Thiopental Sodium
Total Page:16
File Type:pdf, Size:1020Kb
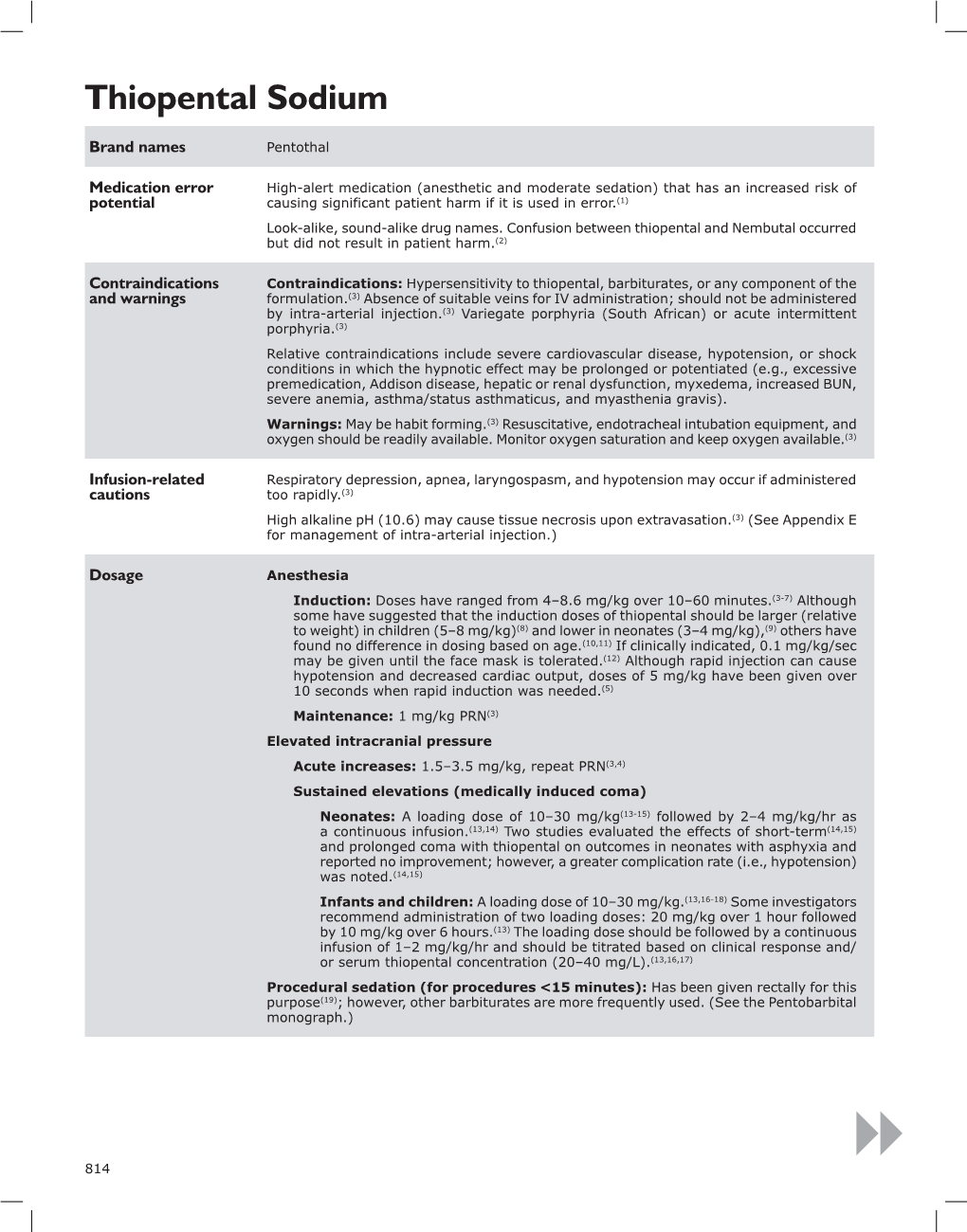
Load more
Recommended publications
-

Components of Respiratory Depression After Narcotic Premedication in Adolescents
COMPONENTS OF RESPIRATORY DEPRESSION AFTER NARCOTIC PREMEDICATION IN ADOLESCENTS R. KNILL*, J.F. Coscnowr P. M. OLLEY,AND H. LEVISON N~d~COTIC ACENTS are potent depressants of ventilation. 1-5 Although this effect is generally assumed to result from decreased output of the central respiratory "'centres," some of the effect could be due to direct action on the ventilatory apparatus itself, by increasing respiratory impendance. For example, both morphine and meperidine can cause bronchoconstriction;" furthermore they can increase the tonic activity of abdominal and intercostal muscles, r-l~ The mechanical effects of this increase in abdominal wall tone have not been assessed after thera- peutic doses of these agents, but large doses of narcotics administered intravenously produce board-like rigidity of the abdominal wall r-lo and markedly decrease total respiratory compliance? As the magnitude of this effect appears to be dose related 1~ it may well be present to a lesser extent after therapeutic doses of these agents. The purpose of this work was to determine whether the ventilatory depression associated with morphine and a meperidine-phenothiazine mixture is solely the result of impairment of the neuromuscular or force-generating mechanisms, or is in part due to increased impedance of the ventilatory pump. Even small increases in ventilatory load with narcotics probably contribute to ventilatory depression, as load compensation is poor when central neural mechanisms are pharmacologi- cally imp aired. 11,1a The conventional technique for examining the effect of narcotics on ventilation is to apply rebreathing and steady-state.methods before and after medication, to measure changes in minute ventilation (V~) and tidal volume (VT).13,~4 However, these measurements depend on both central output and the properties of the ventilatory apparatus, ~,16 without distinction between them. -

Phenobarbital Brand Name: Phenobarb
Generic Name: Phenobarbital Brand Name: Phenobarb What Is It Used For? Decreasing seizure activity in various types of seizures. Especially useful for controlling seizures in neonates and infants Given intravenously in the emergency department for status epilepticus. How Long Does The Oral Medicine Take to Work? 10-30 days What Are The Important Safety Concerns? When first starting the medicine, your child may be slightly drowsy and/or dizzy. Only adjust the dosage as recommended by your health care provider. They will usually increase this medication slowly to avoid side effects. Never increase the dosage more than once per week unless directed otherwise. Once you have started with one brand of the medication stay with it. Avoid switching between different brands. Check with your pharmacist before taking herbal medications and/or over-the- counter medications. They may have adverse effects if taken with anti-seizure medications. Do not stop taking this medication suddenly because this could result in seizures. It is important to keep a record of your child’s seizures and side effects to determine how well they are responding to the medication. Does My Child Need Bloodwork With This Medication? Routine blood work may be done to help determine the best dosage for your child, and also if they have side effects to the medication. If your child is required to have blood work it must be done BEFORE they get the medication. This is called a trough level. This level usually falls between 65 and 170. A blood test may be done before starting this medication to check your child’s liver function and blood counts. -
Journal Watch 1805 TCCC.Pdf
TCCC Journal Watch May 2018 Abou El Fadl M, O’Phelan K: Management of traumatic brain injury: an update. Neurosurg Clin N Am 2018;29:213-221 Abraham P,Russell D, Huffman S, et al: Army combat medic resilience: the process of forging loyalty. Mil Med 2018;183:364-370 Adravanti P, Di Salvo E, Calafiore G, et al: A prospective, randomized, comparative study of intravenous alone and combine intravenous and intraarticular administration of tranexamic acid in primary total knee replacement. Arthoplast Today 2017;4:85-88 Aggarwal N, Brower R, Hager D, et al: Oxygen exposure resulting in arterial oxygen tensions above the protocol goal was associated with worse clinical outcomes in acute respiratory distress syndrome. Crit Care Med 2018;46:517-524 Agimi Y, Regasa L, Ivins B, et al: Role of Department of Defense policies in identifying traumatic brain injuries among deployed US Service members 2001- 2016. Aiolfi A, Benjamin E, Recinos G, et al: Air versus ground transportation in isolated severe head trauma: a national trauma bank study. J Emerg Med 2018;54:328- 334 Aji Y, Apriawan T, Bajamal A: Traumatic supra- and infra-tentorial extradural hematoma: case series and literature review. Asian J Neurosurg 2018;13:453- 457 Akbari E, Safari S, Hatamabadi H: The effect of fibrinogen concentrate and fresh frozen plasma on the outcome of patients with acute traumatic coagulopathy: a quasi-experimental study. Am J Emerg Med 2018;Epub ahead of print. Aries M, Donnelly J: Brain oxygenation optimization after severe traumatic brain injury: an ode to preventing brain hypoxia. Crit Care Med 2018;46:e350 Armstrong R: Visual problems associated with traumatic brain injury. -
CDHO Factsheet Epilepsy
Disease/Medical Condition EPILEPSY Date of Publication: August 7, 2014 (also known as “seizure disorder”) Is the initiation of non-invasive dental hygiene procedures* contra-indicated? No Is medical consult advised? ...................................... No (assuming patient/client is already under medical care for epilepsy, which is well controlled) Is the initiation of invasive dental hygiene procedures contra-indicated?** No Is medical consult advised? ....................................... Possibly (e.g., if there is medication non-compliance) Is medical clearance required? .................................. Possibly (e.g., if there is significant risk of seizure; patient/ client should be seizure-free for several months to be considered controlled) Is antibiotic prophylaxis required? .............................. No Is postponing treatment advised? ............................... No (assuming patient/client is already under medical care for epilepsy, which is well controlled and for which there are no anticipated exacerbating factors in the office setting) Oral management implications Important considerations in the management of epileptic patients/clients are prevention of seizures in the dental chair and preparation for managing seizures if they occur. When a patient/client responds positively to questions about seizures/ epilepsy during health history taking, further information should be obtained. Based on the patient/client’s responses, the dental hygienist may choose to postpone treatment to avoid triggering a seizure in the dental chair. It is valuable for the dental hygienist to know what factors have the potential to exacerbate epileptic seizures in a particular patient/client in order that trigger stimuli can be avoided. The dental hygienist can reduce stress and anxiety by explaining procedures before starting. Bright light should be kept out of the patient/client’s eyes, and dark glasses may assist with this. -

An Evidence-Based Guideline for the Pre-Operative Sedation of Children
Journal of Pediatrics and Neonatal Care An Evidence-Based Guideline for the Pre-Operative Sedation of Children Abstract Review Article There are numerous sedative pharmacological agents currently administered to Volume 2 Issue 6 - 2015 children as premedicants to facilitate the induction of anaesthesia. When pre- operative sedation is required, selection of the appropriate drug is imperative to Deborah M Fradkin*, Victoria L Scott- provide adequate anxiolysis whilst minimising unwanted side effects. We review Warren, Rita Vashisht and Sian E Rolfe the literature regarding the merits and limitations of the commonly used agents and suggest evidence based practical guidance. For the anxious but cooperative Department of Paediatric Anaesthesia, Royal Manchester Children’s Hospital, England child, oral midazolam is often adequate; however with more anxious younger and uncooperative children, combined oral midazolam and ketamine is more *Corresponding author: DM. Fradkin, Department of effective. Other oral benzodiazepines and oral clonidine all have their role when Paediatric Anaesthesia, Royal Manchester Children’s used in the appropriate circumstances. Intranasal clonidine is useful in the child Hospital, Oxford Road, Manchester, M13 9WL, England, Tel: refusing oral medication. Intramuscular ketamine should be reserved for extreme 0161 701 1264; Email: circumstances, administered only by anaesthetists experienced in its use, with full monitoring and resuscitative equipment immediately available. Received: August 15, 2015 | Published: September -

Pentobarbital Sodium
PENTobarbital Sodium Brand names Nembutal Sodium Medication error Look-alike, sound-alike drug names. Tall man letters (not FDA approved) are recommended potential to decrease confusion between PENTobarbital and PHENobarbital.(1,2) ISMP recommends the following tall man letters (not FDA approved): PENTobarbital.(30) Contraindications Contraindications: In patients with known hypersensitivity to barbiturates or any com- and warnings ponent of the formulation.(2) If an allergic or hypersensitivity reaction or a life-threatening adverse event occurs, rapid substitution of an alternative agent may be necessary. If pentobarbital is discontinued due to development of a rash, an anticonvulsant that is structurally dissimilar should be used (i.e., nonaromatic). (See Rare Adverse Effects in the Comments section.) Also contraindicated in patients with a history of manifest or latent porphyria.(2) Warnings: Rapid administration may cause respiratory depression, apnea, laryngospasm, or vasodilation with hypotension.(2) Should be withdrawn gradually if large doses have been used for prolonged periods.(2) Paradoxical excitement may occur or important symptoms could be masked when given to patients with acute or chronic pain.(2) May be habit forming. Infusion-related Respiratory depression and arrest requiring mechanical ventilation may occur. Monitor cautions oxygen saturation. If hypotension occurs, the infusion rate should be decreased and/or the patient should be treated with IV fluids and/or vasopressors. Pentobarbital is an alkaline solution (pH = 9–10.5); therefore, extravasation may cause tissue necrosis.(2) (See Appendix E for management.) Gangrene may occur following inadvertent intra-arterial injection.(2) Dosage Medically induced coma (for persistently elevated intracranial pressure (ICP) or refractory status epilepticus): Patient should be intubated and mechanically ventilated. -

Premedication in Pedodontics Attitudes and Agents
PEDIATRICDENTISTRY/Copyright ~) 1979 by The American Academyof Pedodontics/ Vol. 1, No. 4 / Printed in U.S.A. Premedication in Pedodontics Attitudes and Agents David L. King, D.D.S., Ph.D. William C. Berlocher, D.D.S. Abstract a dentist should find it necessary to resort to premed- icating children to obtain their cooperation. Garfin The goals of premedicationin children’s dentistry are to feels that the routine use of sedatives and tranquiliz- allay excessive apprehensionand to prevent resistance to treatment efforts. With judicious use, premedicatingagents ers may rbflect a "decreased interest in the care and are a valuable and necessary adjunct for the pedodontis~. treatment of the complete child," and Olsen proposes Whenintegrated with proper psychological approaches, that dentists examine their motives to see if they em- premedicationmay enable the anxious child to accept his ploy premedication as a "crutch." Both of these au- first dental experiences without undueemotional turmoil thors emphasize that when faced with a potential or it mayoften allow outpatient treatment of very young management problem, proper psychological ap- "precooperative" children wherethe only alternative might proaches by the dentist will obviate the need for drugs be hospitalization and general anesthesia. Prudent employ- in most instances. MacGregorbelieves the dentist who ment of drugs [or behavior managementis dependent on resorts to premedication or general anesthesia may the training, experience, and iudgementof the operator. actually be treating his own fears and admitting his A regimen of premedicant drugs and dosages is presented inability to manage children. which may serve as base line guidance [or more successful 7 managementof the difficult child patient. -

1,1,1-Trichloroethane (CASRN 71-55-6) | IRIS
Integrated Risk Information System (IRIS) U.S. Environmental Protection Agency Chemical Assessment Summary National Center for Environmental Assessment 1,1,1-Trichloroethane; CASRN 71-55-6 Human health assessment information on a chemical substance is included in the IRIS database only after a comprehensive review of toxicity data, as outlined in the IRIS assessment development process. Sections I (Health Hazard Assessments for Noncarcinogenic Effects) and II (Carcinogenicity Assessment for Lifetime Exposure) present the conclusions that were reached during the assessment development process. Supporting information and explanations of the methods used to derive the values given in IRIS are provided in the guidance documents located on the IRIS website. STATUS OF DATA FOR 1,1,1-Trichloroethane File First On-Line 03/31/1987 Category (section) Assessment Available? Last Revised Oral RfD (I.A.) Acute Oral RfD (I.A.1.) qualitative discussion 09/28/2007 Short-term Oral RfD (I.A.2.) qualitative discussion 09/28/2007 Subchronic Oral RfD (I.A.3.) yes 09/28/2007 Chronic Oral RfD (I.A.4.) yes 09/28/2007 Inhalation RfC (I.B.) Acute Inhalation RfC (I.B.1.) yes 09/28/2007 Short-term Inhalation RfC (I.B.2.) yes 09/28/2007 Subchronic Inhalation RfC (I.B.3.) yes 09/28/2007 1 Integrated Risk Information System (IRIS) U.S. Environmental Protection Agency Chemical Assessment Summary National Center for Environmental Assessment Category (section) Assessment Available? Last Revised Chronic Inhalation RfC (I.B.4.) yes 09/28/2007 Carcinogenicity Assessment (II.) yes 09/28/2007 I. Health Hazard Assessments for Noncarcinogenic Effects I.A. -

Comparison Between Alprazolam and Hydroxyzine for Oral Premedication
13 Comparison between alprazolam and hydroxyzine for oral C. Franssen Mo, R Hans MO, J.E Brichant Mo, D. Noirot Mr), M. Lamy Mo premedication The safety and efficacy of alprazolam and hydroxyzine ad- viduellement le degrd d'anxi~t~: le patient utilise une ~chelle ministered orally as surgical premedicants were compared in visuelle analogique alors que l'anesth~siste utilise une classi- a double-blind controlled study. Sixty-five patients were given fication ordinale en plus de l~chelle analogique. Grace ~ ces either alprazolam 1 mg or hydroxyzine 75 mg, one to two deux m~thodes, le sddation fait l'objet d'un ~valuation par hours before surgery. Anxiety was assessed by both the patient l'anesth~siste seul. L'amndsie est estim~e par une test de and the anaesthetist, the patient using a visual analogue scale, m~moire simple. On ~value la s~curit~ des m~dicaments par the anaesthetist employing both analogue and ordinal ratings. l'enregistrement des effets d~favorables et la mesure des variables Sedation was assessed by the anaesthetist only, using the same h~modynamiquea. La pr~mddication gt l'alprazolam produit two methods. Amnesia was appraised with a simple memory une baisse modeste de l'anxi~t~ (28%) (P < 0,01) alors que test. Safety was assessed by recording adverse effects and meas- lT~ydroxyzine ne produit pas d'effets d~celables. La comparaison uring haemodynamic variables. Premedication with alprazolam entre les deux pr~m~dications pour le degr~ de s~dation et le produced a modest reduction in anxiety (28%) (P < 0.01) while test de mdmoire ne rdvble pas de difference. -

Therapeutic Drug Monitoring of Antiepileptic Drugs by Use of Saliva
REVIEW ARTICLE Therapeutic Drug Monitoring of Antiepileptic Drugs by Use of Saliva Philip N. Patsalos, FRCPath, PhD*† and Dave J. Berry, FRCPath, PhD† INTRODUCTION Abstract: Blood (serum/plasma) antiepileptic drug (AED) therapeu- Measuring antiepileptic drugs (AEDs) in serum or tic drug monitoring (TDM) has proven to be an invaluable surrogate plasma as an aid to personalizing drug therapy is now a well- marker for individualizing and optimizing the drug management of established practice in the treatment of epilepsy, and guidelines patients with epilepsy. Since 1989, there has been an exponential are published that indicate the particular features of epilepsy and increase in AEDs with 23 currently licensed for clinical use, and the properties of AEDs that make the practice so beneficial.1 recently, there has been renewed and extensive interest in the use of The goal of AED therapeutic drug monitoring (TDM) is to saliva as an alternative matrix for AED TDM. The advantages of saliva ’ fl optimize a patient s clinical outcome by supporting the man- include the fact that for many AEDs it re ects the free (pharmacolog- agement of their medication regimen with the assistance of ically active) concentration in serum; it is readily sampled, can be measured drug concentrations/levels. The reason why TDM sampled repetitively, and sampling is noninvasive; does not require the has emerged as an important adjunct to treatment with the expertise of a phlebotomist; and is preferred by many patients, AEDs arises from the fact that for an individual patient -

Calcium Current Block by (-)-Pentobarbital, Phenobarbital
The Journal of Neuroscience, August 1993, 13(E): 321 l-3221 Calcium Current Block by (-)-Pentobarbital, Phenobarbital, and CHEB but not (+)-Pentobarbital in Acutely Isolated Hippocampal CA1 Neurons: Comparison with Effects on GABA-activated Cl- Current Jarlath M. H. ffrench-Mullen,’ Jeffery L. Barker,* and Michael A. Rogawski3 ‘Department of Pharmacology, Zeneca Pharmaceuticals Group, Zeneca Inc., Wilmington, Delaware 19897 and *Laboratory of Neurophysiology, and 3Neuronal Excitability Section, Epilepsy Research Branch, National Institute of Neurological Disorders and Stroke, National Institutes of Health, Bethesda, Maryland 20892 Block of a voltage-activated Ca*+ channel current by pheno- Ca*+ current, whereas the sedative effects that occur at high- barbital (PHB), 5-(2-cyclohexylideneethyl)-5-ethyl barbituric er concentrations could reflect stronger Ca2+ current block- acid (CHEB), and the optical R(-)- and S(+)-enantiomers of ade. The powerful sedative-hypnotic action of (-)-PB may pentobarbital (PB) was examined in freshly dissociated adult reflect greater maximal enhancement of GABA responses guinea pig hippocampal CA1 neurons; the effects of the in conjunction with strong inhibition of Ca2+ current. The barbiturates on GABA-activated Cl- current were also char- convulsant action of CHEB is unlikely to be related to its acterized in the same preparation. (-)-PB, PHB, and CHEB effects on the Ca*+ current. produced a reversible, concentration-dependent block of the [Key words: calcium channel, GABA receptor, (-)-pen- peak Ca*+ channel current (3 mM Ba2+ as the charge carrier) tobarbital, (+)-pentobarbital, phenobarbital, CHEB [S-(2-cy- evoked by depolarization from -80 to - 10 mV (I&,, values, clohexylideneethyl)-S-ethyl barbituric acid], CA 1 hippocam- 3.5, 72, and 118 PM, respectively). -

ACR Manual on Contrast Media
ACR Manual On Contrast Media 2021 ACR Committee on Drugs and Contrast Media Preface 2 ACR Manual on Contrast Media 2021 ACR Committee on Drugs and Contrast Media © Copyright 2021 American College of Radiology ISBN: 978-1-55903-012-0 TABLE OF CONTENTS Topic Page 1. Preface 1 2. Version History 2 3. Introduction 4 4. Patient Selection and Preparation Strategies Before Contrast 5 Medium Administration 5. Fasting Prior to Intravascular Contrast Media Administration 14 6. Safe Injection of Contrast Media 15 7. Extravasation of Contrast Media 18 8. Allergic-Like And Physiologic Reactions to Intravascular 22 Iodinated Contrast Media 9. Contrast Media Warming 29 10. Contrast-Associated Acute Kidney Injury and Contrast 33 Induced Acute Kidney Injury in Adults 11. Metformin 45 12. Contrast Media in Children 48 13. Gastrointestinal (GI) Contrast Media in Adults: Indications and 57 Guidelines 14. ACR–ASNR Position Statement On the Use of Gadolinium 78 Contrast Agents 15. Adverse Reactions To Gadolinium-Based Contrast Media 79 16. Nephrogenic Systemic Fibrosis (NSF) 83 17. Ultrasound Contrast Media 92 18. Treatment of Contrast Reactions 95 19. Administration of Contrast Media to Pregnant or Potentially 97 Pregnant Patients 20. Administration of Contrast Media to Women Who are Breast- 101 Feeding Table 1 – Categories Of Acute Reactions 103 Table 2 – Treatment Of Acute Reactions To Contrast Media In 105 Children Table 3 – Management Of Acute Reactions To Contrast Media In 114 Adults Table 4 – Equipment For Contrast Reaction Kits In Radiology 122 Appendix A – Contrast Media Specifications 124 PREFACE This edition of the ACR Manual on Contrast Media replaces all earlier editions.