Association of Sleep Technologists 1 AAST 39th Annual Meeting Sunday, June 4 – Tuesday, June 6, 2017 This section of the course book contains materials to be presented in general sessions on Sunday, June 4, 2017. THIS COURSE BOOK IS ONLY INTENDED FOR REVIEW BY THE INDIVIDUAL WHO ATTENDED THE COURSE. PHOTOCOPYING AND DISTRIBUTION TO OTHERS IS PROHIBITED. © American Association of Sleep Technologists 2 © American Association of Sleep Technologists 3 Can we use physiology to understand and treat obstructive sleep apnea? Exploring the Possibility of Performing Research in Your Sleep Center Robert L. Owens, MD Scott A. Sands, PhD University of California San Diego Brigham and Women’s Hospital and [email protected] Harvard Medical School [email protected] © American Association of Sleep Technologists 4 The Big Ideas • Is all OSA the same? • Are two people with the same AHI the same? • If we knew the underlying cause of OSA, could we treat people differently? • Can we do all this in the clinic? © American Association of Sleep Technologists 5 Outline • Why might different people get OSA? • Can we measure the causes in an individual? • Is that useful? © American Association of Sleep Technologists 6 What happens when you fall asleep: normal Wake Sleep Ventilation Ventilatory Demand Time © American Association of Sleep Technologists 7 What happens when you fall asleep: normal or OSA Wake Sleep Ventilation Ventilatory Ventilation ≠ Demand Demand Because of poor anatomy Time © American Association of Sleep Technologists 8 What happens when you fall asleep: normal or OSA Hypoventilation leads to increased ventilatory demand, which will activate upper airway Wake Sleep muscles to improve Ventilation ventilation. -

Techniques Frequently Used During London Olympic Judo Tournaments: a Biomechanical Approach
Techniques frequently used during London Olympic judo tournaments: A biomechanical approach S. Sterkowicz,1 A. Sacripanti2, K. Sterkowicz – Przybycien3 1 Department of Theory of Sport and Kinesiology, Institute of Sport, University School of Physical Education, Kraków, Poland 2 Chair of Biomechanics of Sports, FIJLKAM, ENEA, University of Rome “Tor Vergata”, Italy 3 Department of Gymnastics, Institute of Sport, University School of Physical Education, Kraków, Poland Abstract Feedback between training and competition should be considered in athletic training. The aim of the study was contemporary coaching tendencies in women’s and men’s judo with particular focus on a biomechanical classification of throws and grappling actions. 359 throws and 77 grappling techniques scored by male and female athletes in Olympic Judo Tournaments (London 2012) have been analyzed. Independence of traits (gender and weight category by technique classes) was verified via c2 test. Comparison between frequency of each subsequent technique class and rest/inconclusive counts was made in 2×2 contingency tables. The significance level was set at p£0.05. Throwing technique frequencies grouped in the seven biomechanical classes were dependent on gender. A significant difference was found between frequencies of variable arm of physical lever technique scored by males (27.09%) and females (16.67%) as compared to the rest/inconclusively techniques counts. Significant differences between men who competed in extra lightweight and heavy weight concerned the frequency of the techniques used with maximum arm or variable arm of physical lever and a couple of forces applied by trunk and legs. In females, a tendency to higher frequency of techniques that used couple of forces applied by arm or arms and leg was observed in extra lightweight compared to the heavy weight. -
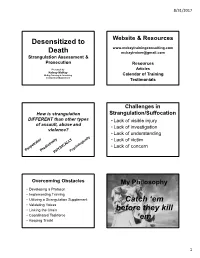
Catch ‘Em • Validating Voices • Linking the Chain Before They Kill • Coordinated Taskforce ‘Em • Keeping Track!
8/31/2017 Desensitized to Website & Resources www.mckaytrainingconsulting.com Death [email protected] Strangulation Assessment & Prosecution Resources Presented by Articles Kelsey McKay McKay Training & Consulting Calendar of Training [email protected] Testimonials Challenges in How is strangulation Strangulation/Suffocation DIFFERENT than other types • Lack of visible injury of assault, abuse and • Lack of investigation violence? • Lack of understanding • Lack of victim • Lack of concern Overcoming Obstacles My Philosophy • Developing a Protocol • Implementing Training • Utilizing a Strangulation Supplement Catch ‘em • Validating Voices • Linking the Chain before they kill • Coordinated Taskforce ‘em • Keeping Track! 1 8/31/2017 Strangulation represents an Lethality & Fatality escalation of force Continuum of Violence 90% prior history of DV After ONE non-fatal strangulation... 7-9 x 43% Women who were more likely to be murdered had been killed strangled in the last year 2 8/31/2017 Catch ‘em while It takes a certain they are killing kind of rage… Haruka Weiser Loyalty Before Betrayal •“He didn’t look like himself, it wasn’t him in his eyes” • Clenching teeth; Gritting teeth; • Squeezing so hard veins were coming out of his head; • Bulging eyes; • Bugged out eyes, angry; • Mad face Trust no bitch, Love no bitch • He had black in his eyes 3 8/31/2017 David Adams • If you had access to a gun… • Only 1 of the 8 stranglers said And a certain he would have used a gun (vs 4/6 stabbers) kind of • “I wanted to know what it felt like to kill someone” enjoyment… Source: D. Adams, Emerge “Whenever V was about to pass out, D would let go just enough to allow V to gasp for air, and then would continue strangling V. -

Review of Human Physiology in the Underwater Environment
Available online at www.ijmrhs.com cal R edi ese M ar of c l h a & n r H u e o a J l l t h International Journal of Medical Research & a S n ISSN No: 2319-5886 o c i t i Health Sciences, 2019, 8(8): 117-121 e a n n c r e e t s n I • • IJ M R H S Review of Human Physiology in the Underwater Environment Oktiyas Muzaky Luthfi1,2* 1 Marine Science University of Brawijaya, Malang, Indonesia 2 Fisheries Diving School, University of Brawijaya, Malang, Indonesia *Corresponding e-mail: [email protected] ABSTRACT Since before centuries, human tries hard to explore underwater and in 1940’s human-introduced an important and revolutionary gear i.e. scuba that allowed human-made long interaction in the underwater world. Since diving using pressure gas under pressure environment, it should be considered to remember gas law (Boyle’s law). The gas law gives a clear understanding of physiological consequences related to diving diseases such as barotrauma or condition in which tissue or organ is damage due to gas pressure. The organ which has direct effect related to compression and expansion of gas were lungs, ear, and sinus. These organs were common and potentially fatigue injury for a diver. In this article we shall review the history of scuba diving, physical stress caused underwater environment, physiology adaptation of lung, ear, and sinus, and diving disease. Keywords: Barotrauma, Boyle’s law, Scuba, Barine, Physical stress INTRODUCTION The underwater world is a place where many people dream to explore it. -

Placental Transfusion for Asphyxiated Infants
UC Davis UC Davis Previously Published Works Title Placental Transfusion for Asphyxiated Infants. Permalink https://escholarship.org/uc/item/9c95r3js Authors Katheria, Anup C Rich, Wade D Bava, Sunita et al. Publication Date 2019 DOI 10.3389/fped.2019.00473 Peer reviewed eScholarship.org Powered by the California Digital Library University of California REVIEW published: 20 November 2019 doi: 10.3389/fped.2019.00473 Placental Transfusion for Asphyxiated Infants Anup C. Katheria 1*, Wade D. Rich 1, Sunita Bava 2 and Satyan Lakshminrusimha 3 1 Sharp Mary Birch Hospital for Women & Newborns, San Diego, CA, United States, 2 Independent Researcher, San Diego, CA, United States, 3 Department of Pediatrics, University of California, Davis, Davis, CA, United States The current recommendation for umbilical cord management of non-vigorous infants (limp, pale, and not breathing) who need resuscitation at birth is to immediately clamp the umbilical cord. This recommendation is due in part to insufficient evidence for delayed cord clamping (DCC) or umbilical cord milking (UCM). These methods may provide a neuroprotective mechanism that also facilitates cardiovascular transition for non-vigorous infants at birth. Keywords: placental transfusion, cord milking, delayed cord clamping, newborn, asphyxia BACKGROUND An estimated one million newborns worldwide suffer from perinatal asphyxia which lead them to being at risk for developing hypoxic-ischemic encephalopathy (HIE) due to inadequate blood flow and oxygen delivery to the neonatal brain and other vital organs such as the heart and kidneys. The incidence of HIE is 1–3/1,000 term births in high-income countries but is 15–20 times greater in low to middle-income countries. -

Definition Brain & Vascular Choke
4/27/17! The Choke Hold Submission Breakdown Don Muzzi MD & Larry Lovelace DO UFC Events 25% of fights end in submission anaconda! d’acre! 74% of submissions are result of choke hold Does not reflect opinions of the NYSAC, FL Boxing Commission, MN, & WI Office of Combative Sports, MMA121 July 2015 (UFC 189)! PA Athletic Commission, Ojibwe Tribal Commission, Fon du Lac Tribal Commission Brain & Vascular Choke Definition A grappling hold that critically reduces or prevents air (choking) and or blood (strangling) from passing through the neck. Neuro-vascular reflexes yield decrease in cerebral blood flow (CBF) • May result in unconsciousness, injury to larynx or trachea, airway compromise… significant morbidity or mortality • Vascular Choke vs Airway Choke 15% of Cardiac Output 1! 4/27/17! Blood Supply to Brain Mechanisms and Reflexes • Auto-regulation: (AR) Intrinsic ability of the cerebral vasculature to alter its resistance in order to maintain cerebral blood flow constant over a wide range of cerebral perfusion pressures • Baroreceptor Reflex (BRR): Mechanoreceptors (stretch) in carotid vasculature that sense BP and relay information to the brain in order to maintain a proper blood pressure Cerebral Baroreceptor Reflex Hemodynamics • CPP = MAP - ICP (or CVP whichever is greater) • CBF = CPP/CVR 2! 4/27/17! Baroreceptor Reflex Pathway… ⬇CBF Venous Compression Stretched “firing” ⬇ Sympathetic ⬆Parasympathetic CPP = MAP-ICP ⬆Peripheral vasodilatation ⬇MAP & ⬇CPP" ⬇HR, ⬇inotropic state of heart, ⬇CO Autoregulation of CBF Autoregulation of CBF CPP= -

Title: Recognizing Barotrauma As an Unexpected Complication of High Flow Nasal Cannula
Title: Recognizing barotrauma as an unexpected complication of high flow nasal cannula Introduction: Spontaneous pneumomediastinum (SPM) is a rare condition defined as free air in the mediastinum without an apparent trauma. It is commonly associated with barotrauma in asthma and COPD patients. High flow nasal cannula (HFNC) has been routinely used for hypoxemic respiratory failure. We present a case of the development of SPM with extensive subcutaneous emphysema with the use of HFNC for hypoxic respiratory failure. Case Presentation: 78 year old Caucasian female with history of interstitial pulmonary fibrosis and COPD was discharged to LTACH after prolonged hospitalization for influenza-A infection complicated by acute on chronic respiratory failure. She was started on supplemental oxygen using HFNC that was progressively increased to 60 liters/min with 100% FiO2 for persistent hypoxia. Over the next four days, she was noted to have worsening facial and neck swelling with progressive dyspnea leading to transfer to the hospital. CT scan of chest noted for extensive pneumomediastinum involving the middle and anterior mediastinum with extensive subcutaneous emphysema throughout the anterior and moderately posterior chest wall extending to lower neck. Lung parenchyma revealed underlying interstitial with patchy airspace disease without evident pneumothorax. She was started on 100% FIO2 with non- rebreather mask. For symptomatic relief, Cardiothoracic surgery performed bilateral anterior chest blowhole incisions and application of negative vacuum-assisted closure on anterior chest with dramatic improvement in subcutaneous emphysema and facial swelling with persistent pneumomediastinum. Patent’s pneumomediastinum and respiratory failure persisted with high oxygen requirement with non- rebreather mask. Due to underlying advanced lung disease and persistent respiratory failure , patient’s family opted for palliative management with comfort measure and patient was transferred to hospice care.