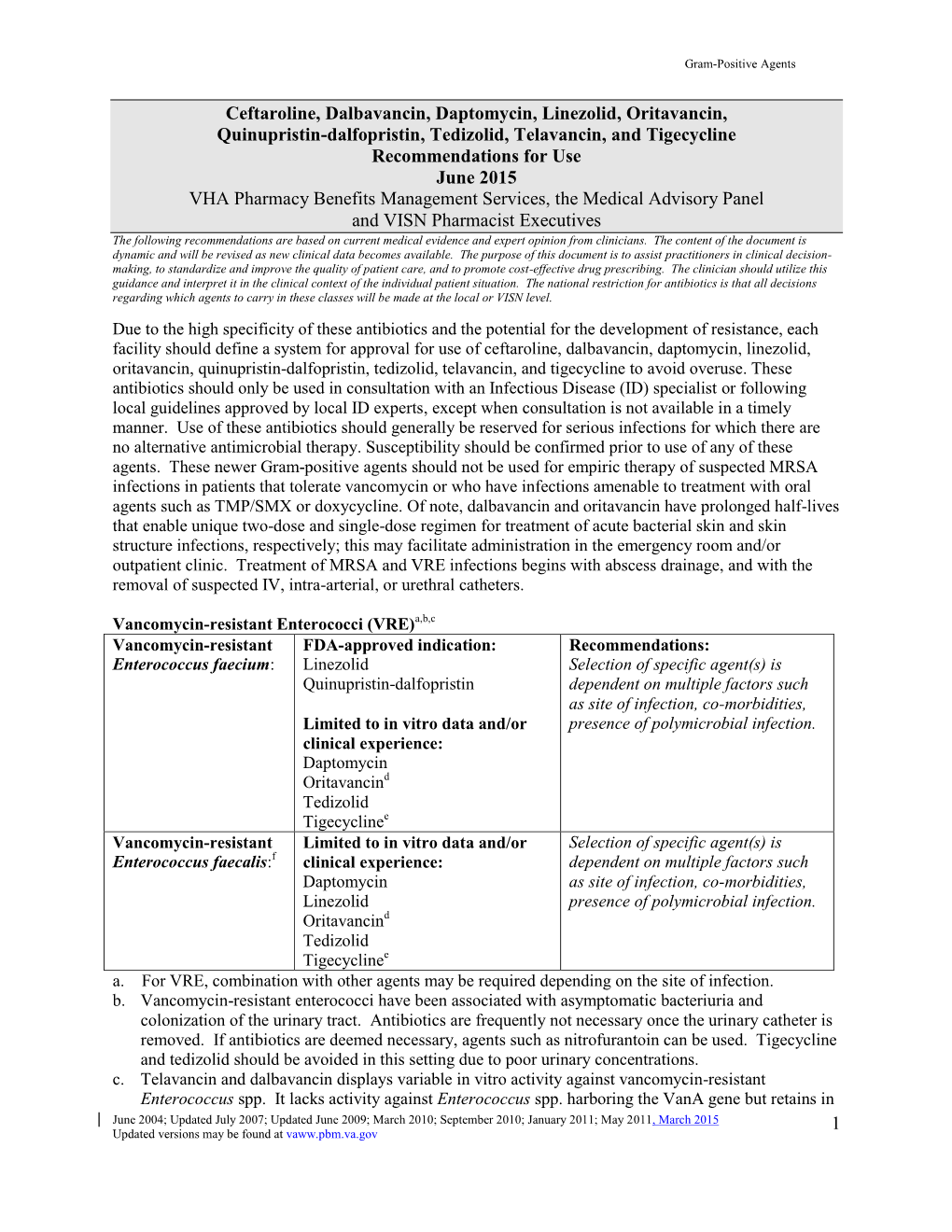
Gram-Positive Recs for Use for Newer MRSA Agents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

P0469 In-Vitro Activity of Oritavancin Against Daptomycin And/Or Linezolid Resistant Enterococcus Faecium Clinical Isolates: a Single Centre Study
P0469 In-vitro activity of oritavancin against daptomycin and/or linezolid resistant Enterococcus faecium clinical isolates: a single centre study Abhay Dhand*1, Nicholas Feola1, Leslie Lee1, Guiqing Wang1 1Westchester Medical Center Background: Oritavancin is a novel antibiotic with potent activity against a broad range of gram- positive organisms. Resistance to daptomycin, linezolid and other antibiotics among enterococcus is on the rise in many US hospitals. Oritavancin may provide an alternative antibiotic therapy for serious infections caused by such very resistant enterococci. The aim of this study was to evaluate in vitro antimicrobial susceptibility of oritavancin against enterococci with focus on Daptomycin non- susceptible (DNSE) and Linezolid resistant (LRE) clinical isolates. Materials/methods: DNSE and LRE clinical isolates were recovered from patients in a tertiary medical center in suburban New York City from May 2015 through December 2016. Daptomycin susceptibility was determined by MicroScan WalkAway™ System and confirmed by E-test. Susceptibility of oritavancin and linezolid was performed by broth microdilution using the Sensititre™ panel in accordance with the guidelines of the Clinical and Laboratory Standards Institute and package insert of the manufacturer. The isolates were confirmed by analysis of 16S rRNA gene sequence or by the MALDI Biobiotyper CA System™. Results: A total of 24 nonduplicate E. faecium clinical isolates were analyzed in this study. 19/24 isolates were DNSE (6-96 μg/ml), 4/24 were LRE (8-16 μg/ml) and 2/24 were both DNSE and LRE. The MIC50 and MIC90 of oritavancin against combined resistant enterococci isolates was 0.06 μg/ml and 0.25 μg/ml (range: 0.008 – 0.25 μg/ml) respectively. -

Use of Ceftaroline Fosamil in Children: Review of Current Knowledge and Its Application
Infect Dis Ther (2017) 6:57–67 DOI 10.1007/s40121-016-0144-8 REVIEW Use of Ceftaroline Fosamil in Children: Review of Current Knowledge and its Application Juwon Yim . Leah M. Molloy . Jason G. Newland Received: November 10, 2016 / Published online: December 30, 2016 Ó The Author(s) 2016. This article is published with open access at Springerlink.com ABSTRACT infections, CABP caused by penicillin- and ceftriaxone-resistant S. pneumoniae and Ceftaroline is a novel cephalosporin recently resistant Gram-positive infections that fail approved in children for treatment of acute first-line antimicrobial agents. However, bacterial skin and soft tissue infections and limited data are available on tolerability in community-acquired bacterial pneumonia neonates and infants younger than 2 months (CABP) caused by methicillin-resistant of age, and on pharmacokinetic characteristics Staphylococcus aureus, Streptococcus pneumoniae in children with chronic medical conditions and other susceptible bacteria. With a favorable and those with invasive, complicated tolerability profile and efficacy proven in infections. In this review, the microbiological pediatric patients and excellent in vitro profile of ceftaroline, its mechanism of action, activity against resistant Gram-positive and and pharmacokinetic profile will be presented. Gram-negative bacteria, ceftaroline may serve Additionally, clinical evidence for use in as a therapeutic option for polymicrobial pediatric patients and proposed place in therapy is discussed. Enhanced content To view enhanced content for this article go to http://www.medengine.com/Redeem/ 1F47F0601BB3F2DD. Keywords: Antibiotic resistance; Ceftaroline J. Yim (&) fosamil; Children; Methicillin-resistant St. John Hospital and Medical Center, Detroit, MI, Staphylococcus aureus; Streptococcus pneumoniae USA e-mail: [email protected] L. -

Dalvance Generic Name: Dalbavancin Manufacturer1: DURATA Therapeutics Drug Class1,2,3,4: Antibiotic
Brand Name: Dalvance Generic Name: dalbavancin Manufacturer1: DURATA therapeutics Drug Class1,2,3,4: Antibiotic Uses: Labeled Uses1: Treatment of adult patients with acute bacterial skin and skin structure infections caused by susceptible isolates of the following Gram-positive microorganisms: Staphylococcus aureus (including methicillin-susceptible and methicillin-resistant strains), Streptococcus pyogenes, Streptococcus agalactiae, Streptococcus anginosus group (including S. anginosus, S. intermedius, S. constellatus) Mechanism of Action:1,2,3,4 This drug is a lipoglycopeptide which binds to the D-alanyl-D-alanine terminus of the stem pentapeptide in nascent cell wall. Through this above mechanism it prevents cross-linking and interferes with cell wall synthesis. Dalbavancin is bactericidal in vitro against Staphylococcus aureus and Streptococcus pyogenes. Pharmacokinetics1,2,3,4 Tmax End of infusion time Vd 7-13L t1/2 346 hours Clearance .0513 l/h Protein binding (albumin) 93% (primarily to albumin) Bioavailability 100% Metabolism1,2,3,4: A minor metabolite- hydroxy-dalbavancin has been observed in the urine of healthy subjects, however quantifiable plasma concentrations have not been observed. Elimination1,2,3,4: Urine (33% as unchanged drug, 12% as hydroxy metabolite) Feces (20%) Efficacy: Boucher HW, Wilcox M, Talbot GH, Puttagunta S, Das AF, Dunne MW. Once-Weekly Dalbavancin versus Daily Conventional Therapy for Skin Infection. N Engl J Med 2014; 370:2169-2179. Study Design: Double blind, double dummy, randomized controlled study Description of Study: Discover 1 and Discover 2 were international, multicenter, randomized trials conducted from 2011 through 2012 at 54 and 86 investigative sites, respectively. The studies had the same design. Patients with acute bacterial skin and skin-structure infection were stratified then randomly assigned to receive dalbavancin intravenously on days 1 and 8 or vancomycin intravenously for at least 3 days with the option to switch to oral linezolid to complete 10 to 14 days of therapy. -

Criteria for Use of Dalbavancin for Acute Bacterial Skin/Soft Tissue Infection (Abssti)
Criteria for Use of Dalbavancin for Acute Bacterial Skin/Soft Tissue Infection (abSSTI) 1. Patients meeting any of the following are NOT ELIGIBLE for dalbavancin therapy: a. History of hypersensitivity reaction to lipoglycopeptide antibiotics (vancomycin, televancin, dalbavancin, oritavancin). b. Patients with acute bacterial skin or skin structure infections such as superficial/simple cellulitis/erysipelas, impetiginous lesion, furuncle, or simple abscess that only requires surgical drainage for cure. c. Infection thought to be caused by gram-negative bacteria d. Infection due to an organism suspected or known to be resistant to dalbavancin or vancomycin 2. For outpatient use (i.e. ED) a. Contact infectious disease for authorization: ABX approval pager (see ON-CALL schedule) b. The following clinical criteria must be met: i. Pre-antibiotic blood cultures must be drawn. ii. Clinical condition expected to require ≥ 24 hours of IV antibiotics – must not qualify for oral antibiotic therapy. iii. Presence of cellulitis, major abscess or a wound infection associated with at least 75cm2 of erythema highly suspected or known to be caused by gram-positive bacteria. iv. The size of the infection must be clearly documented and/or outlined prior to leaving the ED, preferably with a photograph. v. Patient to be discharged to home ± home health (not to skilled nursing facility). c. Required follow up must be set up prior to leaving the ED: i. Must document patient contact info for follow up, preferably reliable cell phone number. ii. Must have follow up within 48-72H with Dr. Turnipseed (916-765-0196) or Rominski. 1. Email patient name, MRN, and phone number. -

Dalbavancin (Dalvance®)
DalbavancinDalbavancin (Dalvance (Dalvance®)®) IV Only Use requires formal ID Consult Activity: Coverage against Staphylococcus aureus (including MSSA and MRSA), Streptococcus pyogenes, Streptococcus agalactiae (Group B Strep.) and Streptococcus anginosus group (including S. anginosus, S. intermedius, S. constellatus) No clinical data, but activity in vitro vs. Enterococcus faecalis (vancomycin-susceptible strains only), Enterococcus faecium (vancomycin-susceptible strains only), vancomycin-intermediate S. aureus (not vancomycin-resistant strains) Criteria for Use: Treatment of adult patients with acute bacterial skin and skin structure infections (ABSSSI) caused by susceptible gram-positive isolates Unable to use vancomycin (due to intolerance, MIC >2mg/L, or infection unresponsive to vancomycin despite therapeutic concentrations) Unable to use other agents (refer to empiric therapy for ABSSSI) Unacceptable Uses: Infections due to vancomycin-resistant enterococci Contraindicated in patients with known hypersensitivity to dalbavancin. Due to the possibility of cross-reactivity to glycopeptide, avoid in patients with previous glycopeptide hypersensitivity due to long half-life Dosing in Adults: Standard dose: Administration should be over 30 minutes 1 Dose Regimen: 1500mg IV once 2 Dose Regimen: 1000mg IV once, then 500mg IV on day 8 Renal dose adjustment: 1 Dose Regimen CrCl <30 mL/min 1125 mg IV 2 Dose Regimen CrCl <30 mL/min: 750mg IV once, then 325mg IV day 8 If receiving regularly scheduled hemodialysis: No dosage adjustment No hepatic dose adjustment anticipated Monitoring: Baseline BUN/Scr, AST/ALT/bili, CBC w/ diff, infusion-related reactions Considerations for Use: In clinical trials, 6 (0.9%) patients in the dalbavancin arm had ALT elevations greater than 5x ULN including 3 with ALT >10x ULN. -

CLSI Subcommittee on Antimicrobial Susceptibility Testing CLSI AST News Update Janet a Hindler, MCLS MT(ASCP) F(AAM), Editor Audrey Schuetz, MD, MPH, FCAP, Editor
Volume 3, Issue 1 Winter 2018 CLSI Subcommittee on Antimicrobial Susceptibility Testing CLSI AST News Update Janet A Hindler, MCLS MT(ASCP) F(AAM), Editor Audrey Schuetz, MD, MPH, FCAP, Editor The CLSI Outreach Working Group (ORWG) is providing this Newsletter to highlight some recent issues related to antimicrobial susceptibility Inside This Issue: testing (AST) and reporting. We are listing links to some new educational materials and reminding you where you can find information about the 21st Century Cures Act – Exciting News .......4 CLSI AST Subcommittee proceedings. Feature Article - Understanding Pharmacokinetics (PK) and Pharmacodynamics (PD) .................................5 CLSI 2018 AST Webinar: M100, M02, and M07 Updates Case Study - Direct Detection of MRSA/MSSA This hour and a half webinar will help you identify the latest changes in from Positive Blood Cultures .........................9 the updated editions of M100, M02, and M07. Don’t miss the opportunity to learn directly from leading AST experts. Burning Question - When Should Clinical Microbiology Laboratories Perform Date Options: Carbapenemase Detection Tests? ..............12 February 7, 2018 | 1:00-2:30 PM Eastern (US) Time Respiratory Illnesses and the Need for February 8, 2018 | 3:00-4:30 PM Eastern (US) Time Antibiotic Stewardship ..................................15 Moderator: Janet A. Hindler, MCLS MT(ASCP) F(AAM) Antimicrobial Susceptibility Testing of Speakers: Romney M. Humphries, PhD, D(ABMM) Bacteria Associated with Community- Audrey Schuetz, MD, MPH, FCAP Acquired Pneumonia .....................................18 Nonmember Price: $99.00. | Earn 1.5 PACE® CE credits. Hot Topic - Candida auris ..............................20 Member discounts apply. Register today. What does the CLSI AST Subcommittee do? The first edition of the CLSI AST News Update (Volume 1, Issue 1, Spring 2016) described details about the organization and operation of the CLSI AST Subcommittee. -

Antibacterial Drug Usage Analysis
Department of Health and Human Services Public Health Service Food and Drug Administration Center for Drug Evaluation and Research Office of Surveillance and Epidemiology Drug Use Review Date: April 5, 2012 To: Edward Cox, M.D. Director Office of Antimicrobial Products Through: Gerald Dal Pan, M.D., MHS Director Office of Surveillance and Epidemiology Laura Governale, Pharm.D., MBA Deputy Director for Drug Use Division of Epidemiology II Office of Surveillance and Epidemiology Hina Mehta, Pharm.D. Drug Use Data Analysis Team Leader Division of Epidemiology II Office of Surveillance and Epidemiology From: Tracy Pham, Pharm.D. Drug Use Data Analyst Division of Epidemiology II Office of Surveillance and Epidemiology Drug Name(s): Systemic Antibacterial Drug Products Application Type/Number: Multiple Applicant/sponsor: Multiple OSE RCM #: 2012-544 **This document contains proprietary drug use data obtained by FDA under contract. The drug use data/information in this document has been cleared for public release.** 1 EXECUTIVE SUMMARY The Division of Epidemiology II is providing an update of the drug utilization data in terms of number of kilograms or international units of selected systemic antibacterial drug products sold from manufacturers to various retail and non-retail channels of distribution for years 2010-2011 as a surrogate for nationwide antibacterial drug use in humans. Propriety drug use databases licensed by the FDA were used to conduct this analysis. Data findings are as follows: During years 2010 and 2011, the majority of kilograms of selected systemic antibacterial drug products sold were to outpatient retail pharmacy settings. Approximately 3.28 million kilograms of selected systemic antibacterial drug products were sold during year 2010, and around 3.29 million kilograms were sold during year 2011. -

Consideration of Antibacterial Medicines As Part Of
Consideration of antibacterial medicines as part of the revisions to 2019 WHO Model List of Essential Medicines for adults (EML) and Model List of Essential Medicines for children (EMLc) Section 6.2 Antibacterials including Access, Watch and Reserve Lists of antibiotics This summary has been prepared by the Health Technologies and Pharmaceuticals (HTP) programme at the WHO Regional Office for Europe. It is intended to communicate changes to the 2019 WHO Model List of Essential Medicines for adults (EML) and Model List of Essential Medicines for children (EMLc) to national counterparts involved in the evidence-based selection of medicines for inclusion in national essential medicines lists (NEMLs), lists of medicines for inclusion in reimbursement programs, and medicine formularies for use in primary, secondary and tertiary care. This document does not replace the full report of the WHO Expert Committee on Selection and Use of Essential Medicines (see The selection and use of essential medicines: report of the WHO Expert Committee on Selection and Use of Essential Medicines, 2019 (including the 21st WHO Model List of Essential Medicines and the 7th WHO Model List of Essential Medicines for Children). Geneva: World Health Organization; 2019 (WHO Technical Report Series, No. 1021). Licence: CC BY-NC-SA 3.0 IGO: https://apps.who.int/iris/bitstream/handle/10665/330668/9789241210300-eng.pdf?ua=1) and Corrigenda (March 2020) – TRS1021 (https://www.who.int/medicines/publications/essentialmedicines/TRS1021_corrigenda_March2020. pdf?ua=1). Executive summary of the report: https://apps.who.int/iris/bitstream/handle/10665/325773/WHO- MVP-EMP-IAU-2019.05-eng.pdf?ua=1. -

Conjugate and Prodrug Strategies As Targeted Delivery Vectors for Antibiotics † † ‡ Ana V
Review Cite This: ACS Infect. Dis. XXXX, XXX, XXX−XXX pubs.acs.org/journal/aidcbc Signed, Sealed, Delivered: Conjugate and Prodrug Strategies as Targeted Delivery Vectors for Antibiotics † † ‡ Ana V. Cheng and William M. Wuest*, , † Department of Chemistry, Emory University, 1515 Dickey Drive, Atlanta, Georgia 30322, United States ‡ Emory Antibiotic Resistance Center, Emory School of Medicine, 201 Dowman Drive, Atlanta, Georgia 30322, United States ABSTRACT: Innate and developed resistance mechanisms of bacteria to antibiotics are obstacles in the design of novel drugs. However, antibacterial prodrugs and conjugates have shown promise in circumventing resistance and tolerance mechanisms via directed delivery of antibiotics to the site of infection or to specific species or strains of bacteria. The selective targeting and increased permeability and accumu- lation of these prodrugs not only improves efficacy over unmodified drugs but also reduces off-target effects, toxicity, and development of resistance. Herein, we discuss some of these methods, including sideromycins, antibody-directed prodrugs, cell penetrating peptide conjugates, and codrugs. KEYWORDS: oligopeptide, sideromycin, antibody−antibiotic conjugate, cell penetrating peptide, dendrimer, transferrin inding new and innovative methods to treat bacterial F infections comes with many inherent challenges in addition to those presented by the evolution of resistance mechanisms. The ideal antibiotic is nontoxic to host cells, permeates bacterial cells easily, and accumulates at the site of infection at high concentrations. Narrow spectrum drugs are also advantageous, as they can limit resistance development and leave the host commensal microbiome undisturbed.1 However, various resistance mechanisms make pathogenic infections difficult to eradicate: Many bacteria respond to antibiotic pressure by decreasing expression of active transporters and porins2 and 3,4 Downloaded via EMORY UNIV on April 18, 2019 at 12:34:17 (UTC). -

Oritavancin - Rev.0 / 14.01.2016 Oritavancin Antibiotic Disc for Susceptibility Testing of Gram-Positive Bacteria
© Liofilchem® - Oritavancin - Rev.0 / 14.01.2016 Oritavancin Antibiotic disc for susceptibility testing of Gram-positive bacteria. DESCRIPTION Oritavancin, formerly LY333328, is a lipoglycopeptide with broad-spectrum activity against Gram-positive pathogens, such as staphylococci, including methicillin resistant Staphylococcus aureus (MRSA), streptococci and enterococci. This antimicrobial agent causes cell death by inhibiting cell wall synthesis as well as depolarizing and permeabilizing the cellular membrane of susceptible organisms. Oritavancin (ORBACTIV®), has been recently approved by the FDA and EMA for the treatment of adults with acute bacterial skin and skin structure infections (ABSSSI) caused by Staphylococcus aureus (including methicillin-susceptible and methicillin–resistant isolates), Streptococcus pyogenes, Streptococcus agalactiae, Streptococcus dysgalactiae, Streptococcus anginosus group (includes S. anginosus, S. intermedius, and S. constellatus), and Enterococcus faecalis (vancomycin- susceptible isolates only). Great benefits, compared to other drugs having similar therapeutic indications, derive from its single, once-only dosing regimen administered by intravenous infusion. As claimed by the drug’s Manufacturer as well, to reduce the development of drug-resistant bacteria and maintain the effectiveness of oritavancin and other antibacterial drugs, ORBACTIV® should be used only to treat infections that are proven or strongly suspected to be caused by susceptible bacteria. Therefore, the confirmation of susceptibility of a given isolate to oritavancin becomes of primary importance. CONTENTS OF THE PACKAGES The 50-test box contains 1 cartridge with 50 discs packed in a desiccant envelop. The 250-test box contains 5 desiccant envelops, each containing 1 cartridge with 50 discs. Each package also contains a transparent plastic resealable pouch. GATHERING AND KEEPING SAMPLES The colonies that are to be subjected to the susceptibility test are taken up by culture media that have been previously swabbed with the sample under examination. -

Swedres-Svarm 2019
2019 SWEDRES|SVARM Sales of antibiotics and occurrence of antibiotic resistance in Sweden 2 SWEDRES |SVARM 2019 A report on Swedish Antibiotic Sales and Resistance in Human Medicine (Swedres) and Swedish Veterinary Antibiotic Resistance Monitoring (Svarm) Published by: Public Health Agency of Sweden and National Veterinary Institute Editors: Olov Aspevall and Vendela Wiener, Public Health Agency of Sweden Oskar Nilsson and Märit Pringle, National Veterinary Institute Addresses: The Public Health Agency of Sweden Solna. SE-171 82 Solna, Sweden Östersund. Box 505, SE-831 26 Östersund, Sweden Phone: +46 (0) 10 205 20 00 Fax: +46 (0) 8 32 83 30 E-mail: [email protected] www.folkhalsomyndigheten.se National Veterinary Institute SE-751 89 Uppsala, Sweden Phone: +46 (0) 18 67 40 00 Fax: +46 (0) 18 30 91 62 E-mail: [email protected] www.sva.se Text, tables and figures may be cited and reprinted only with reference to this report. Images, photographs and illustrations are protected by copyright. Suggested citation: Swedres-Svarm 2019. Sales of antibiotics and occurrence of resistance in Sweden. Solna/Uppsala ISSN1650-6332 ISSN 1650-6332 Article no. 19088 This title and previous Swedres and Svarm reports are available for downloading at www.folkhalsomyndigheten.se/ Scan the QR code to open Swedres-Svarm 2019 as a pdf in publicerat-material/ or at www.sva.se/swedres-svarm/ your mobile device, for reading and sharing. Use the camera in you’re mobile device or download a free Layout: Dsign Grafisk Form, Helen Eriksson AB QR code reader such as i-nigma in the App Store for Apple Print: Taberg Media Group, Taberg 2020 devices or in Google Play. -

APPLICATION for AVYCAZ® (Avibactam and Ceftazidime) for Injection, DALVANCE® (Dalbavancin) for Injection, and TEFLARO® (Ceftaroline Fosamil) Injection
APPLICATION FOR AVYCAZ® (avibactam and ceftazidime) for injection, DALVANCE® (dalbavancin) for injection, and TEFLARO® (ceftaroline fosamil) for injection myAbbVie Assist provides free medicine to qualifying patients. We review all applications on a case-by-case basis. Participation in our program is free; we do not collect any fees from people seeking our assistance. CHECKLIST FOR SUBMITTING AN APPLICATION IF YOU ARE THE PRESCRIBER, COMPLETE PAGE 2 o SECTION 1: Prescriber Information o SECTION 2: Patient Information . If this a request for replacement product, please submit a claim denial dated within 60 days. o SECTION 3: Product information o SECTION 4: Prescriber Certification and Signature IF YOU ARE A PATIENT, COMPLETE PAGE 3. PLEASE READ PAGE 4 o SECTION 5: Patient Information o SECTION 6: Financial Information . Also include proof of income for all in household. A copy of your current federal tax return is preferred. o SECTION 7: Insurance Information . If you have Insurance, include front and back copies of all insurance cards. If you have insurance coverage, please attach list of your medical or prescription drug out of pocket costs. If you are taking multiple prescriptions, a printout from your pharmacy will be helpful. This information will help us review your eligibility for our program. o SECTION 8: Patient Consent and Signature . Carefully read the HIPAA authorization, patient terms of participation and privacy notice in Section 10 on Page 4. Provide your consent for eligibility determination by checking the box in Section 8. Confirm your understanding of our privacy policy by providing your signature and date in Section 8.