An Empirical Antigen Selection Method Identifies Neoantigens That Either Elicit Broad Antitumor T-Cell Responses Or Drive Tumor Growth
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-
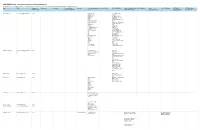
2020-2021 Cancer Communications Committee Disclosures All Relationships Are Considered Compensated
2020-2021 Cancer Communications Committee Disclosures All relationships are considered compensated. Relationships are self-held unless otherwise noted. I = Immediate Family Member, Inst = My Institution Name EMAIL Committee Employment Leadership Stock and Other Honoraria Consulting or Advisory Speakers' Bureau Research Funding Patents, Royalties, Other Expert Testimony Travel, Other Relationship (OPTIONAL) (OPTIONAL) Open Member Status Ownership Interests Role Intellectual Property Accommodations, Uncompensated Payments Link Expenses Relationships Neeraj Agarwal [email protected] Active Astellas Pharma Active Biotech (Inst) Astellas Pharma Amgen (Inst) AstraZeneca AstraZeneca (Inst) AstraZeneca Bavarian Nordic (Inst) AVEO Bayer (Inst) Bayer BN ImmunoTherapeutics Bristol-Myers Squibb (Inst) Calithera Biosciences Bristol-Myers Squibb (Inst) Eisai Calithera Biosciences EMD Serono (Inst) Exelixis Celldex (Inst) Foundation Medicine Eisai (Inst) Foundation One Inc Exelixis (Inst) Genentech Genentech (Inst) Janssen Oncology GlaxoSmithKline (Inst) Lilly Immunomedics (Inst) Lilly Janssen (Inst) lily Merck (Inst) Medivation/Astellas Newlink Genetics (Inst) MEI Pharma Novartis (Inst) Merck Pfizer (Inst) Nektar Prometheus (Inst) Novartis Rexahn Pharmaceuticals Pfizer (Inst) Pfizer Sanofi (Inst) Pharmacyclics Takeda (Inst) Seattle Genetics TRACON Pharma (Inst) Muhammad S. Beg muhammad.beg@utsouthwestern. Active Array BioPharma Agios (Inst) edu AstraZeneca/MedImmune ArQule (Inst) Cancer Commons AstraZeneca/MedImmune Ipsen (Inst) Legend Biotech -

Companies in Attendance
COMPANIES IN ATTENDANCE Abbott Diabetes Care Archbow Consulting LLC Business One Technologies Abbott Laboratories ARKRAY USA BusinessOneTech AbbVie Armory Hill Advocates, LLC CastiaRX ACADIA Artia Solutions Catalyst Acaria Health Asembia Celgene Accredo Assertio Therapeutics Celltrion Acer Therapeutics AssistRx Center for Creative Leadership Acorda Therapeutics Astellas Pharma US Inc. Cigna Actelion AstraZeneca Cigna Specialty Pharmacy AdhereTech Athenex Oncology Circassia Advantage Point Solutions Avanir Coeus Consulting Group Aerie Pharmaceuticals Avella Coherus Biosciences AGIOS AveXis Collaborative Associates LLC Aimmune Theraputics Bank of America Collegium Akcea Therapeutics Bausch Health Corsica Life Sciences Akebia Therapeutics Bayer U.S. CoverMyMeds Alder BioPharmaceuticals Becton Dickinson Creehan & Company, Inc., an Inovalon Company Alexion Biofrontera CSL Behring Alkermes Biogen Curant Health Allergan Biohaven CVS Health Almirall BioMarin D2 Consulting Alnylam BioMatrix Specialty Pharmacy Daiichi Sankyo Amarin BioPlus Specialty Pharmacy DBV Technologies Amber Pharmacy Bioventus Deloitte Consulting LLP AmerisourceBergen Blue Cross Blue Shield Association Dendreon Amgen Blue Fin Group Dermira Amicus Therapeutics bluebird bio Dexcom Amneal Boehringer Ingelheim Diplomat Pharmacy Anthem Boston Biomedical Dova Applied Policy Bowler and Company Decision Resources Group Aquestive Therapeutics Braeburn Eisai Arbor Pharmaceuticals Bristol-Myers Squibb 1 electroCore Indivior Merz Pharmaceuticals EMD Serono Inside Rx Milliman Encore Dermatology, -

Cabozantinib
Cabozantinib EXELIXIS, INC. 2011 ANNUAL REPORT Cabozantinib a potent, first-in-class, tyrosine kinase inhibitor that simultaneously targets the MET and V EGF signaling pathways. In clinical studies, cabozantinib has demonstrated a unique spectrum of anti-tumor activity in 12 out of 13 tumor types tested, with regression of metastatic or primary tumor lesions in so t sue, v ceral organs and the brain, and resolution of bone lesions on bone scan. we initiated the fi rst of two planned pivotal trials in metastatic castration-resistant prostate cancer (CRPC) and executed an agreement with the National Cancer Institute to broadly explore tumor indications outside of MTC and CRPC. LOOKING TOWARD APPROVAL One high point of 2011 was the positive outcome of the cabozantinib pivotal phase 3 clinical trial in MTC – the fi rst time we’ve generated pivotal data for one of our compounds. With a nearly three-fold Michael M. Morrissey, Ph.D. increase in progression-free survival over placebo, the data clearly demonstrate that cabozantinib provides a substantial benefi t to MTC patients. These data offer hard evidence that cabozantinib is a potent anti- TO OUR STOCKHOLDERS cancer agent with the ability to signifi cantly improve outcomes in a patient population that has few options and represents a signifi cant unmet medical need. IF I SUM UP 2011 FOR EXELIXIS IN A SINGLE WORD, Although MTC is not a major commercial opportunity, IT IS “CLARITY” — OF OPPORTUNITY, DIRECTION, pursuing the indication has given us the ability to move AND PURPOSE. It was a year in which the unique forward with a New Drug Application (NDA) in MTC, activity profi le and broad commercial potential of providing a solid foundation upon which to build a cabozantinib became clear, and our fi rst potential franchise in prostate cancer and other tumor types. -

Innovations and Patent Trends in the Development of USFDA Approved Protein Kinase Inhibitors in the Last Two Decades
pharmaceuticals Review Innovations and Patent Trends in the Development of USFDA Approved Protein Kinase Inhibitors in the Last Two Decades Mohd. Imran 1,* , Syed Mohammed Basheeruddin Asdaq 2,* , Shah Alam Khan 3 , Dhanalekshmi Unnikrishnan Meenakshi 3, Abdulhakeem S. Alamri 4,5 , Walaa F. Alsanie 4,5, Majid Alhomrani 4,5, Yahya Mohzari 6, Ahmed Alrashed 7, Mohammed AlMotairi 8, Eman H. Alkhaldi 9, Abeer K. Alorabi 10, Ahmed Subeh Alshrari 11, Mohammad Tauseef 12, Abida 1 , Saleh I. Alaqel 1, Ozair Alam 13 and Md. Afroz Bakht 14 1 Department of Pharmaceutical Chemistry, Faculty of Pharmacy, Northern Border University, Arar 91911, Saudi Arabia; [email protected] (A.); [email protected] (S.I.A.) 2 Department of Pharmacy Practice, College of Pharmacy, AlMaarefa University, Dariyah, Riyadh 13713, Saudi Arabia 3 College of Pharmacy, National University of Science and Technology, Muscat 130, Oman; [email protected] (S.A.K.); [email protected] (D.U.M.) 4 Department of Clinical Laboratory Sciences, The Faculty of Applied Medical Sciences, Taif University, Taif 21944, Saudi Arabia; [email protected] (A.S.A.); [email protected] (W.F.A.); [email protected] (M.A.) 5 Centre of Biomedical Sciences Research (CBSR), Deanship of Scientific Research, Taif University, Taif 21944, Saudi Arabia Citation: Imran, M.; Asdaq, S.M.B.; 6 Clinical Pharmacy Department, King Saud Medical City, Riyadh 12746, Saudi Arabia; [email protected] 7 Khan, S.A.; Unnikrishnan Meenakshi, Pharmaceutical Services Administration, Inpatient Department, Main Hospital, King Fahad Medical City, D.; Alamri, A.S.; Alsanie, W.F.; Riyadh 11564, Saudi Arabia; [email protected] 8 Department of Clinical Pharmacy, King Fahad Medical City, Riyadh 11564, Saudi Arabia; Alhomrani, M.; Mohzari, Y.; Alrashed, [email protected] A.; AlMotairi, M.; et al. -

Drug Companies Participating in MED-Project Stewardship Plan (February 9, 2017)
Drug Companies Participating in MED-Project Stewardship Plan (February 9, 2017) Participating Drug Company Parent Drug Company 3M Corporation 3M Corporation 3M Critical and Chronic Care 3M Corporation 3M Drug Delivery Systems 3M Corporation 3M Infection Prevention 3M Corporation 3M Oral Care 3M Corporation AbbVie Inc. AbbVie Inc. ACADIA Pharmaceuticals Inc. ACADIA Pharmaceuticals Inc. Accord Healthcare Inc. Accord Healthcare Inc. Acorda Therapeutics, Inc. Acorda Therapeutics, Inc. Acorda Therapeutics, Inc. Acorda Therapeutics, Inc. Actavis Generics Teva Pharmaceuticals USA, Inc. Actavis Pharma, Inc. (only for labeler code 52544) Allergan, Inc. Actelion Pharmaceuticals US, Inc. Actelion Pharmaceuticals US, Inc. Advanced Vision Research Inc. d.b.a. Akorn Consumer Health Akorn, Inc. Aegerion Pharmaceuticals, Inc. Aegerion Pharmaceuticals, Inc. Afaxys Inc. Afaxys Inc. Afaxys Pharmaceuticals (a division of Afaxys Inc.) Afaxys Inc. Affordable Pharmaceuticals LLC Braintree Laboratories Inc. Akorn Animal Health, Inc. Akorn, Inc. Akorn, Inc. Akorn, Inc. Akrimax Pharmaceuticals, LLC Akrimax Pharmaceuticals, LLC AKRON COATING & ADHESIVES AKRON COATING & ADHESIVES Alcon Laboratories, Inc. Novartis Group Companies Allergan Sales LLC Allergan, Inc. Allergan USA, Inc. Allergan, Inc. Allergan, Inc. Allergan, Inc. Alva-Amco Pharmacal Companies, Inc. Alva-Amco Pharmacal Companies, Inc. AMAG Pharma USA, Inc. AMAG Pharmaceuticals, Inc. AMAG Pharmaceuticals, Inc. AMAG Pharmaceuticals, Inc. Amarin Corp Amarin Pharma, Inc. Amarin Corp. PLC Amarin Pharma, Inc. Amarin Pharma, Inc. Amarin Pharma, Inc. Amarin Pharmaceuticals Ireland Ltd. Amarin Pharma, Inc. American Regent, Inc. Daiichi Sankyo, Inc. Amerisource Health Services Corporation DBA: American Health Amerisource Health Services Corporation DBA: American Health Packaging Packaging Amgen Inc. Amgen Inc. Amgen USA Amgen Inc. Amneal Pharmaceuticals LLC Amneal Pharmaceuticals LLC Anchen Pharmaceuticals, Inc. -
MED-Project Participating Drug Companies - King County Washington, March 2020
MED-Project Participating Drug Companies - King County Washington, March 2020 Drug Company Name Parent Company 3M Corporation 3M Corporation 3M Drug Delivery Systems 3M Corporation 3M ESPE 3M Corporation 3M Health Care 3M Corporation 3M Personal Care 3M Corporation AbbVie Inc. AbbVie Inc. ACADIA Pharmaceuticals Inc. ACADIA Pharmaceuticals Inc. Accord Healthcare Inc. Accord Healthcare Inc. Acorda Therapeutics, Inc. Acorda Therapeutics, Inc. Acorda Therapeutics, Inc. Acorda Therapeutics, Inc. Actavis Generics Teva Pharmaceuticals USA, Inc. Actavis Pharma, Inc. (only for labeler code 52544) Allergan, Inc. Actelion Johnson & Johnson Adapt Pharma Inc. Adapt Pharma Inc. Advanced Vision Research Inc. d.b.a. Akorn Consumer Health Akorn, Inc. Advantice Health Advantice Health Aegerion Pharmaceuticals, Inc. Aegerion Pharmaceuticals, Inc. Afaxys Inc. Afaxys Inc. Afaxys Pharmaceuticals (a division of Afaxys Inc.) Afaxys Inc. Affordable Pharmaceuticals LLC Sebela Pharmaceuticals Inc. Ajanta Pharma USA Inc. Ajanta Pharma USA Inc. AkaRx, Inc., dba Dova Pharmaceuticals AkaRx, Inc., dba Dova Pharmaceuticals Akebia Therapeutics, Inc. Akebia Therapeutics, Inc. Akorn Animal Health, Inc. Akorn, Inc. Akorn, Inc. Akorn, Inc. Akrimax Pharmaceuticals, LLC Akrimax Pharmaceuticals, LLC AKRON COATING & ADHESIVES AKRON COATING & ADHESIVES Alaven Pharmaceuticals LLC Mylan Inc. Alcon Laboratories, Inc. Novartis Group Companies Alembic Pharmaceuticals Inc. Alembic Pharmaceuticals Inc. Allergan Sales, LLC Allergan, Inc. Allergan USA, Inc. Allergan, Inc. Allergan, Inc. Allergan, Inc. Almaject, Inc. Alvogen Pharma US, Inc. Almatica Pharma, Inc. Alvogen Pharma US, Inc. Almirall LLC Almirall LLC Alphapharm Pty Ltd Mylan Inc. Alva-Amco Pharmacal Companies, Inc. Alva-Amco Pharmacal Companies, Inc. Alvogen Pharma US, Inc. Alvogen Pharma US, Inc. Alvogen, Inc. Alvogen Pharma US, Inc. AMAG Pharma USA, Inc. -
Annual Report John Hancock Multifactor Etfs ETF
Annual report John Hancock Multifactor ETFs ETF April 30, 2021 A message to shareholders Dear shareholder, The global equity markets were propelled to strong gains for the 12 months ended April 30, 2021. The U.S. Federal Reserve and other world central banks maintained their policies of ultra-low short-term interest rates. With little in the way of yield available on safer assets, investors gravitated toward equities in search of more attractive total returns. The approval and subsequent rollout of multiple COVID-19 vaccines also boosted investor sentiment by providing a clearer path for economic conditions to return to normal in 2021. The passing of fiscal stimulus packages in the United States was an additional source of support for the markets. In combination, these developments helped the major stock indexes gradually recapture, and ultimately exceed, the levels at which they stood prior to the global outbreak of the coronavirus in early 2020. Despite the overall good news, there are still obstacles. Some economies may have reopened too early, the pace of vaccinations varies widely from country to country, and many industries will take time to recover from the losses suffered. In these uncertain times, your financial professional can assist with positioning your portfolio so that it’s sufficiently diversified to help meet your long-term objectives and to withstand the inevitable bouts of market volatility along the way. On behalf of everyone at John Hancock Investment Management, I’d like to take this opportunity to welcome new shareholders and thank existing shareholders for the continued trust you’ve placed in us. -

Resilient Together
Annual Report 2018 Resilient Together 2018 Highlights 480+ employees united in our mission to help cancer patients recover stronger and live longer, a 30 percent increase in headcount versus year-end 2017 3 new pivotal trials of cabozantinib initiated, with additional pivotal trial starts anticipated in 2019 4millions profitable quarters, resulting in the company's second consecutive full year of profitability on an operating basis #1 CABOMETYX® (cabozantinib) became the #1newly prescribed TKI to treat advanced RCC "Our discovery, development, and commercialization teams are working seamlessly to advance our mission to help patients with cancer.” Letter to our stockholders Letter to Stockholders Exelixis started and finished 2018 in A Solid Commercial Foundation two very different places – literally Since the FDA first approved and figuratively. We began the year CABOMETYX in the U.S. in 2016, the in South San Francisco, California at Exelixis commercial team has leveraged the site our company had called strong data and a tireless, collaborative home for nearly two decades. We work ethic to make it the preferred finished 2018 in the nearby city of tyrosine kinase inhibitor (TKI) to treat Alameda in new headquarters advanced renal cell carcinoma (RCC), the 1 designed from scratch just for most common form of kidney cancer. Exelixis, with ample room to grow In fact, by the end of 2018, CABOMETYX had become the number one newly and new state-of-the-art onsite prescribed TKI for advanced RCC, discovery laboratories. capturing 34 percent market share for this therapy class.2 In the fourth quarter 1000 These two facilities are only about ten $851.6 of 2018 specifically, this included miles apart across the San Francisco 800 approximately 90 percent of patients Bay, but the distance feels greater when whose disease had progressed following 600 you consider what the move means for $479.6 $457.2 immune checkpoint inhibitor (ICI) our company. -

UNITED STATES SECURITIES and EXCHANGE COMMISSION Washington, D.C
Table of Contents As filed with the Securities and Exchange Commission on September 26, 2008 Registration No. 333-152166 UNITED STATES SECURITIES AND EXCHANGE COMMISSION Washington, D.C. 20549 Amendment No. 1 to FORM S-1 REGISTRATION STATEMENT UNDER THE SECURITIES ACT OF 1933 EXELIXIS, INC. (Exact name of registrant as specified in its charter) Delaware 8731 04-3257395 (State or other jurisdiction of (Primary Standard Industrial (I.R.S. Employer incorporation or organization) Classification Code Number) Identification No.) 249 East Grand Ave. P.O. Box 511 South San Francisco, CA 94083-0511 (650) 837-7000 (Address, including zip code, and telephone number, including area code, of registrant’s principal executive offices) George A. Scangos, Ph.D. President and Chief Executive Officer Exelixis, Inc. 249 East Grand Ave. P.O. Box 511 South San Francisco, CA 94083-0511 (650) 837-7000 (Name, address, including zip code, and telephone number, including area code, of agent for service) Copy to: Suzanne Sawochka Hooper, Esq. Cooley Godward Kronish LLP Five Palo Alto Square 3000 El Camino Real Palo Alto, CA 94306-2155 (650) 843-5000 Approximate date of commencement of proposed sale to the public: From time to time after the effective date of this Registration Statement. If any of the securities being registered on this Form are to be offered on a delayed or continuous basis pursuant to Rule 415 under the Securities Act of 1933 check the following box. x If this Form is filed to register additional securities for an offering pursuant to Rule 462(b) under the Securities Act, please check the following box and list the Securities Act registration statement number of the earlier effective registration statement for the same offering. -

20200915 MED-Project Participant List.Xlsx
Pierce County MED-Project Stewardship Plan Participants (August 13, 2021) Parent Company Name Company Name 3M Corporation 3M Corporation 3M Corporation 3M ESPE Dental Products 3M Corporation 3M Health Care AbbVie Inc. AbbVie Inc. AbbVie Inc. Allergan USA, Inc. AbbVie Inc. Pharmacyclics, subsidiary of AbbVie Inc. ACADIA Pharmaceuticals Inc. ACADIA Pharmaceuticals Inc. Accord Healthcare Inc. Accord Healthcare Inc. Accord Healthcare Inc. Accord Biopharma Acorda Therapeutics, Inc. Acorda Therapeutics, Inc. Adapt Pharma Inc. Adapt Pharma Inc. Advantice Health Advantice Health Advanz Pharma Group Advanz Pharma Group Afaxys Inc. Afaxys Inc. Afaxys Inc. Afaxys Pharmaceuticals (a division of Afaxys Inc.) Ajanta Pharma USA Inc. Ajanta Pharma USA Inc. AkaRx, Inc., dba Dova Pharmaceuticals AkaRx, Inc., dba Dova Pharmaceuticals AkaRx, Inc., dba Dova Pharmaceuticals Dova Pharmaceuticals Akebia Therapeutics, Inc. Akebia Therapeutics, Inc. Akebia Therapeutics, Inc. Keryx Biopharmaceuticals, Inc. Akorn Operating Company, LLC Akorn Operating Company, LLC Akorn Operating Company, LLC Advanced Vision Research Inc. d.b.a. Akorn Consumer Health Akorn Operating Company, LLC Akorn Animal Health, Inc. Akorn Operating Company, LLC Clover Pharmaceuticals Corp. Akorn Operating Company, LLC Hi-Tech Pharmacal Co., Inc. Akorn Operating Company, LLC Oak Pharmaceuticals, Inc. Akorn Operating Company, LLC Versapharm, Incorporated Alembic Pharmaceuticals Inc. Alembic Pharmaceuticals Inc. Alfasigma USA, Inc. Alfasigma USA, Inc. Allergan, Inc. Allergan, Inc. Allergan, Inc. Allergan Sales, LLC Allergan, Inc. Aptalis Pharma US, Inc. Allergan, Inc. Durata Therapeutics US Limited Allergan, Inc. Pacific Pharma, Inc. Allergan, Inc. Warner Chilcott (US), LLC Almirall LLC Almirall LLC Alva-Amco Pharmacal Companies, Inc. Alva-Amco Pharmacal Companies, Inc. Alvogen Pharma US, Inc. Alvogen Pharma US, Inc. -

Downloads/Cometriq Full Prescribing Information.Pdf
Table of Contents UNITED STATES SECURITIES AND EXCHANGE COMMISSION Washington, D.C. 20549 FORM 10-Q ☒ QUARTERLY REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 For the quarterly period ended April 2, 2021 or ☐ TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 Commission File Number: 000-30235 EXELIXIS, INC. (Exact name of registrant as specified in its charter) Delaware 04-3257395 (State or other jurisdiction of incorporation or organization) (I.R.S. Employer Identification Number) 1851 Harbor Bay Parkway Alameda, CA 94502 (650) 837-7000 (Address, including zip code, and telephone number, including area code, of registrant’s principal executive offices) Securities registered pursuant to Section 12(b) of the Act: Title of each class Trading Symbol(s) Name of each exchange on which registered Common Stock $.001 Par Value per Share EXEL The Nasdaq Stock Market LLC Indicate by check mark whether the registrant: (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days). Yes ☒ No ☐ Indicate by check mark whether the registrant has submitted electronically every Interactive Data File required to be submitted pursuant to Rule 405 of Regulation S-T during the preceding 12 months (or for such shorter period that the registrant was required to submit such files). -

Biogen Inc. 2020 Annual Report
Annual Report Biogen ANNUAL REPORT 2020 ® CONTAINS SOYOIL 2020 HIGHLIGHTS Total Revenue Product Revenue ($ in millions) ($ in millions and % of total product revenue) 2020 $13,445 $3,905 36.5% Fumarate 5 2020 $13,445 $4,438 39.0% 2019 $14,378 $1,878 17.6% 2019 $14,378 Interferon 6 2018 $13,453 $2,102 18.5% 2018 $1,946 18.2% 2017 $12,274$13,453 TYSABRI 2017 $12,274 $1,892 16.6% 2017 2016 $11,449$12,274 $2,052 19.2% 2016 $11,449 SPINRAZA 2016 $11,449 $2,097 18.4% $911 8.5% Other 7 GAAP Diluted EPS ⁄ Non-GAAP Diluted EPS 1 $851 7.5% 2020 $24.80 ∕ $33.70 2 2020 2020 $24.80 ∕ $33.70 2 2019 $31.42 ∕ $33.57 2019 2019 $31.42 ∕ $33.57 2018 $21.58 3 ∕ $27.44 2 2018 $21.58 3 ∕ $27.44 2 2017 $11.92 3 ∕ $22.72 2 2017 $11.92 3 ∕ $22.72 2 2016 $16.93 ∕ $20.22 2016 $16.93 ∕ $20.22 Free cash flow1,4 Product Revenue by Region ($2020 in millions) $3,805 (% of total product revenue) 2020 $3,805 2019 $6,564 2020 2019 2018 2019 $6,564 2018 $5,417 2018 $5,417 % % % 2017 $3,684 55 59 63 2017 $3,684 % % % 2016 $3,906 45 41 37 2016 $3,906 U.S. Rest of the world 1 Non-GAAP diluted earnings per share (EPS) and free cash flow are Non-GAAP financial measures. A reconciliation of GAAP to FOSSIL 1st Fortune 500 company to Non-GAAP diluted EPS and free cash flow amounts is set forth on FUEL FREE commit to going fossil fuel free pages 10–13 of this Annual Report.