Levonorgestrel Correlates with Less Weight Gain Than Other Progestins
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Attachment: Extract from Clinical Evaluation Bosentan
AusPAR Attachment 1 Extract from the Clinical Evaluation Report for Bosentan Proprietary Product Name: Tracleer Sponsor: Actelion Pharmaceuticals Australia Pty Ltd First round report: 25 October 2016 Second round report: 3 February 2017 Therapeutic Goods Administration About the Therapeutic Goods Administration (TGA) · The Therapeutic Goods Administration (TGA) is part of the Australian Government Department of Health, and is responsible for regulating medicines and medical devices. · The TGA administers the Therapeutic Goods Act 1989 (the Act), applying a risk management approach designed to ensure therapeutic goods supplied in Australia meet acceptable standards of quality, safety and efficacy (performance), when necessary. · The work of the TGA is based on applying scientific and clinical expertise to decision- making, to ensure that the benefits to consumers outweigh any risks associated with the use of medicines and medical devices. · The TGA relies on the public, healthcare professionals and industry to report problems with medicines or medical devices. TGA investigates reports received by it to determine any necessary regulatory action. · To report a problem with a medicine or medical device, please see the information on the TGA website <https://www.tga.gov.au>. About the Extract from the Clinical Evaluation Report · This document provides a more detailed evaluation of the clinical findings, extracted from the Clinical Evaluation Report (CER) prepared by the TGA. This extract does not include sections from the CER regarding product documentation or post market activities. · The words [Information redacted], where they appear in this document, indicate that confidential information has been deleted. · For the most recent Product Information (PI), please refer to the TGA website <https://www.tga.gov.au/product-information-pi>. -

LOKELMA Is Sodium Zirconium Cyclosilicate, a Potassium Binder
HIGHLIGHTS OF PRESCRIBING INFORMATION • For oral suspension: 10 g per packet (3) These highlights do not include all the information needed to use LOKELMA™ safely and effectively. See full prescribing information for ------------------------------ CONTRAINDICATIONS ---------------------------- LOKELMA™. None. (4) ----------------------- WARNINGS AND PRECAUTIONS --------------------- LOKELMA™ (sodium zirconium cyclosilicate) for oral suspension • Gastrointestinal Adverse Events in Patients with Motility Disorders. Initial U.S. Approval: [2018] (5.1) --------------------------- INDICATIONS AND USAGE ------------------------- • Edema. (5.2) LOKELMA is a potassium binder indicated for the treatment of hyperkalemia in adults. (1) ------------------------------ ADVERSE REACTIONS ---------------------------- Most common adverse reactions with LOKELMA: mild to moderate edema. Limitation of Use (6.1) LOKELMA should not be used as an emergency treatment for life-threatening hyperkalemia because of its delayed onset of action. (1) To report SUSPECTED ADVERSE REACTIONS, contact AstraZeneca at 1-800-236-9933 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. ---------------------- DOSAGE AND ADMINISTRATION --------------------- • Recommended starting dose is 10 g administered three times a day for ------------------------------ DRUG INTERACTIONS ---------------------------- up to 48 hours. (2.1) In general, other oral medications should be administered at least 2 hours • For maintenance treatment, recommended dose is 10 g once daily. (2.1) before -

NDA/BLA Multi-Disciplinary Review and Evaluation
NDA/BLA Multi-disciplinary Review and Evaluation NDA 214154 Nextstellis (drospirenone and estetrol tablets) NDA/BLA Multi-Disciplinary Review and Evaluation Application Type NDA Application Number(s) NDA 214154 (IND 110682) Priority or Standard Standard Submit Date(s) April 15, 2020 Received Date(s) April 15, 2020 PDUFA Goal Date April 15, 2021 Division/Office Division of Urology, Obstetrics, and Gynecology (DUOG) / Office of Rare Diseases, Pediatrics, Urologic and Reproductive Medicine (ORPURM) Review Completion Date April 15, 2021 Established/Proper Name drospirenone and estetrol tablets (Proposed) Trade Name Nextstellis Pharmacologic Class Combination hormonal contraceptive Applicant Mayne Pharma LLC Dosage form Tablet Applicant proposed Dosing x Take one tablet by mouth at the same time every day. Regimen x Take tablets in the order directed on the blister pack. Applicant Proposed For use by females of reproductive potential to prevent Indication(s)/Population(s) pregnancy Recommendation on Approval Regulatory Action Recommended For use by females of reproductive potential to prevent Indication(s)/Population(s) pregnancy (if applicable) Recommended Dosing x Take one pink tablet (drospirenone 3 mg, estetrol Regimen anhydrous 14.2 mg) by mouth at the same time every day for 24 days x Take one white inert tablet (placebo) by mouth at the same time every day for 4 days following the pink tablets x Take tablets in the order directed on the blister pack 1 Reference ID: 4778993 NDA/BLA Multi-disciplinary Review and Evaluation NDA 214154 Nextstellis (drospirenone and estetrol tablets) Table of Contents Table of Tables .................................................................................................................... 5 Table of Figures ................................................................................................................... 7 Reviewers of Multi-Disciplinary Review and Evaluation ................................................... -

The Novel Progesterone Receptor
0013-7227/99/$03.00/0 Vol. 140, No. 3 Endocrinology Printed in U.S.A. Copyright © 1999 by The Endocrine Society The Novel Progesterone Receptor Antagonists RTI 3021– 012 and RTI 3021–022 Exhibit Complex Glucocorticoid Receptor Antagonist Activities: Implications for the Development of Dissociated Antiprogestins* B. L. WAGNER†, G. POLLIO, P. GIANGRANDE‡, J. C. WEBSTER, M. BRESLIN, D. E. MAIS, C. E. COOK, W. V. VEDECKIS, J. A. CIDLOWSKI, AND D. P. MCDONNELL Department of Pharmacology and Cancer Biology (B.L.W., G.P., P.G., D.P.M.), Duke University Medical Center, Durham, North Carolina 27710; Molecular Endocrinology Group (J.C.W., J.A.C.), NIEHS, National Institutes of Health, Research Triangle Park, North Carolina 27709; Department of Biochemistry and Molecular Biology (M.B., W.V.V.), Louisiana State University Medical School, New Orleans, Louisiana 70112; Ligand Pharmaceuticals, Inc. (D.E.M.), San Diego, California 92121; Research Triangle Institute (C.E.C.), Chemistry and Life Sciences, Research Triangle Park, North Carolina 27709 ABSTRACT by agonists for DNA response elements within target gene promoters. We have identified two novel compounds (RTI 3021–012 and RTI Accordingly, we observed that RU486, RTI 3021–012, and RTI 3021– 3021–022) that demonstrate similar affinities for human progeste- 022, when assayed for PR antagonist activity, accomplished both of rone receptor (PR) and display equivalent antiprogestenic activity. As these steps. Thus, all three compounds are “active antagonists” of PR with most antiprogestins, such as RU486, RTI 3021–012, and RTI function. When assayed on GR, however, RU486 alone functioned as 3021–022 also bind to the glucocorticoid receptor (GR) with high an active antagonist. -

Glucocorticoid Withdrawal—An Overview on When and How to Diagnose Adrenal Insufficiency in Clinical Practice
diagnostics Review Glucocorticoid Withdrawal—An Overview on When and How to Diagnose Adrenal Insufficiency in Clinical Practice Katarzyna Pelewicz and Piotr Mi´skiewicz* Department of Internal Medicine and Endocrinology, Medical University of Warsaw, 02-091 Warsaw, Poland; [email protected] * Correspondence: [email protected]; Tel.: +48-225-992-877 Abstract: Glucocorticoids (GCs) are widely used due to their anti-inflammatory and immunosup- pressive effects. As many as 1–3% of the population are currently on GC treatment. Prolonged therapy with GCs is associated with an increased risk of GC-induced adrenal insufficiency (AI). AI is a rare and often underdiagnosed clinical condition characterized by deficient GC production by the adrenal cortex. AI can be life-threatening; therefore, it is essential to know how to diagnose and treat this disorder. Not only oral but also inhalation, topical, nasal, intra-articular and intravenous administration of GCs may lead to adrenal suppression. Moreover, recent studies have proven that short-term (<4 weeks), as well as low-dose (<5 mg prednisone equivalent per day) GC treatment can also suppress the hypothalamic–pituitary–adrenal axis. Chronic therapy with GCs is the most com- mon cause of AI. GC-induced AI remains challenging for clinicians in everyday patient care. Properly conducted GC withdrawal is crucial in preventing GC-induced AI; however, adrenal suppression may occur despite following recommended GC tapering regimens. A suspicion of GC-induced AI requires careful diagnostic workup and prompt introduction of a GC replacement treatment. The Citation: Pelewicz, K.; Mi´skiewicz,P. present review provides a summary of current knowledge on the management of GC-induced AI, Glucocorticoid Withdrawal—An including diagnostic methods, treatment schedules, and GC withdrawal regimens in adults. -

Hormones in Pregnancy
SYMPOSIUM Hormones in pregnancy Pratap Kumar, Navneet Magon1 Department of Obstetrics and Gynecology, Kasturba Medical College, Manipal University, Manipal, Karnataka, 1Air Force Hospital, Nathu Singh Road, Kanpur Cantt, Uttar Pradesh, India ABSTRACT The endocrinology of human pregnancy involves endocrine and metabolic changes that result from physiological alterations at the boundary between mother and fetus. Progesterone and oestrogen have a great role along with other hormones. The controversies of use of progestogen and others are discussed in this chapter. Progesterone has been shown to stimulate the secretion of Th2 and reduces the secretion of Th1 cytokines which maintains pregnancy. Supportive care in early pregnancy is associated with a significant beneficial effect on pregnancy outcome. Address for correspondence: Prophylactic hormonal supplementation can be recommended for all assisted reproduction Dr. Navneet Magon, techniques cycles. Preterm labor can be prevented by the use of progestogen. The route of Head, Department of Obstetrics administration plays an important role in the drug’s safety and efficacy profile in different and Gynecology, Air Force trimesters of pregnancy. Thyroid disorders have a great impact on pregnancy outcome and Hospital, Nathu Singh Road, needs to be monitored and treated accordingly. Method of locating review: Pubmed, scopus Kanpur Cantt, U.P. India. E‑ mail: [email protected] Key words: Oestrogen, hormones, progesterone, thyroid INTRODUCTION about 250 mg/day. Almost all of the progesterone produced by the placenta enters the placenta, contrast to oestrogen. Steroid hormones like progesterone have been extensively Progesterone production is independent of he precursor studied in the literature with controversies in early available, fetal status including the wellbeing. -

Efficacy and Safety of the Selective Glucocorticoid Receptor Modulator
Efficacy and Safety of the Selective Glucocorticoid Receptor Modulator, Relacorilant (up to 400 mg/day), in Patients With Endogenous Hypercortisolism: Results From an Open-Label Phase 2 Study Rosario Pivonello, MD, PhD1; Atil Y. Kargi, MD2; Noel Ellison, MS3; Andreas Moraitis, MD4; Massimo Terzolo, MD5 1Università Federico II di Napoli, Naples, Italy; 2University of Miami Miller School of Medicine, Miami, FL, USA; 3Trialwise, Inc, Houston, TX, USA; 4Corcept Therapeutics, Menlo Park, CA, USA; 5Internal Medicine 1 - San Luigi Gonzaga Hospital, University of Turin, Orbassano, Italy INTRODUCTION EFFICACY ANALYSES Table 5. Summary of Responder Analysis in Patients at Last SAFETY Relacorilant is a highly selective glucocorticoid receptor modulator under Key efficacy assessments were the evaluation of blood pressure in the Observation Table 7 shows frequency of TEAEs; all were categorized as ≤Grade 3 in hypertensive subgroup and glucose tolerance in the impaired glucose severity investigation for the treatment of all etiologies of endogenous Cushing Low-Dose Group High-Dose Group tolerance (IGT)/type 2 diabetes mellitus (T2DM) subgroup Five serious TEAEs were reported in 4 patients in the high-dose group syndrome (CS) Responder, n/N (%) Responder, n/N (%) o Relacorilant reduces the effects of cortisol, but unlike mifepristone, does o Response in hypertension defined as a decrease of ≥5 mmHg in either (pilonidal cyst, myopathy, polyneuropathy, myocardial infarction, and not bind to progesterone receptors (Table 1)1 mean systolic blood pressure (SBP) or diastolic blood pressure (DBP) from HTN 5/12 (41.67) 7/11 (63.64) hypertension) baseline No drug-induced cases of hypokalemia or abnormal vaginal bleeding were IGT/T2DM 2/13 (15.38) 6/12 (50.00) o Response in IGT/T2DM defined by one of the following: noted Table 1. -

Guideline for Preoperative Medication Management
Guideline: Preoperative Medication Management Guideline for Preoperative Medication Management Purpose of Guideline: To provide guidance to physicians, advanced practice providers (APPs), pharmacists, and nurses regarding medication management in the preoperative setting. Background: Appropriate perioperative medication management is essential to ensure positive surgical outcomes and prevent medication misadventures.1 Results from a prospective analysis of 1,025 patients admitted to a general surgical unit concluded that patients on at least one medication for a chronic disease are 2.7 times more likely to experience surgical complications compared with those not taking any medications. As the aging population requires more medication use and the availability of various nonprescription medications continues to increase, so does the risk of polypharmacy and the need for perioperative medication guidance.2 There are no well-designed trials to support evidence-based recommendations for perioperative medication management; however, general principles and best practice approaches are available. General considerations for perioperative medication management include a thorough medication history, understanding of the medication pharmacokinetics and potential for withdrawal symptoms, understanding the risks associated with the surgical procedure and the risks of medication discontinuation based on the intended indication. Clinical judgement must be exercised, especially if medication pharmacokinetics are not predictable or there are significant risks associated with inappropriate medication withdrawal (eg, tolerance) or continuation (eg, postsurgical infection).2 Clinical Assessment: Prior to instructing the patient on preoperative medication management, completion of a thorough medication history is recommended – including all information on prescription medications, over-the-counter medications, “as needed” medications, vitamins, supplements, and herbal medications. Allergies should also be verified and documented. -

Pharmacology/Therapeutics II Block III Lectures 2013-14
Pharmacology/Therapeutics II Block III Lectures 2013‐14 66. Hypothalamic/pituitary Hormones ‐ Rana 67. Estrogens and Progesterone I ‐ Rana 68. Estrogens and Progesterone II ‐ Rana 69. Androgens ‐ Rana 70. Thyroid/Anti‐Thyroid Drugs – Patel 71. Calcium Metabolism – Patel 72. Adrenocorticosterioids and Antagonists – Clipstone 73. Diabetes Drugs I – Clipstone 74. Diabetes Drugs II ‐ Clipstone Pharmacology & Therapeutics Neuroendocrine Pharmacology: Hypothalamic and Pituitary Hormones, March 20, 2014 Lecture Ajay Rana, Ph.D. Neuroendocrine Pharmacology: Hypothalamic and Pituitary Hormones Date: Thursday, March 20, 2014-8:30 AM Reading Assignment: Katzung, Chapter 37 Key Concepts and Learning Objectives To review the physiology of neuroendocrine regulation To discuss the use neuroendocrine agents for the treatment of representative neuroendocrine disorders: growth hormone deficiency/excess, infertility, hyperprolactinemia Drugs discussed Growth Hormone Deficiency: . Recombinant hGH . Synthetic GHRH, Recombinant IGF-1 Growth Hormone Excess: . Somatostatin analogue . GH receptor antagonist . Dopamine receptor agonist Infertility and other endocrine related disorders: . Human menopausal and recombinant gonadotropins . GnRH agonists as activators . GnRH agonists as inhibitors . GnRH receptor antagonists Hyperprolactinemia: . Dopamine receptor agonists 1 Pharmacology & Therapeutics Neuroendocrine Pharmacology: Hypothalamic and Pituitary Hormones, March 20, 2014 Lecture Ajay Rana, Ph.D. 1. Overview of Neuroendocrine Systems The neuroendocrine -

Glucocorticoid Induced Adrenal Insufficiency BMJ: First Published As 10.1136/Bmj.N1380 on 12 July 2021
STATE OF THE ART REVIEW Glucocorticoid induced adrenal insufficiency BMJ: first published as 10.1136/bmj.n1380 on 12 July 2021. Downloaded from Alessandro Prete,1 Irina Bancos2 ABSTRACT 1 Synthetic glucocorticoids are widely used for their anti-inflammatory and Institute of Metabolism and Systems Research, University of immunosuppressive actions. A possible unwanted effect of glucocorticoid treatment Birmingham, Birmingham, UK 2Division of Endocrinology, is suppression of the hypothalamic-pituitary-adrenal axis, which can lead to adrenal Metabolism and Nutrition, insufficiency. Factors affecting the risk of glucocorticoid induced adrenal insufficiency Department of Internal Medicine, Mayo Clinic, (GI-AI) include the duration of glucocorticoid therapy, mode of administration, Rochester, MN 55905, USA Correspondence to: I Bancos glucocorticoid dose and potency, concomitant drugs that interfere with [email protected] glucocorticoid metabolism, and individual susceptibility. Patients with exogenous (ORCID 0000-0001-9332-2524) Cite this as: BMJ 2021;374:n1380 glucocorticoid use may develop features of Cushing’s syndrome and, subsequently, http://dx.doi.org/10.1136/bmj.n1380 glucocorticoid withdrawal syndrome when the treatment is tapered down. Symptoms Series explanation: State of the Art Reviews are commissioned of glucocorticoid withdrawal can overlap with those of the underlying disorder, as on the basis of their relevance to academics and specialists well as of GI-AI. A careful approach to the glucocorticoid taper and appropriate in the US and internationally. patient counseling are needed to assure a successful taper. Glucocorticoid therapy For this reason they are written predominantly by US authors. should not be completely stopped until recovery of adrenal function is achieved. In this review, we discuss the factors affecting the risk of GI-AI, propose a regimen for the glucocorticoid taper, and make suggestions for assessment of adrenal function recovery. -

6. References
176 IARC MONOGRAPHS VOLUME 91 6. References Adam, S.A., Sheaves, J.K., Wright, N.H., Mosser, G., Harris, R.W. & Vessey, M.P. (1981) A case– control study of the possible association between oral contraceptives and malignant mela- noma. Br. J. Cancer, 44, 45–50 Adami, H.-O., Bergström, R., Persson, I. & Sparén, P. (1990) The incidence of ovarian cancer in Sweden, 1960–1984. Am. J. Epidemiol., 132, 446–452 Ahmad, M.E., Shadab, G.G.H.A., Azfer, M.A. & Afzal, M. (2001) Evaluation of genotoxic poten- tial of synthetic progestins norethindrone and norgestrel in human lymphocytes in vitro. Mutat. Res., 494, 13–20 Ali, M.M. & Cleland, J. (2005) Sexual and reproductive behaviour among single women aged 15–24 in eight Latin American countries: A comparative analysis. Soc. Sci. Med., 60, 1175–1185 Althuis, M.D., Brogan, D.R., Coates, R.J., Daling, J.R., Gammon, M.D., Malone, K.E., Schoenberg, J.B. & Brinton, L.A. (2003) Hormonal content and potency of oral contraceptives and breast cancer risk among young women. Br. J. Cancer, 88, 50–57 Arai, N., Ström, A., Rafter, J.J. & Gustafsson, J.-A. (2000) Estrogen receptor beta mRNA in colon cancer cells: Growth effects of estrogen and genistein. Biochem. biophys. Res. Commun., 270, 425–431 Arbeit, J.M., Münger, K., Howley, P.M. & Hanahan, D. (1994) Progressive squamous epithelial neoplasia in K14-human papillomavirus type 16 transgenic mice. J. Virol., 68, 4358–4368 Arbeit, J.M., Howley, P.M. & Hanahan, D. (1996) Chronic estrogen-induced cervical and vaginal squamous carcinogenesis in human papillomavirus type 16 transgenic mice. -
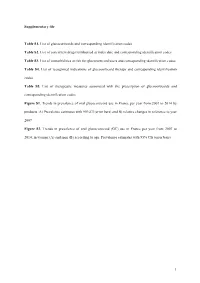
Supplementary File Table S1. List of Glucocorticoids and Corresponding
Supplementary file Table S1. List of glucocorticoids and corresponding identification codes Table S2. List of concurrent drugs reimbursed at index date and corresponding identification codes Table S3. List of comorbidities at risk for glucocorticoid users and corresponding identification codes Table S4. List of recognized indications of glucocorticoid therapy and corresponding identification codes Table S5. List of therapeutic measures associated with the prescription of glucocorticoids and corresponding identification codes Figure S1. Trends in prevalence of oral glucocorticoid use in France per year from 2007 to 2014 by products. A) Prevalence estimates with 95%CI (error bars) and B) relative changes in reference to year 2007 Figure S2. Trends in prevalence of oral glucocorticoid (GC) use in France per year from 2007 to 2014, in women (A) and men (B) according to age. Prevalence estimates with 95% CIs (error bars) 1 Table S1. List of glucocorticoids and corresponding identification codes Glucocorticoids Source Code Betamethasone Drug reimbursement (ATC) H02AB01 Dexamethasone Drug reimbursement (ATC) H02AB02 Methylprednisolone Drug reimbursement (ATC) H02AB04 Prednisolone Drug reimbursement (ATC) H02AB06 Prednisone Drug reimbursement (ATC) H02AB07 ATC: Anatomical Therapeutic Chemical classification system Table S2. List of concurrent drugs reimbursed at index date and corresponding identification codes Concurrent drugs at index date Source Code Analgesics Drug reimbursement (ATC) N02 Antibiotics Drug reimbursement (ATC) J01 Anti-inflammatory