Manual for Sputum Smear Fluorescence Microscopy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

TB Auramine-Rhodamine PRODUCT DETERIORATION
Directions should be read and followed carefully. Refer to Material Safety Data Sheet for additional information. STORAGE This product is ready for use and no further preparation is necessary. Store product in its original container at 20-25°C until used. TB Auramine-Rhodamine PRODUCT DETERIORATION INTENDED USE This product should not be used if (1) the color has changed Remel TB Auramine-Rhodamine is a stain recommended for from a red, clear liquid, (2) the expiration date has passed, or use in qualitative procedures in the fluorescent microscopic (3) there are other signs of deterioration. detection of mycobacteria. SPECIMEN COLLECTION, STORAGE AND TRANSPORT Specimens should be collected and handled following SUMMARY AND EXPLANATION 5 recommended guidelines. One of the earliest methods devised for the detection of tubercle bacilli is the microscopic staining technique.1 MATERIALS REQUIRED BUT NOT SUPPLIED Mycobacteria possess cell walls that contain mycolic acid (1) Loop sterilization device, (2) Inoculating loop, swab, which complex with dyes resulting in the characteristic known collection containers, (3) Incubators, alternative environmental as “acid-fastness.” Acid-fast microscopy is the most rapid, TM systems, (4) Supplemental media, (5) QC-Slide AFB Stain initial step in diagnosis and in providing information about the Control (REF 40146) or quality control organisms, (6) TB number of acid-fast bacilli present. The use of fluorescent Decolorizer (Truant-Moore) (REF 40107), (7) TB Potassium dyes for the detection of acid-fast bacilli in clinical specimens 2 Permanganate (REF 40092), (8) Demineralized water, was described by Hagemann in 1937. In 1962, Truant, Brett, (9) Glass slides, (10) Bunsen burner or slide warmer, and Thomas evaluated the usefulness of the fluorescent (11) Microscope, (12) Immersion oil. -

QBC F.A.S.T. Auramine O Stain
QBC F.A.S.T.TM Auramine O Stain Kit Instruction Manual 4277-400-053 Rev. I Revised 2018-11-20 English QBC F.A.S.T.TM Auramine O Stain Kit Intended Use For use as a stain for smears made from patient specimens or cultures in the detection or characterization of acid fast bacilli such as Mycobacterium tuberculosis. Summary and Principles The worldwide incidence of tuberculosis has been on an increasing trend since at least 1990, when the World Health Organization began tracking incidence data1. Early and accurate detection of tuberculosis is critical for both effective control and treatment of the disease. The most common method for detection of Mycobacterium tuberculosis is the use of sputum smear microscopy1, which can provide both an initial presumptive diagnosis as well as a quantification of the mycobacterial load. Acid fast bacilli, such as Mycobacterium tuberculosis, can be stained by aniline dyes and are resistant to decolorization by acid and alcohol. When followed by a counterstain, this treatment results in the acid fast bacilli staining with contrast to other organisms and debris that have retained only the counterstain. However, the staining methods classically used for acid fast microscopy result in a smear that can be difficult and time consuming to read. Auramine O and auramine-rhodamine stains have been successfully used for fluorescence based microscopy of mycobacteria. Reports of mechanism of staining are conflicting; these include Auramine O binding to the cell wall of the mycobacteria2 and the stain binding 1 to “most if not all” the Auramine O binding to the nucleic acid in the mycobacteria3. -

Auramine O C.I. 41000
AURAMINE O C.I. 41000 IVD In vitro diagnostic medical device Basic Yellow 2, BSC certified stain For staining acid-fast lung tissue bacteria acc. to Truant INSTRUCTIONS FOR USE REF Product code: AU-P-25 (25 g) Introduction Histology, cytology and other related scientific disciplines study the microscopic anatomy of tissues and cells. In order to achieve a good tissue and cellular structure, the samples need to be stained in a correct manner. Auramine O powder dye is used in various staining methods in microscopy. It is used in clinical microbiology and histology for detecting tuberculosis Mycobacteria and other acid-fast bacteria. Staining using Auramine O is a fluorescent method of visualizing acid-fast bacteria. Mycobacteria are difficult to stain due to high amount of lipids and wax in their cellular membranes. When stained using Auramine O dye, acid-fast mycobactera retain the dye even when exposed to strong destaining solutions, such as HCl-ethanol. Product description AURAMINE O - Biological Stain Commission (BSC) certified powder dye for preparing solution for detecting Mycobacterium tuberculosis and other acid-fast bacteria Other preparations and reagents used in preparing the dye solution: Microscopy powder dyes, such as BioGnost's Rhodamine B dye (product code RHB-P-25) Phenol (C6H5OH) Glycerol (C3H5(OH)3) Preparing the solutions for staining Auramine O-Rhodamine B staining solution: Dissolve by mixing 3 g of Auramine O powder dye adn 1.5 g of Rhodamine B powder dye in 150 ml of glycerol at room temperature. Add 20 ml of molten phenol (at 45oC) and 100 ml of distilled/demineralized water After mixing, filter through glass wool Results Tb bacterija (ARB) - red or greenish fluorescence Background - dark Note The mentioned formulation is only one of the ways of preparing the dye solution. -
Application of Taguchi Method and Response Surface Methodology Into
www.nature.com/scientificreports OPEN Application of Taguchi method and response surface methodology into the removal of malachite green and auramine‑O by NaX nanozeolites Siroos Shojaei1*, Saeed Shojaei2, Shahab S. Band3*, Amir Abbas Kazemzadeh Farizhandi4, Milad Ghoroqi5 & Amir Mosavi6 In the present study, the simultaneous removal of malachite green (MG) and auramine‑O (AO) dyes from the aqueous solution by NaX nanozeolites in a batch system is investigated. Taguchi method and response surface methodology (RSM) were used to optimize and model dye removal conditions. In order to do so, the efect of various factors (dyes concentration, sonication time, ionic strength, adsorbent dosage, temperature, and pH of the solution) on the amount of dye removal was evaluated by the Taguchi method. Then, the most important factors were chosen and modeled by the RSM method so as to reach the highest percentage of dye removal. The proposed quadratic models to remove both dyes were in good accordance with the actual experimental data. The maximum removal efciencies of MG and AO dyes in optimal operating conditions were 99.07% and 99.61%, respectively. Also, the coefcients of determination (R2) for test data were 0.9983 and 0.9988 for MG and AO dyes, respectively. The reusability of NaX nanozeolites was evaluated during the adsorption process of MG and AO. The results showed that the adsorption efciency decreases very little up to fve cycles. Moreover, NaX nanozeolites were also applied as adsorbents to remove MG and AO from environmental water samples, and more than 98.1% of both dyes were removed from the solution in optimal conditions. -

L003568.C -- Auramine O Stain Sets.Pdf
[+1] 800.221.6058 United States Directions For Use for the following: [+1] 360.260.2779 International Auramine O Fluorescent Stain Set with Potassium Permanganate, Auramine O Fluorescent Stain Set with Thiazine Red, Auramine O Fluorescent Stain, TB Fluorescent Decolorizer, Potassium Permanganate Counterstain, Thiazine Red Counterstain INTENDED USE SPECIMEN PROCESSING Alpha-Tec Systems, Inc. Auramine O Fluorescent Stain Set with 1. Make a thin smear of the specimen over an area of 2-3 sq cm. Heat Potassium Permanganate, Auramine O Fluorescent Stain Set with fix by warming on a slide warmer (65-75ºC) for 10 minutes, or until Thiazine Red, and components are recommended for use in qualitative the smear is dry. If a Bunsen burner is used, pass the slide slowly procedures for the fluorescent microscopic detection of mycobacteria. 3 times over its cone of heat. Do not scorch. 2. Flood the smear with Auramine O Fluorescent Stain for 15 minutes. SUMMARY 3. Rinse with deionized or distilled water and drain. One of the earliest methods devised for the detection of the tubercle 4. Decolorize with TB Fluorescent Decolorizer for 2-3 minutes. bacillus is the microscopic staining technique. Mycolic acid within the 5. Rinse with deionized or distilled water and drain. mycobacteria cell wall interacts with dyes resulting in the characteristics 6. Flood smear with Potassium Permanganate or Thiazine Red known as “acid-fastness”. Acid-fast microscopy is the most rapid, initial Counterstain for 2-4 minutes, no longer. step in diagnosis and provides information about the number of acid-fast 7. Rinse with deionized or distilled water and allow to air-dry. -

AFB Smear Microscopy
AFB Smear Microscopy 1 Terminology • AFB Smear Microscopy: Microscopic examination of specially stained smears to detect acid-fast organisms such as Mycobacterium tuberculosis and non- tuberculous mycobacteria (NTM) • Acid Fast Bacilli (AFB): organisms (including mycobacteria) that resist decolorization with acid alcohol due to the lipid-rich mycolic acids in the cell wall thereby retaining the primary stain 2 Terminology • Processing: digestion, decontamination, and/or concentration of a primary patient specimen prior to setting up culture and smear • Smear: A small amount of primary patient specimen (direct or processed) is placed on a slide for the purpose of microscopic examination 3 AFB Microscopy • Examination of smears is a rapid, convenient and inexpensive test • All types of specimens can be evaluated – sputum, tissue, body fluids, etc. • Positive AFB smear results provide a first indication of mycobacterial infection and potential TB disease • Must be accompanied by additional testing including culture for confirmatory diagnosis 4 AFB Microscopy Results Guide Decisions • Clinical management – Patient therapy may be initiated for TB based on smear result and clinical presentation – Changes in smear status important for monitoring response to therapy • Laboratory testing – Algorithms for use of nucleic acid amplification tests are often based on smear positivity • Public health interventions – Smear status and grade useful for identifying the most infectious cases – Contact investigations prioritized based on smear result – Decisions regarding respiratory isolation based on smear result 5 Smear-positive TB Cases • Smear-positivity and grade indicates relative bacterial burden and correlates with disease presentation • Patients that are sputum smear-positive are 5–10 times more infectious than smear negative patients • Untreated or treated with an inappropriate regimen, a sputum smear-positive patient may infect 10-15 persons/year 6 Sputum Smear Results • In 2010, 43% of pulmonary TB cases in the U.S. -
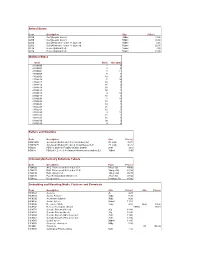
Discontinued List to Go on Website
Animal Serum Code Description Size Price £ G210 Calf (Aseptic Donor) 100ml 13.90 G250 Calf (Aseptic Donor) 500ml 38.60 G212 Calf (Newborn) - under 14 days old 100ml 5.65 G252 Calf (Newborn) - under 14 days old 500ml 22.30 G610 Horse (Natural Clot) 100ml 7.80 G650 Horse (Natural Clot) 500ml 31.90 Multitest Slides Code Wells Size (mm) 61100-00 1 8 61100-01 3 8 61100-04 3 14 61100-05 8 6 61100-09 10 8 61100-10 2 10 61100-11 10 5 61100-12 36 2 61100-14 10 6 61100-16 10 7 61100-18 4 14 61100-19 12 8 61100-24 1 18 61100-25 15 4 61100-26 14 5 61100-28 21 4 61100-29 12 6 61100-30 3 11 61100-33 12 3 61100-36 18 5 61100-50 30 3 61100-60 4 6 Buffers and Solutions Code Description Size Price £ HDS15/25 Sorensen's Buffer pH 6.5 (1 vial makes 5L) 25 vials 35.00 HDS20/25 Sorensen's Buffer pH 7.0-7.6 (1 vial makes 5L)* 25 vials 36.75 HDS25 PBS for Osmotic Fragility (makes 250ml) 25ml 2.65 HDS35 PBS pH 7.2 or 7.6 for Immunofluorescence (makes 2L) 100ml 3.40 Immunocytochemistry Substrate Tablets Code Description Pack Price £ HD4190 AEC Effervescent Buffered pH 5.1 5mg x 50 44.80 HD4170 DAB Effervescent Buffered pH 7.0 10mg x 50 63.10 HD4240 DAB Unbuffered 10mg x 50 55.20 HD4120 Fast Red Standard Unbuffered 2mg x 50 47.90 HD4360 Ureaperoxide 5.68mg x 50 65.80 Embedding and Mounting Media, Fixatives and Chemicals Code Description Size Price £ Size Price £ HC8503 Acetone 2L 4.25 HC8510 Acacia Powder 100g 5.35 HC8520 Aluminium Sulphate 500g 4.20 HC8530 Aniline Xylene 500ml 11.15 HC8540 Beeswax - White 100g 4.10 500g 14.30 HC8542 Berlese Fluid (gum chloral) -

AURAMINE and AURAMINE PRODUCTION 1. Exposure Data
AURAMINE AND AURAMINE PRODUCTION 1. Exposure Data 1.1 Chemical and Physical Data 1.1.1 Nomenclature Auramine Chem. Abstr. Serv. Reg. No.: 492–80–8 CAS Name: 4,4'-Carbonimidoylbis[N,N-dimethylbenzenamine] Synonyms: C.I. 41000B; C.I. Solvent Yellow 34; 4,4'- dimethylaminobenzophenonimide; 4,4'-(imidocarbonyl)bis(N,N-dimethylaniline); glauramine; Solvent Yellow 34; yellow pyoctanine Auramine hydrochloride Chem. Abstr. Serv. Reg. No.: 2465–27–2 CAS Name: 4,4'-Carbonimidoylbis[N,N-dimethylbenzenamine], hydrochloride (1:1) Synonyms: Auramine chloride; 4,4'-carbonimidoylbis[N,N-dimethylbenzenamine], monohydrochloride; C.I. 41000; C.I. Basic Yellow 2; C.I. Basic Yellow 2, monohydrochloride Michler’s base Chem. Abstr. Serv. Reg. No.: 101-6-1 CAS Name: 4,4'-Methylenebis(N,N-dimethyl)benzenamine Synonyms: 4,4’-methylenebis(N,N-dimethyl) aniline; tetramethyldiaminodiphenylmethane; 4,4’-bis(dimethylamino) diphenylmethane; tetra base; methane base; Michler’s hydride; Michler's methane Use: 4,4’-Methylenebis(N,N-dimethyl)benzenamine (Michler’s base) is an intermediate in the synthesis of several organic dyes, e.g., auramine. –111– 112 IARC MONOGRAPHS VOLUME 99 Michler's ketone Chem. Abstr. Serv. Reg. No.: 90-94-8 CAS Name: Bis[4-(dimethylamino)phenyl]methanone. Synonyms: 4,4'-bis(dimethylamino)benzophenone; p,p'-bis(dimethylamino)benzophenone; bis[p-(N,N′-dimethylamino)phenyl]ketone; tetramethyldiaminobenzophenone Use: Bis[4-(dimethylamino)phenyl]methanone (Michler’s ketone) is a chemical intermediate used in the synthesis of a number of dyes and pigments, particularly auramine derivatives. It is a hydrolysis product of auramine. 1.1.2 Structural formula, molecular formula, and relative molecular mass Auramine NH H3C CH3 N N CH3 CH3 C17H21N3 Rel. -

Fluorescence Microscopy of Tubercle Bacilli Stained with Auramine and Rhodamine J
Henry Ford Hospital Medical Journal Volume 10 | Number 2 Article 2 6-1962 Fluorescence Microscopy Of Tubercle Bacilli Stained With Auramine And Rhodamine J. P. Truant W. A. Brett W. Thomas Jr. Follow this and additional works at: https://scholarlycommons.henryford.com/hfhmedjournal Part of the Life Sciences Commons, Medical Specialties Commons, and the Public Health Commons Recommended Citation Truant, J. P.; Brett, W. A.; and Thomas, W. Jr. (1962) "Fluorescence Microscopy Of Tubercle Bacilli Stained With Auramine And Rhodamine," Henry Ford Hospital Medical Bulletin : Vol. 10 : No. 2 , 287-296. Available at: https://scholarlycommons.henryford.com/hfhmedjournal/vol10/iss2/2 This Article is brought to you for free and open access by Henry Ford Health System Scholarly Commons. It has been accepted for inclusion in Henry Ford Hospital Medical Journal by an authorized editor of Henry Ford Health System Scholarly Commons. For more information, please contact [email protected]. Henry Ford Hosp. Med. Bull. Vol. 10, June, 1962 FLUORESCENCE MICROSCOPY OF TUBERCLE BACILLI STAINED WITH AURAMINE AND RHODAMINE TRUANT, J.P.,* BRETT, W.A.* AND THOMAS, W., JR.** THE IDENTIFICATION OF Mycobacterium tuberculosis in clinical specimens is one of the most tedious tasks confronting both the bacteriologist and pathologist. It is well known that the detection of acid-fast organisms is extremely difficult in conventionally stained smears especially when they contain only a few tubercle bacilli. Therefore, a method which is capable of detecting this pathogen more readily would certainly be of considerable value. Such a procedure has been discussed in the past but, although previously tried by us and many others, has not been widely accepted. -

L003565.C -- Auramine O Rhodamine B Stain Set.Pdf
[+1] 800.221.6058 United States Directions For Use for the following: [+1] 360.260.2779 International Auramine O/Rhodamine B Fluorescent Stain Set, Auramine O/Rhodamine B Fluorescent Stain, TB Fluorescent Decolorizer, Potassium Permanganate Counterstain INTENDED USE SPECIMEN PROCESSING Alpha-Tec Systems, Inc. Auramine O Fluorescent Stain Set and 1. Make a thin smear of the specimen over an area of 2-3 sq cm. Heat components are recommended for use in qualitative procedures for the fix by warming on a slide warmer (65-75ºC) for 10 minutes, or until fluorescent microscopic detection of mycobacteria. the smear is dry. If a Bunsen burner is used, pass the slide slowly 3 times over its cone of heat. Do not scorch. SUMMARY 2. Flood the smear with Auramine O Fluorescent Stain for 15 minutes. One of the earliest methods devised for the detection of the tubercle 3. Rinse with deionized or distilled water and drain. bacillus is the microscopic staining technique. Mycolic acid within the 4. Decolorize with TB Fluorescent Decolorizer for 2-3 minutes. mycobacteria cell wall interacts with dyes resulting in the characteristics 5. Rinse with deionized or distilled water and drain. known as “acid-fastness”. Acid-fast microscopy is the most rapid, initial 6. Flood smear with Potassium Permanganate Counterstain for 2-4 step in diagnosis and provides information about the number of acid-fast minutes, no longer. bacilli present. Hagermann described the use of fluorescent dyes for the 7. Rinse with deionized or distilled water and allow to air-dry. detection of acid-fast bacilli in clinical specimens. -

Auramine O Stain
AURAMINE O STAIN Preanalytical Considerations I. PRINCIPLE Acid-fast mycobacteria resist decolorization by acid-alcohol after primary staining owing to the high lipid (mycolic acid) content in their cell walls. The identification of mycobacteria with auramine O is due to the affinity of the mycolic acid in the cell walls for the fluorochromes. The dye will bind to the mycobacteria, which appear as bright yellow, luminous rods against a dark background. The potassium permanganate helps prevent non-specific fluorescence. All acid-fast organisms will be stained by auramine O, including some parasites. Slides stained with auramine O may be restained with Ziehl-Neelsen or Kinyoun stain directly, as long as the oil has been removed. This provides a convenient method of confirming and differentiating morphology of positive slides with the traditional stains. The fluorochromes stains are recommended for specimen examination because of their increased sensitivity and speed. II. SPECIMENS Clinical specimens or pure cultures suspected of harboring mycobacteria are stained for acid fastness. A direct smear (not concentrated) from a clinical specimen is discouraged because it lacks the sensitivity of a concentrated (centrifuged) smear. A negative result from a direct smear must be followed by a concentrated smear. Preparation of smear for staining is as follows: A. In the case of a solid medium, an aqueous suspension is made. Take a small amount of material and suspend it in a drop of distilled water on a microscope slide. Do not make the smear too thick. B. In the case of a liquid medium, a drop is used directly from the culture container. -

The Color of Tissue Diagnostics Routine Stains, Special Stains and Ancillary Reagents
The Color of Tissue Diagnostics Routine Stains, Special Stains and Ancillary Reagents The life science business of Merck KGaA, Darmstadt, Germany operates as MilliporeSigma in the U.S. and Canada. For over years, 100routine stains, special stains and ancillary reagents have been part of the MilliporeSigma product range. This tradition and experience has made MilliporeSigma one of the world’s leading suppliers of microscopy products. The products for microscopy, a comprehensive range for classical hematology, histology, cytology, and microbiology, are constantly being expanded and adapted to the needs of the user and to comply with all relevant global regulations. Many of MilliporeSigma’s microscopy products are classified as in vitro diagnostic (IVD) medical devices. Quality Means Trust As a result of MilliporeSigma’s focus on quality control, microscopy products are renowned for excellent reproducibility of results. MilliporeSigma products are manufactured in accordance with a quality management system using raw materials and solvents that meet the most stringent quality criteria. Prior to releasing the products for particular applications, relevant chemical and physical parameters are checked along with product functionality. The methods used for testing comply with international standards. For over Contents Ancillary Reagents Microbiology 3-4 Fixing Media 28-29 Staining Solutions and Kits years, 5-6 Embedding Media 30 Staining of Mycobacteria 100 6 Decalcifiers and Tissue Softeners 30 Control Slides 7 Mounting Media Cytology 8 Immersion