Sodium–Glucose Cotransporter 2 Inhibitors: a Case Study in Translational Research
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Shared Cerebral Metabolic Pathology in Non-Transgenic Animal Models of Alzheimer’S And… 233 Intracellularly (Mitochondria, the Target of Toxicity)
Journal of Neural Transmission (2020) 127:231–250 https://doi.org/10.1007/s00702-020-02152-8 NEUROLOGY AND PRECLINICAL NEUROLOGICAL STUDIES - REVIEW ARTICLE Shared cerebral metabolic pathology in non‑transgenic animal models of Alzheimer’s and Parkinson’s disease Jelena Osmanovic Barilar1 · Ana Knezovic1 · Ana Babic Perhoc1 · Jan Homolak1 · Peter Riederer2,3 · Melita Salkovic‑Petrisic1,4 Received: 17 December 2019 / Accepted: 24 January 2020 / Published online: 6 February 2020 © The Author(s) 2020 Abstract Parkinson’s disease (PD) and Alzheimer’s disease (AD) are the most common chronic neurodegenerative disorders, character- ized by motoric dysfunction or cognitive decline in the early stage, respectively, but often by both symptoms in the advanced stage. Among underlying molecular pathologies that PD and AD patients have in common, more attention is recently paid to the central metabolic dysfunction presented as insulin resistant brain state (IRBS) and altered cerebral glucose metabolism, both also explored in animal models of these diseases. This review aims to compare IRBS and alterations in cerebral glucose metabolism in representative non-transgenic animal PD and AD models. The comparison is based on the selectivity of the neurotoxins which cause experimental PD and AD, towards the cellular membrane and intracellular molecular targets as well as towards the selective neurons/non-neuronal cells, and the particular brain regions. Mitochondrial damage and co- expression of insulin receptors, glucose transporter-2 and dopamine transporter on the membrane of particular neurons as well as astrocytes seem to be the key points which are further discussed in a context of alterations in insulin signalling in the brain and its interaction with dopaminergic transmission, particularly regarding the time frame of the experimental AD/ PD pathology appearance and the correlation with cognitive and motor symptoms. -

New Advances in Urea Transporter UT-A1 Membrane Trafficking
Int. J. Mol. Sci. 2013, 14, 10674-10682; doi:10.3390/ijms140510674 OPEN ACCESS International Journal of Molecular Sciences ISSN 1422-0067 www.mdpi.com/journal/ijms Review New Advances in Urea Transporter UT-A1 Membrane Trafficking Guangping Chen Department of Physiology, Emory University School of Medicine, Atlanta, GA 30322, USA; E-Mail: [email protected]; Tel.: +1-404-727-7494; Fax: +1-404-727-2648. Received: 22 April 2013; in revised form: 9 May 2013 / Accepted: 9 May 2013 / Published: 21 May 2013 Abstract: The vasopressin-regulated urea transporter UT-A1, expressed in kidney inner medullary collecting duct (IMCD) epithelial cells, plays a critical role in the urinary concentrating mechanisms. As a membrane protein, the function of UT-A1 transport activity relies on its presence in the plasma membrane. Therefore, UT-A1 successfully trafficking to the apical membrane of the polarized epithelial cells is crucial for the regulation of urea transport. This review summarizes the research progress of UT-A1 regulation over the past few years, specifically on the regulation of UT-A1 membrane trafficking by lipid rafts, N-linked glycosylation and a group of accessory proteins. Keywords: lipid rafts; glycosylation; accessory proteins; SNARE protein; cytoskeleton protein 1. Introduction Urea is the major end product of amino acid metabolism. It is generated from the ornithine cycle in liver, and is ultimately excreted by the kidney representing 90% of total nitrogen in urine. The physiological significance of urea in the production of concentrated urine was recognized by Gamble in the 1930s [1,2]. Urea reabsorbed in the kidney inner medullary collecting duct (IMCD) contributes to the development of the osmolality in the medullary interstitium. -

Therapeutic Medications Against Diabetes: What We Have and What We Expect
Advanced Drug Delivery Reviews 139 (2019) 3–15 Contents lists available at ScienceDirect Advanced Drug Delivery Reviews journal homepage: www.elsevier.com/locate/addr Therapeutic medications against diabetes: What we have and what we expect Cheng Hu a,b, Weiping Jia a,⁎ a Shanghai Diabetes Institute, Shanghai Key Laboratory of Diabetes Mellitus, Shanghai Key Clinical Center for Metabolic Diseases, Shanghai Jiao Tong University Affiliated Sixth People's Hospital, 600 Yishan Road, Shanghai 200233, People's Republic of China b Shanghai Jiao Tong University Affiliated Sixth People's Hospital South Campus, 6600 Nanfeng Road, Shanghai 200433, People's Republic of China article info abstract Article history: Diabetes has become one of the largest global health and economic burdens, with its increased prevalence and Received 28 June 2018 high complication ratio. Stable and satisfactory blood glucose control are vital to reduce diabetes-related compli- Received in revised form 1 September 2018 cations. Therefore, continuous attempts have been made in antidiabetic drugs, treatment routes, and traditional Accepted 27 November 2018 Chinese medicine to achieve better disease control. New antidiabetic drugs and appropriate combinations of Available online 5 December 2018 these drugs have increased diabetes control significantly. Besides, novel treatment routes including oral antidia- betic peptide delivery, nanocarrier delivery system, implantable drug delivery system are also pivotal for diabetes Keywords: fi Diabetes control, with its greater ef ciency, increased bioavailability, decreased toxicity and reduced dosing frequency. Treatment Among these new routes, nanotechnology, artificial pancreas and islet cell implantation have shown great poten- Drug delivery tial in diabetes therapy. Traditional Chinese medicine also offer new options for diabetes treatment. -

Iron Transport Proteins: Gateways of Cellular and Systemic Iron Homeostasis
Iron transport proteins: Gateways of cellular and systemic iron homeostasis Mitchell D. Knutson, PhD University of Florida Essential Vocabulary Fe Heme Membrane Transport DMT1 FLVCR Ferroportin HRG1 Mitoferrin Nramp1 ZIP14 Serum Transport Transferrin Transferrin receptor 1 Cytosolic Transport PCBP1, PCBP2 Timeline of identification in mammalian iron transport Year Protein Original Publications 1947 Transferrin Laurell and Ingelman, Acta Chem Scand 1959 Transferrin receptor 1 Jandl et al., J Clin Invest 1997 DMT1 Gunshin et al., Nature; Fleming et al. Nature Genet. 1999 Nramp1 Barton et al., J Leukocyt Biol 2000 Ferroportin Donovan et al., Nature; McKie et al., Cell; Abboud et al. J. Biol Chem 2004 FLVCR Quigley et al., Cell 2006 Mitoferrin Shaw et al., Nature 2006 ZIP14 Liuzzi et al., Proc Natl Acad Sci USA 2008 PCBP1, PCBP2 Shi et al., Science 2013 HRG1 White et al., Cell Metab DMT1 (SLC11A2) • Divalent metal-ion transporter-1 • Former names: Nramp2, DCT1 Fleming et al. Nat Genet, 1997; Gunshin et al., Nature 1997 • Mediates uptake of Fe2+, Mn2+, Cd2+ • H+ coupled transporter (cotransporter, symporter) • Main roles: • intestinal iron absorption Illing et al. JBC, 2012 • iron assimilation by erythroid cells DMT1 (SLC11A2) Yanatori et al. BMC Cell Biology 2010 • 4 different isoforms: 557 – 590 a.a. (hDMT1) Hubert & Hentze, PNAS, 2002 • Function similarly in iron transport • Differ in tissue/subcellular distribution and regulation • Regulated by iron: transcriptionally (via HIF2α) post-transcriptionally (via IRE) IRE = Iron-Responsive Element Enterocyte Lumen DMT1 Fe2+ Fe2+ Portal blood Enterocyte Lumen DMT1 Fe2+ Fe2+ Fe2+ Fe2+ Ferroportin Portal blood Ferroportin (SLC40A1) • Only known mammalian iron exporter Donovan et al., Nature 2000; McKie et al., Cell 2000; Abboud et al. -

(Glut1ds): Methylxanthines Potentiate GLUT1 Haploinsufficiency in Vitro
0031-3998/01/5002-0254 PEDIATRIC RESEARCH Vol. 50, No. 2, 2001 Copyright © 2001 International Pediatric Research Foundation, Inc. Printed in U.S.A. Glucose Transporter Type 1 Deficiency Syndrome (Glut1DS): Methylxanthines Potentiate GLUT1 Haploinsufficiency In Vitro YUAN-YUAN HO, HONG YANG, JÖRG KLEPPER, JORGE FISCHBARG, DONG WANG, AND DARRYL C. DE VIVO Department of Neurology, Columbia University, New York, New York 10032, U.S.A. [Y.Y.H., H.Y., D.W., D.C.D.]; Department of Pediatrics, University of Essen, Essen, Germany 45122 [J.K.]; and Departments of Physiology and Cellular Biophysics, and Ophthalmology, Columbia University, New York, New York 10032, U.S.A. [J.F.] ABSTRACT Methylxanthines such as caffeine and theophylline are known substrate for Glut1. The combined effects of caffeine (3 mM) and to inhibit glucose transport. We have studied such inhibition in phenobarbital (10 mM) on glucose transport, as determined in the glucose transporter type 1 deficiency syndrome (Glut1DS) by patient 15 and the maternal control, show no additive or syner- erythrocyte glucose transport assays. Data from four patients gistic inhibition. These data indicate that caffeine and phenobar- with individual mutations in the GLUT1 gene are discussed: bital have similar Glut1 inhibitory properties in these two sub- patient 1 (hemizygosity), 3 (S66F), 15 (368Ins23), and 17 jects. Our study suggests that Glut1DS patients may have a (R333W). Zero-trans influx of 14C-labeled 3-O-methyl glucose reduced safety margin for methylxanthines. Consumption of (3-OMG) into erythrocytes of patients is reduced (patient 1, 51%; methylxanthine-containing products may aggravate the neuro- 3, 45%; 15, 31%; 17, 52%) compared with maternal controls. -

Cystine–Glutamate Antiporter Xct Deficiency Suppresses Tumor Growth While Preserving Antitumor Immunity
Cystine–glutamate antiporter xCT deficiency suppresses tumor growth while preserving antitumor immunity Michael D. Arensmana, Xiaoran S. Yanga, Danielle M. Leahya, Lourdes Toral-Barzaa, Mary Mileskia, Edward C. Rosfjorda, Fang Wanga, Shibing Dengb, Jeremy S. Myersa, Robert T. Abrahamb, and Christina H. Enga,1 aOncology Research & Development, Pfizer, Pearl River, NY 10965; and bOncology Research & Development, Pfizer, San Diego, CA 92121 Edited by William G. Kaelin Jr., Dana-Farber Cancer Institute and Brigham and Women’s Hospital, Harvard Medical School, Boston, MA, and approved April 2, 2019 (received for review September 1, 2018) T cell-invigorating cancer immunotherapies have near-curative Thus, tumor cells may rely on xCT to fulfill the majority of their potential. However, their clinical benefit is currently limited, as cysteine and GSH needs by importing cystine. only a fraction of patients respond, suggesting that these regimens Inhibition of xCT has been investigated as a therapeutic may benefit from combination with tumor-targeting treatments. As strategy for cancer based on observations that elevated xCT ex- oncogenic progression is accompanied by alterations in metabolic pression on tumor cells correlates with poor prognosis (10–12) pathways, tumors often become heavily reliant on antioxidant and that inhibition of xCT in preclinical studies suppresses tumor machinery and may be susceptible to increases in oxidative stress. growth (10, 12–14). However, these studies relied heavily on the The cystine–glutamate antiporter xCT is frequently overexpressed in use of sulfasalazine, a clinical compound used for the treatment cancer and fuels the production of the antioxidant glutathione; thus, of rheumatoid arthritis, ulcerative colitis, and Crohn’s disease. -

Natural Products As Lead Compounds for Sodium Glucose Cotransporter (SGLT) Inhibitors
Reviews Natural Products as Lead Compounds for Sodium Glucose Cotransporter (SGLT) Inhibitors Author ABSTRACT Wolfgang Blaschek Glucose homeostasis is maintained by antagonistic hormones such as insulin and glucagon as well as by regulation of glu- Affiliation cose absorption, gluconeogenesis, biosynthesis and mobiliza- Formerly: Institute of Pharmacy, Department of Pharmaceu- tion of glycogen, glucose consumption in all tissues and glo- tical Biology, Christian-Albrechts-University of Kiel, Kiel, merular filtration, and reabsorption of glucose in the kidneys. Germany Glucose enters or leaves cells mainly with the help of two membrane integrated transporters belonging either to the Key words family of facilitative glucose transporters (GLUTs) or to the Malus domestica, Rosaceae, Phlorizin, flavonoids, family of sodium glucose cotransporters (SGLTs). The intesti- ‑ SGLT inhibitors, gliflozins, diabetes nal glucose absorption by endothelial cells is managed by SGLT1, the transfer from them to the blood by GLUT2. In the received February 9, 2017 kidney SGLT2 and SGLT1 are responsible for reabsorption of revised March 3, 2017 filtered glucose from the primary urine, and GLUT2 and accepted March 6, 2017 GLUT1 enable the transport of glucose from epithelial cells Bibliography back into the blood stream. DOI http://dx.doi.org/10.1055/s-0043-106050 The flavonoid phlorizin was isolated from the bark of apple Published online April 10, 2017 | Planta Med 2017; 83: 985– trees and shown to cause glucosuria. Phlorizin is an inhibitor 993 © Georg Thieme Verlag KG Stuttgart · New York | of SGLT1 and SGLT2. With phlorizin as lead compound, specif- ISSN 0032‑0943 ic inhibitors of SGLT2 were developed in the last decade and some of them have been approved for treatment mainly of Correspondence type 2 diabetes. -

Myricetin Antagonizes Semen-Derived Enhancer of Viral Infection (SEVI
Ren et al. Retrovirology (2018) 15:49 https://doi.org/10.1186/s12977-018-0432-3 Retrovirology RESEARCH Open Access Myricetin antagonizes semen‑derived enhancer of viral infection (SEVI) formation and infuences its infection‑enhancing activity Ruxia Ren1,2†, Shuwen Yin1†, Baolong Lai2, Lingzhen Ma1, Jiayong Wen1, Xuanxuan Zhang1, Fangyuan Lai1, Shuwen Liu1* and Lin Li1* Abstract Background: Semen is a critical vector for human immunodefciency virus (HIV) sexual transmission and harbors seminal amyloid fbrils that can markedly enhance HIV infection. Semen-derived enhancer of viral infection (SEVI) is one of the best-characterized seminal amyloid fbrils. Due to their highly cationic properties, SEVI fbrils can capture HIV virions, increase viral attachment to target cells, and augment viral fusion. Some studies have reported that myri- cetin antagonizes amyloid β-protein (Aβ) formation; myricetin also displays strong anti-HIV activity in vitro. Results: Here, we report that myricetin inhibits the formation of SEVI fbrils by binding to the amyloidogenic region of the SEVI precursor peptide (PAP248–286) and disrupting PAP248–286 oligomerization. In addition, myricetin was found to remodel preformed SEVI fbrils and to infuence the activity of SEVI in promoting HIV-1 infection. Moreover, myricetin showed synergistic efects against HIV-1 infection in combination with other antiretroviral drugs in semen. Conclusions: Incorporation of myricetin into a combination bifunctional microbicide with both anti-SEVI and anti- HIV activities is a highly promising approach to preventing sexual transmission of HIV. Keywords: HIV, Myricetin, Amyloid fbrils, SEVI, Synergistic antiviral efects Background in vivo because they facilitate virus attachment and inter- Since the frst cases of acquired immune defciency nalization into cells [4]. -

Effect of Hydrolyzable Tannins on Glucose-Transporter Expression and Their Bioavailability in Pig Small-Intestinal 3D Cell Model
molecules Article Effect of Hydrolyzable Tannins on Glucose-Transporter Expression and Their Bioavailability in Pig Small-Intestinal 3D Cell Model Maksimiljan Brus 1 , Robert Frangež 2, Mario Gorenjak 3 , Petra Kotnik 4,5, Željko Knez 4,5 and Dejan Škorjanc 1,* 1 Faculty of Agriculture and Life Sciences, University of Maribor, Pivola 10, 2311 Hoˇce,Slovenia; [email protected] 2 Veterinary Faculty, Institute of Preclinical Sciences, University of Ljubljana, Gerbiˇceva60, 1000 Ljubljana, Slovenia; [email protected] 3 Center for Human Molecular Genetics and Pharmacogenomics, Faculty of Medicine, University of Maribor, Taborska 8, 2000 Maribor, Slovenia; [email protected] 4 Department of Chemistry, Faculty of Medicine, University of Maribor, Taborska 8, 2000 Maribor, Slovenia; [email protected] (P.K.); [email protected] (Ž.K.) 5 Laboratory for Separation Processes and Product Design, Faculty of Chemistry and Chemical Engineering, University of Maribor, Smetanova 17, 2000 Maribor, Slovenia * Correspondence: [email protected]; Tel.: +386-2-320-90-25 Abstract: Intestinal transepithelial transport of glucose is mediated by glucose transporters, and affects postprandial blood-glucose levels. This study investigates the effect of wood extracts rich in hydrolyzable tannins (HTs) that originated from sweet chestnut (Castanea sativa Mill.) and oak (Quercus petraea) on the expression of glucose transporter genes and the uptake of glucose and HT constituents in a 3D porcine-small-intestine epithelial-cell model. The viability of epithelial cells CLAB and PSI exposed to different HTs was determined using alamarBlue®. qPCR was used to analyze the gene expression of SGLT1, GLUT2, GLUT4, and POLR2A. Glucose uptake was confirmed Citation: Brus, M.; Frangež, R.; by assay, and LC–MS/ MS was used for the analysis of HT bioavailability. -

Expression of SLC2A9 Isoforms in the Kidney and Their Localization in Polarized Epithelial Cells
Expression of SLC2A9 Isoforms in the Kidney and Their Localization in Polarized Epithelial Cells Toru Kimura1, Michi Takahashi1, Kunimasa Yan2, Hiroyuki Sakurai1* 1 Department of Pharmacology and Toxicology, Kyorin University School of Medicine, Mitaka, Tokyo, Japan, 2 Department of Pediatrics, Kyorin University School of Medicine, Mitaka, Tokyo, Japan Abstract Background: Many genome-wide association studies pointed out that SLC2A9 gene, which encodes a voltage-driven urate transporter, SLC2A9/GLUT9 (a.k.a. URATv1), as one of the most influential genes for serum urate levels. SLC2A9 is reported to encode two splice variants: SLC2A9-S (512 amino acids) and SLC2A9-L (540 amino acids), only difference being at their N- termini. We investigated isoform-specific localization of SLC2A9 in the human kidney and role of N-terminal amino acids in differential sorting in vitro. Methodology/Principal Findings: Isoform specific antibodies against SLC2A9 were developed and human kidney sections were stained. SLC2A9-S was expressed in the apical side of the collecting duct while SLC2A9-L was expressed in the basolateral side of the proximal tubule. GFP fused SLC2A9s were expressed in MDCK cells and intracellular localization was observed. SLC2A9-S was expressed at both apical and basolateral membranes, whereas SLC2A9-L was expressed only at the basolateral membrane. Although SLC2A9-L has a putative di-leucine motif at 33th and 34th leucine, deletion of the motif or replacement of leucine did not affect its subcellular localization. When up to 16 amino acids were removed from the N- terminal of SLC2A9-S or when up to 25 amino acids were removed from the N-terminal of SLC2A9-L, there was no change in their sorting. -
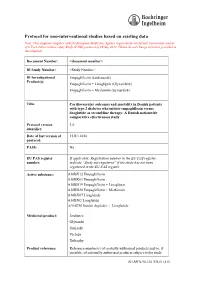
Protocol for Non-Interventional Studies Based on Existing Data
ABCD TITLE PAGE Protocol for non-interventional studies based on existing data TITLE PAGE Note: This template complies with the European Medicines Agency requirements on format, layout and content of a Post Authorisation safety Study (PASS) protocol of 26 Sep 2012. Please do not change structure provided in this template. Document Number: <document number> BI Study Number: <Study Number> BI Investigational Empagliflozin (Jardiance®) Product(s): Empagliflozin + Linagliptin (Glyxambi®) Empagliflozin + Metformin (Synjardy®) Title: Cardiovascular outcomes and mortality in Danish patients with type 2 diabetes who initiate empagliflozin versus liraglutide as second-line therapy: A Danish nationwide comparative effectiveness study Protocol version 1.0 identifier: Date of last version of 15JUL2018 protocol: PASS: No EU PAS register If applicable: Registration number in the EU PAS register; number: indicate “Study not registered” if the study has not been registered in the EU PAS register Active substance: A10BX12 Empagliflozin A10BK03 Empagliflozin A10BD19 Empagliflozin + Linagliptin A10BD20 Empagliflozin + Metformin A10BX07 Liraglutide A10BJ02 Liraglutide A10AE56 Insulin degludec + Liraglutide Medicinal product: Jardiance Glyxambi Synjardy Victoza Xultophy Product reference: Reference number(s) of centrally authorised products and/or, if possible, of nationally authorised products subject to the study 001-MCS-90-124_RD-01 (4.0) Boehringer Ingelheim Page 2 of 55 Protocol for non-interventional studies based on existing data BI Study Number <Study Number> <document number> Proprietary confidential information © 2019 Boehringer Ingelheim International GmbH or one or more of its affiliated companies Procedure number: If applicable, Agency or national procedure number(s), e.g. EMA/X/X/XXX Joint PASS: No Research question and To compare, among patients with type 2 diabetes in Denmark, objectives: clinical outcomes among new users (initiators) of empagliflozin versus liraglutide. -

2.1 Drosophila Melanogaster
Overend, Gayle (2010) Drosophila as a model for the Anopheles Malpighian tubule. PhD thesis, University of Glasgow. http://theses.gla.ac.uk/1604/ Copyright and moral rights for this thesis are retained by the author A copy can be downloaded for personal non-commercial research or study, without prior permission or charge This thesis cannot be reproduced or quoted extensively from without first obtaining permission in writing from the Author The content must not be changed in any way or sold commercially in any format or medium without the formal permission of the Author When referring to this work, full bibliographic details including the author, title, awarding institution and date of the thesis must be given Glasgow Theses Service http://theses.gla.ac.uk/ [email protected] Drosophila as a model for the Anopheles Malpighian tubule A thesis submitted for the degree of Doctor of Philosophy at the University of Glasgow Gayle Overend Integrative and Systems Biology Faculty of Biomedical and Life Sciences University of Glasgow Glasgow G11 6NU UK August 2009 2 The research reported within this thesis is my own work except where otherwise stated, and has not been submitted for any other degree. Gayle Overend 3 Abstract The insect Malpighian tubule is involved in osmoregulation, detoxification and immune function, physiological processes which are essential for insect development and survival. As the Malpighian tubules contain many ion channels and transporters, they could be an effective tissue for targeting with novel pesticides to control populations of Diptera. Many of the insecticide compounds used to control insect pest species are no longer suited to their task, and so new means of control must be found.