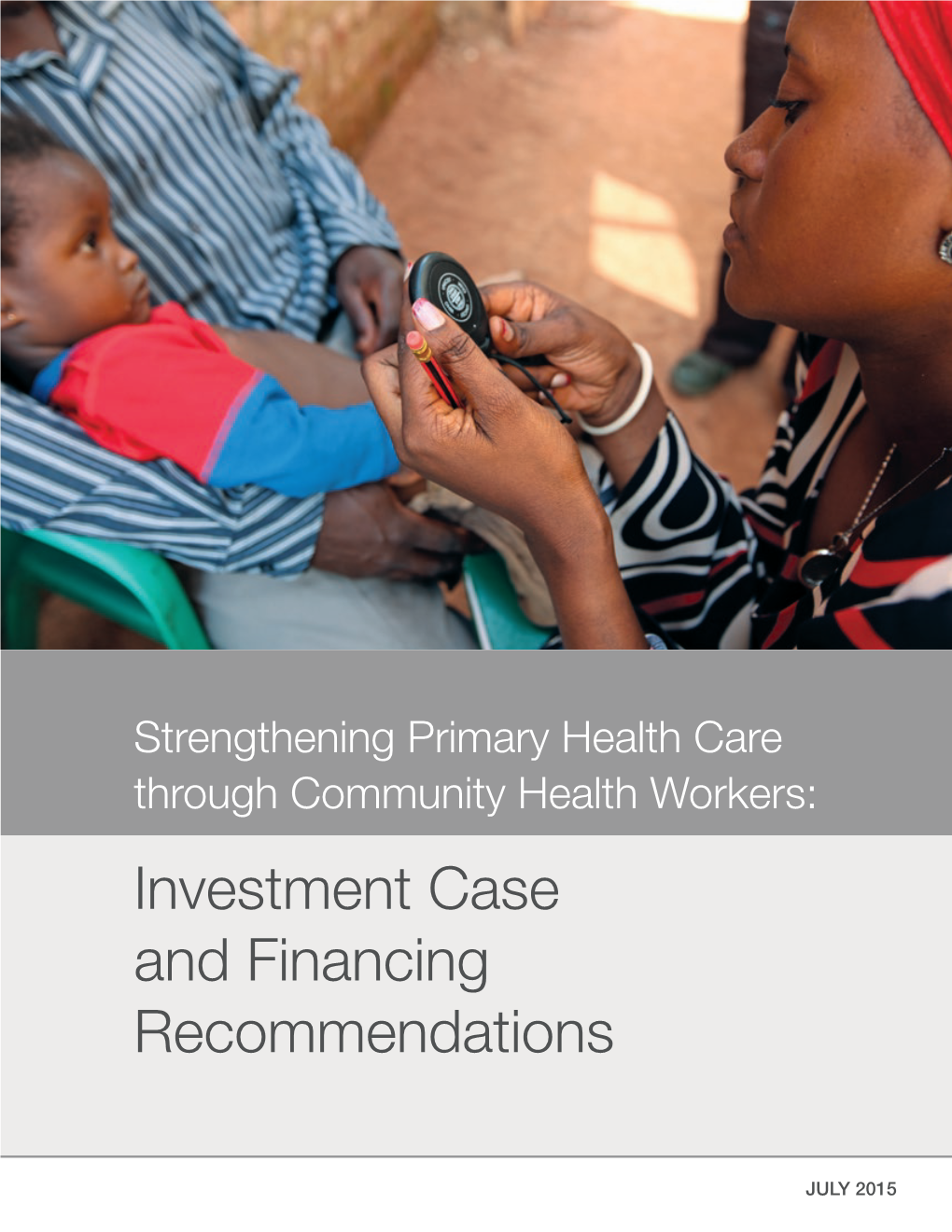
Investment Case and Financing Recommendations
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Role of the Community Health Worker to Strengthen Popular Education in Health Revista De Pesquisa Cuidado É Fundamental Online, Vol
Revista de Pesquisa Cuidado é Fundamental Online E-ISSN: 2175-5361 [email protected] Universidade Federal do Estado do Rio de Janeiro Brasil Scherlowski Leal David, Helena Maria The role of the community health worker to strengthen popular education in health Revista de Pesquisa Cuidado é Fundamental Online, vol. 9, núm. 2, abril-junio, 2017, pp. 371-378 Universidade Federal do Estado do Rio de Janeiro Rio de Janeiro, Brasil Available in: http://www.redalyc.org/articulo.oa?id=505754109011 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative REVISTA ONLINE DE PESQUISA CUIDADO É FUNDAMENTALREVISTA ONLINE DE PESQUISA UNIVERSIDADE FEDERAL DO ESTADO DO RIO DE JANEIRO . ESCOLA DE ENFERMAGEM ALFREDO PINTO RESEARCH CUIDADO É FUNDAMENTALDOI: 10.9789/2175-5361.2017.v9i2.371-378 UNIVERSIDADE FEDERAL DO ESTADO DO RIO DE JANEIRO . ESCOLA DE ENFERMAGEM ALFREDO PINTO O papel do agente comunitário de saúde no fortalecimento da educação popular em saúde The role of the community health worker to strengthen popular education in health El rol del agente comunitario de salud en el fortalecimiento de la educación popular en salud Helena Maria Scherlowski Leal David1 FAPERJ Financial Aid Priority Announcement Rio 200. How to quote this article: David HMSL. The role of the community health worker to strengthen popular education in health. Rev Fund Care Online. 2017 abr/jun; 9(2):371-378. DOI: http://dx.doi.org/10.9789/2175-5361.2017.v9i2.371-378 ABSTRACT Objective: To discuss the Community Health Agent (CHA)’s role as a popular educator. -

The Newark Public Schools Historical Preservation Committee MISSION
The Newark Public Schools Historical Preservation Committee MISSION The Newark Public Schools Historical Preservation Committee is a 501 (c)(3) organization formed in 2009 to chronicle the district’s rich heritage by preserving its documents, artifacts and school buildings. It is our intention to share the history of the Newark Public Schools with students and the greater com- munity at a permanent historic site. This Distinguished Alumni Directory is the first in a series of publications that we hope will help to inform and instill a sense of pride in our Newark history. 1 NEWARK PUBLIC SCHOOLS DISTINGUISHED ALUMNI The Newark Public School District Historical Preservation Committee GOALS ≈ To establish a policy and guidelines for the preservation and archiving of historically valuable artifacts of the Newark Public Schools. ≈ To establish repositories within the schools for the col- lection and preservation of valuable documents and materials relating to the history of the school district which otherwise would be lost. ≈ To develop and keep current a chronology of significant events in the Newark Public Schools. ≈ To identify and nominate public schools for listing on the National Register of Historic Places. ≈ To establish a permanent Newark Public Schools museum. ≈ To have students become involved with the archiving and chronicling process. To develop collaborative work- ing relationships with alumni associations and other preservation organizations. 2 NEWARK PUBLIC SCHOOLS DISTINGUISHED ALUMNI JANET LIPPMAN ABU-LUGHOD (Weequahic/1945) (1928–2013) Urban sociologist; expert on the history and dynamics of the World System and Middle Eastern cities; taught for twenty years at Northeastern; retired in 1988 as professor of sociology and historical research on the Gradu- ate Faculty of the New School for Social Research; her thirteen books include the classic work: Cairo: 100 Years of the City Victorious. -

Factors Impacting the Effectiveness of Community Health Worker Behavior Change
FACTORS IMPACTING THE EFFECTIVENESS OF COMMUNITY HEALTH WORKER BEHAVIOR CHANGE A LITERATURE REVIEW February 16, 2015 TABLE OF CONTENTS ACRONYMS ............................................................................................................................................................................................2 EXECUTIVE SUMMARY ......................................................................................................................................................................3 INTRODUCTION ...................................................................................................................................................................................4 METHODOLOGY ..................................................................................................................................................................................6 KEY FINDINGS .......................................................................................................................................................................................7 Knowledge and Competency Barriers ..................................................................................................................................7 Structural and Contextual Barriers .........................................................................................................................................10 Attitudinal Barriers .......................................................................................................................................................................15 -

Finding Aid to the Historymakers ® Video Oral History with Tai Beauchamp
Finding Aid to The HistoryMakers ® Video Oral History with Tai Beauchamp Overview of the Collection Repository: The HistoryMakers®1900 S. Michigan Avenue Chicago, Illinois 60616 [email protected] www.thehistorymakers.com Creator: Beauchamp, Tai, 1978- Title: The HistoryMakers® Video Oral History Interview with Tai Beauchamp, Dates: October 7, 2014 Bulk Dates: 2014 Physical 6 uncompressed MOV digital video files (2:42:13). Description: Abstract: Journalist and entrepreneur Tai Beauchamp (1978 - ) was the style ambassador of InStyle magazine and the CEO of Tai Life Media, LLC. She became the youngest and first African American beauty and fitness director at Seventeen magazine in 2004. Beauchamp was interviewed by The HistoryMakers® on October 7, 2014, in New York, New York. This collection is comprised of the original video footage of the interview. Identification: A2014_228 Language: The interview and records are in English. Biographical Note by The HistoryMakers® Journalist and entrepreneur Tai Beauchamp was born on January 7, 1978 in Newark, New Jersey. She graduated from Spelman College in 2000 with her B.A. degree in English Literature and received a certificate in television production from New York University in 2003. Beauchamp began her career as an intern for Good Housekeeping and Harper’s Bazaar magazines in 1998. In 2000, she was hired at O, The Oprah Magazine as a fashion and beauty assistant, but was soon named associate beauty editor. In 2003, Essence magazine/Time Inc. hired her to serve as the beauty editor of several prototypes that later became Suede magazine. In 2004, Beauchamp became the youngest and first African American appointed to the role of beauty and fitness director at Seventeen magazine. -
Franklin Project's Plan of Action
Generi Corp Inc Management Report Table of Contents A Declaration of Service 1 Executive Summary 5 A Plan of Action: A 21st Century National Service System 12 Core Elements of a 21st Century National Service System 12 Pathways to Engage More Americans in National Service 22 A Talent Pipeline through National Service 25 The Case for National Service 28 National Service to Address National Challenges 33 Conclusion 38 Acknowledgments 38 Endnotes 39 A Declaration of Service We, the undersigned, endorse the Franklin Project's Plan of Action to establish a 21st Century National Service System in America that inspires and engages at least one million young adults annually from all socio- economic backgrounds in a demanding year of full-time national service as a civic rite of passage to unleash the energy and idealism of each generation to address our nation’s challenges. General Stanley McChrystal Michael Brown Leadership Council Chair, The Franklin Project; U.S. Co-Founder and CEO, City Year Army General (Retired); Former Commander, International Security Assistance Force & U.S. Forces Afghanistan Anna Burger Former Secretary-Treasurer, SEIU; Former Chair, Change to Win Madeleine Albright Chair, Albright Stonebridge Group; Former U.S. Secretary of State & U.S. Ambassador to the United Nations Barbara Bush Co-Founder and CEO, Global Health Corps Don Baer Worldwide Chair and CEO, Burson-Marsteller; Former Jean Case White House Director of Strategic Planning and CEO, The Case Foundation; Former Chair, President's Communications Council on Service and Civic Participation Melody Barnes Ray Chambers Chair, Aspen Forum for Community Solutions and UN Secretary General's Special Envoy for Financing of Opportunity Youth Incentive Fund; Vice Provost for the Health Related Millennium Development Goals & for Global Student Leadership Initiatives, New York Malaria; Co-Founder, America's Promise Alliance; Chair, University; Former Director, White House Domestic The MCJ Amelior Foundation Policy Council AnnMaura Connolly Samuel R. -

Case Studies of Large-Scale Community Health Worker Programs
Case Studies of Large-Scale Community Health Worker Programs: Examples from Afghanistan, Bangladesh, Brazil, Ethiopia, India, Indonesia, Iran, Nepal, Niger, Pakistan, Rwanda, Zambia, and Zimbabwe January 2017 Prepared by: Henry Perry Rose Zulliger Kerry Scott Dena Javadi Jessica Gergen Katharine Shelley Lauren Crigler Iain Aitken Said Habib Arwal Novia Afdhila Yekoyesew Worku Jon Rohde Zayna Chowdhury Rachel Strodel Table of Contents Introduction ............................................................................................................................... 1 The Community-Based Health Care System of Afghanistan ...................................................................... 2 Summary ...................................................................................................................................................... 2 What is the historical context of Afghanistan’s Community Health Worker Program? ............................ 3 Key health needs ......................................................................................................................................... 3 Health system structure .............................................................................................................................. 4 Scope of work of the CHWs ......................................................................................................................... 4 Community roles ......................................................................................................................................... -

Mhealth Tool to Improve Community Health Agent Performance for Child Development: Study Protocol for a Cluster-Randomised Controlled Trial in Peru
Open access Protocol BMJ Open: first published as 10.1136/bmjopen-2018-028361 on 6 November 2019. Downloaded from mHealth tool to improve community health agent performance for child development: study protocol for a cluster- randomised controlled trial in Peru Christopher Michael Westgard ,1,2 Natalia Rivadeneyra,2 Patricia Mechael3 To cite: Westgard CM, ABSTRACT Strengths and limitations of this study Rivadeneyra N, Mechael P. Introduction Cultivating child health and development mHealth tool to improve creates long- term impact on the well- being of the ► The intermediate variables will be assessed to mea- community health agent individual and society. The Amazon of Peru has high levels performance for child sure the behaviour changes that occurs along the of many risk factors that are associated with poor child development: study protocol for theory of change. The study will be able to evaluate development. The use of ‘community health agents’ (CHAs) a cluster- randomised controlled the various mediator variables that are expected to has been shown to be a potential solution to improve child trial in Peru. BMJ Open contribute to the final objective. 2019;9:e028361. doi:10.1136/ development outcomes. Additionally, mobile information and ► A process evaluation with qualitative assessments communication technology (ICT) can potentially increase bmjopen-2018-028361 will be used to identify issues of implementation and the performance and impact of CHAs. However, there is Prepublication history for inform the implementation plan for scalability. ► a knowledge gap in how mobile ICT can be deployed to this paper is available online. ► The mHealth tool and the monitoring and evaluation improve child development in low resource settings. -

How Effective Are Community Health Workers?
HOW EFFECTIVE ARE COMMUNITY HEALTH WORKERS? An Overview of Current Evidence with Recommendations for Strengthening Community Health Worker Programs to Accelerate Progress in Achieving the Health-related Millennium Development Goals September 2012 Henry Perry, Senior Associate Department of International Health Johns Hopkins Bloomberg School of Public Health and Rose Zulliger, PhD Doctoral Candidate Department of Health Behavior and Society Johns Hopkins Bloomberg School of Public Health Acknowledgements This report was prepared for the MDG Health Alliance. Funding was provided by the Alliance and the Rockefeller Philanthropy Advisors, Inc. We are grateful for the assistance of Sara Ju, master’s student in the Department of International Health at the Johns Hopkins Bloomberg School of Public Health, for her assistance in collecting information used in this review and in editing this document. We are also grateful for the assistance of Ingrid Friberg, Assistant Scientist in the Department of International Health, with the LiST calculations. How Effective Are Community Health Workers? | i Table of Contents Acknowledgements .......................................................................................................................... i Glossary ........................................................................................................................................... iv I. Introduction ............................................................................................................................. 1 II. -

COMMUNITY HEALTH POLICIES and PROGRAMMES Publication: October 2019 © Cover Photo: Tremeau/Fonds Français Muskoka ANALYSIS REPORT
ANALYSIS REPORT COMMUNITY HEALTH POLICIES AND PROGRAMMES Publication: October 2019 © cover photo: Tremeau/Fonds Français Muskoka ANALYSIS REPORT COMMUNITY HEALTH POLICIES AND PROGRAMMES ACRONYMS AC Care community agents (in French: Agents EBV Epstein-Barr virus communautaires - Sénégal) ECD Early Childhood Development ACPP Prevention and Promotion Community Actor (in French: Acteur Communautaire de Prévention et de Promotion EMTCT Elimination of mother-to-child transmission of VIH - Sénégal) FGM Female Genital Mutilation ACT Artemisinin-based combination therapy GAC Global Affairs Canada (ex-CIDA) ANC Antenatal Care HPV Human papilloma virus APP Agents for Promotion and Prevention (in French: iCCM integrated Community Case Management Agents pour la Promotion et la Prévention - Niger) IMCI Integrated Management of Childhood Illness ARI Acute Respiratory Infection IPTp Intermittent preventive treatment in pregnancy ASACO Community Health Organizations (Mali) KMC Kangaroo Mother Care ASBC Community-based health workers (in French : Agent de santé à base communautaire - Burkina Faso) LGA Local Government Area (Nigeria) BEPC First Secondary school diploma in francophone LLI(T)N Long-lasting insecticidal(-treated) nets education systems - 14/15 years old (in French: Brevet d’Etudes du Premier Cycle) LMIS Logistics management and information system CAC Community organization unit (in French: Cellule MAM Moderate acute malnutrition d’animation communautaire - DRC) M&E Monitoring and Evaluation CBC Community Birth Companion (The Gambia) MNP Micronutrient -
Report on the 'Think-In' on Community Health Worker Voice, Power, And
January 2018 Learning Exchange Report Number 3 Report on the ‘Think-in’ on Community Health Worker Voice, Power, and Citizens’ Right to Health Marta Schaaf Caitlin Warthin Amy Manning Stephanie Topp Report on the ‘Think-in’ on Community Health Worker Voice, Power, and Citizens’ Right to Health 1 About Accountability Research Center (ARC) The Accountability Research Center (ARC) is an action-research incubator based in the School of International Service at American University. ARC partners with civil society organizations and policy reformers in the global South to improve research and practice in the field of transparency, participation and accountability. For more information about ARC, please visit the website: www.accountabilityresearch.org. About ARC Publications ARC publications serve as a platform for accountability strategists and researchers to share their experiences and insights with diverse readers and potential allies across issue areas and sectors. These publications frame distinctive local and national initiatives in terms that engage with the broader debates in the transparency, participation and accountability (TPA) field. Research publications include brief Accountability Notes, longer Accountability Working Papers and Learning Exchange Reports. Rights and Permissions The material in this publication is copyrighted under the Creative Commons Attribution 4.0 Unported license (CC BY 4.0) https://creativecommons.org/licenses/by/4.0/. Under the Creative Commons Attribution license, you are free to copy, distribute, transmit, and adapt this work, including for commercial purposes, under the following conditions: Attribution—Please cite the work as follows: Schaaf, Marta, Caitlin Warthin, Amy Manning, and Stephanie Topp. 2018. “Report on the ‘Think-In’ on Community Health Worker Voice, Power, and Citizens’ Right to Health.” Accountability Research Center, Learning Exchange Report 3. -

Chapter 4: Downtown Arena
79 Chapter 4: Downtown Arena “an area in need of redevelopment…” During the week before Christmas 1998 several hundred residents of a small East Ward neighborhood received bright notices in their mailboxes from City Hall. The notices announced that a hearing would be held in two days to determine if a 40-acre region containing much of the neighborhood would be designated as an “area in need of redevelopment,” the modern and euphemistic term for what was once called “blighted.” Confused residents across the neighborhood read the notices and realized that the city intended to raze their houses and businesses. The telephone at the Sumei Multidisciplinary Arts Center rang constantly during the day and night as architect Hal Laessig and his wife Yoland Skeete answered questions from their neighbors about the implications of the notice. As one of the only community institutions in the neighborhood, the five-year old Sumei Center and its owners soon found themselves at the head of the local response to the city’s redevelopment plans. After the initial shock wore off, Laessig realized that the notices were the first step in the city’s campaign to acquire land to build the new basketball arena that the newspapers had been hinting for months would be coming to Newark.1 As more and more neighbors phoned Laessig to question the intent of the city notices, he decided to organize a community-wide meeting to discuss the options available to the newly targeted community. Hal Laessig has lived in Newark since 1976 working as an architect and designer after graduating from the New Jersey Institute of Technology. -

Conference Speakers Wednesday, October 30, 2019
CONFERENCE SPEAKERS WEDNESDAY, OCTOBER 30, 2019 9:00 AM WELCOME REMARKS Sancia Dalley, Senior Vice President, Strategic Partnerships & Director, RFK Compass Investor Program, Robert F. Kennedy Human Rights Sancia Dalley leads private sector engagement and business development, while leading the RFK Compass Investor Program, a network of 250 institutional investors and fund managers who are committed to seeking superior risk-adjusted returns while considering human rights and the “S” in ESG. Dalley has over fifteen years of experience in corporate social responsibility, philanthropy, public-private partnership building and management, and global affairs. Before joining Robert F. Kennedy Human Rights, she served under Ambassador Richard Holbrooke, the former US Ambassador to the United Nations, and Ray Chambers, the former United Nations Special Envoy on Health Financing, where she led private-sector partnerships and financing in Africa and Latin America. Concurrently, she served as the private sector liaison to the Roll Back Malaria Global Partnership, the Board of the Global Fund to Fight HIV, Tuberculosis and Malaria, and the Corporate Alliance on Malaria in Africa. Dalley earned her AB in international relations and French at Wesleyan College in Macon, Georgia. She is the founder of Redlake Global LLC, a boutique strategic philanthropy advisory group, and sits on the boards of Center for Active Design (CfAD) in New York and Boardwalk Village Foundation in Negril, Jamaica. 9:05 AM KEYNOTE FIRESIDE CHAT: A CONVERSATION WITH FIONA MA Fiona Ma, Treasurer, State of California Fiona Ma is California’s 34th State Treasurer. She was elected with more votes than any other candidate for treasurer in the state’s history, and is the first woman of color and the first woman certified public accountant (CPA) elected to the position.